Lots of interesting abstracts and cases were submitted for TCTAP 2025. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-036
Comparison of Clinical Outcomes Between First-and Second-Generation Drug-Eluting Stents in Elderly Patients: 10-Year Follow-Up Results
By Seung-Woon Rha, Manda Satria Chesario, Byoung Geol Choi, Se Yeon Choi, Jae Kyeong Byun, Jinah Cha, Woo Jin Ahn, Wonsang Chu, Soohyung Park, Cheol Ung Choi, Chang Gyu Park
Presenter
Manda Satria Chesario
Authors
Seung-Woon Rha1, Manda Satria Chesario2, Byoung Geol Choi3, Se Yeon Choi1, Jae Kyeong Byun1, Jinah Cha1, Woo Jin Ahn4, Wonsang Chu1, Soohyung Park1, Cheol Ung Choi1, Chang Gyu Park1
Affiliation
Korea University Guro Hospital, Korea (Republic of)1, Korea University Guro Hospital, Indonesia2, Honam University, Korea (Republic of)3, National Emergency Medical Center, Korea (Republic of)4
View Study Report
TCTAP A-036
DES/BRS/DCB
Comparison of Clinical Outcomes Between First-and Second-Generation Drug-Eluting Stents in Elderly Patients: 10-Year Follow-Up Results
Seung-Woon Rha1, Manda Satria Chesario2, Byoung Geol Choi3, Se Yeon Choi1, Jae Kyeong Byun1, Jinah Cha1, Woo Jin Ahn4, Wonsang Chu1, Soohyung Park1, Cheol Ung Choi1, Chang Gyu Park1
Korea University Guro Hospital, Korea (Republic of)1, Korea University Guro Hospital, Indonesia2, Honam University, Korea (Republic of)3, National Emergency Medical Center, Korea (Republic of)4
Background
The second-generation (2G)drug-eluting stents (DES) have been used to Coronary Artery Disease. There are very limited long-term clinical outcomedata comparing first-generation (1G) versus 2G-DES in Elderly (≥65 years of age) patients undergoing percutaneouscoronary intervention (PCI). The study aimed to compare the efficacy and safety 2G-DESwith 1G-DES in Elderly patients who underwent PCI during 10-year clinicalfollow-up periods.
Methods
The outcomes of 1,280consecutive Elderly patients who underwent PCI with with 1G-DES(paclitaxel-, sirolimus-eluting stent, n=561) or 2G-DES (zotarolimus [endeavor,endeavor resolute]- or everolimus-eluting stent [promus element, xience], n=719)were enrolled. The study endpoints were individual and composite clinicaloutcomes up to ten-year. After PSM, two propensity-matched (PSM) groups (345pairs) were generated.
Results
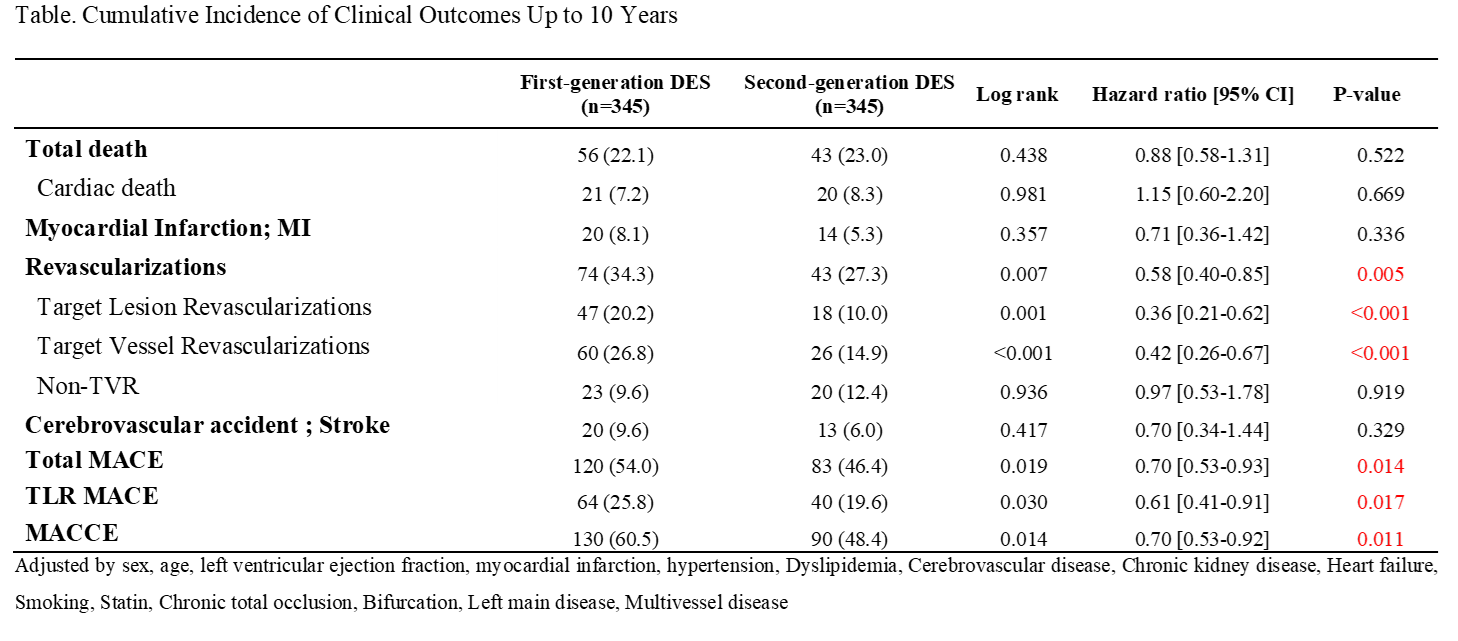
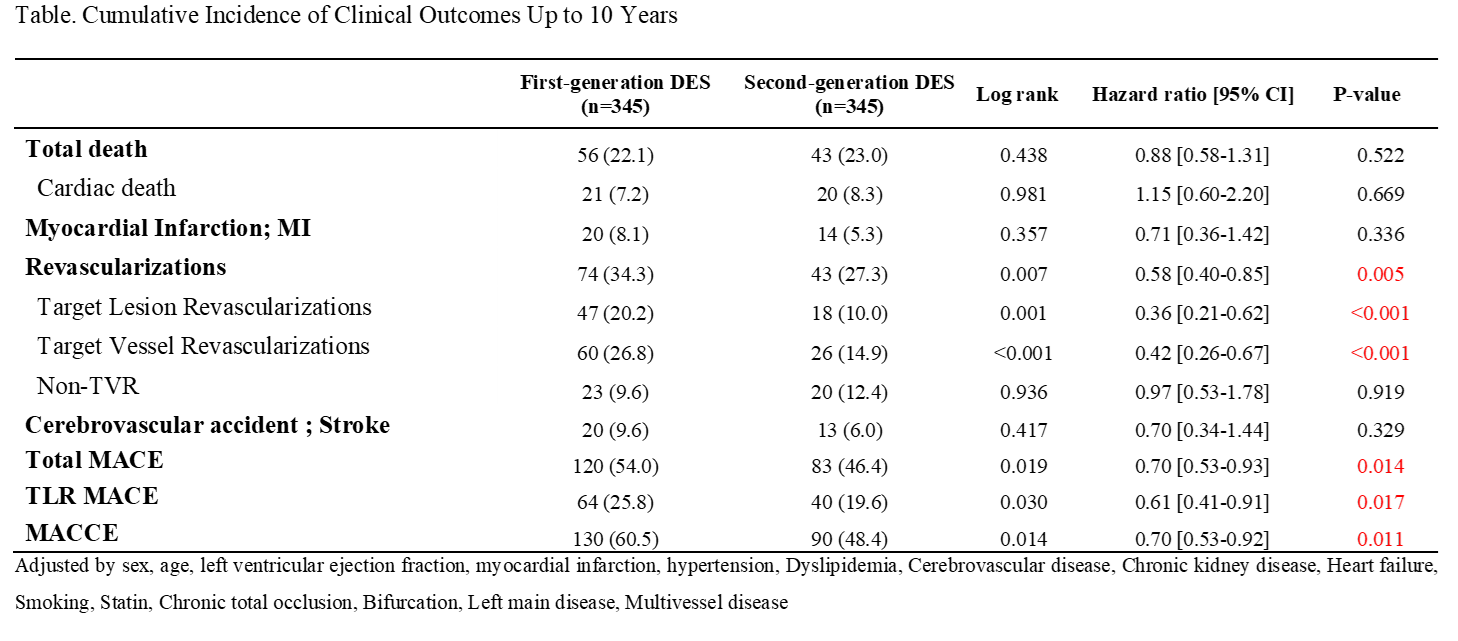
During the 10-year follow-up period, the 2G-DES grouphad a lower incidence of any revascularization (hazard ratio [HR], 0.58; 95% confidenceinterval [CI], 0.40 – 0.85; p=0.005), target lesion revascularization (TLR; HR,0.36; 95% CI, 0.21 – 0.62; p<0.001), target vessel revascularization (TVR; HR,0.42; 95% CI, 0.26 – 0.67; p<0.001), total major adverse cardiac events (MACE;HR, 0.70; 95% CI, 0.53 – 0.93; p = 0.014), TLR MACE (HR, 0.61; 95% CI, 0.41 –0.91; p=0.017) and MACCE (HR, 0.70; 95% CI, 0.53 – 0.92; p = 0.011, table). However, the cumulative incidence of totaldeath, cardiac death, MI, non-TVR and cerebrovascular disease were similarbetween the two groups (Table).
Conclusion
In our single-center, all-comer registry, 1G-DEShad comparable efficacy compared with 2G-DES in Elderly patients except lowerincidence of TLR, TVR, MACE and TLR MACE in 2G-DES during 10-year follow-upperiods