Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-154
Successful Management of Dislodged Left Main Stent in Very High-Risk Patient With Cardiogenic Shock on V-a Ecmo
By Pornpimol Vichitchaisilp, Pavit Pienvichit, Thinnakrit Sasiprapha
Presenter
Pornpimol Vichitchaisilp
Authors
Pornpimol Vichitchaisilp1, Pavit Pienvichit1, Thinnakrit Sasiprapha1
Affiliation
Ramathibodi Hospital, Thailand1,
View Study Report
TCTAP C-154
IMAGING AND PHYSIOLOGIC LESION ASSESSMENT - Imaging: Intravascular
Successful Management of Dislodged Left Main Stent in Very High-Risk Patient With Cardiogenic Shock on V-a Ecmo
Pornpimol Vichitchaisilp1, Pavit Pienvichit1, Thinnakrit Sasiprapha1
Ramathibodi Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
A 69-year old female with hypertension and dyslipidemia
Relevant Clinical History and Physical Exam
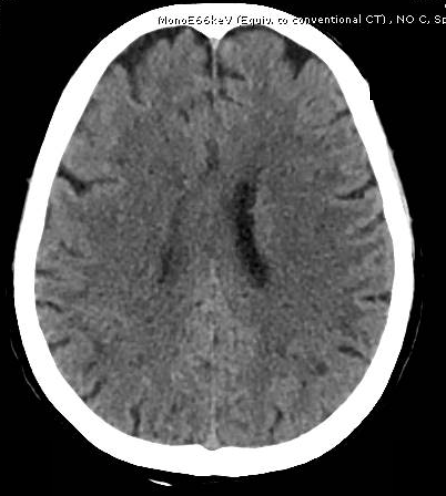
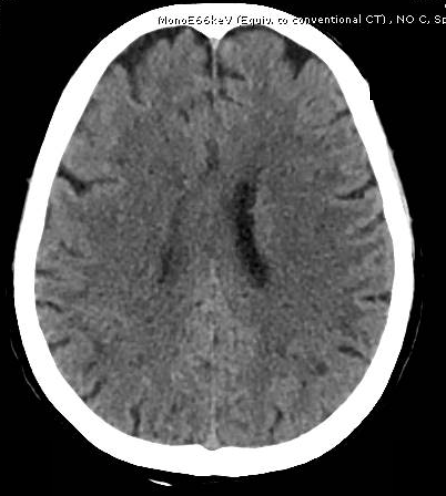
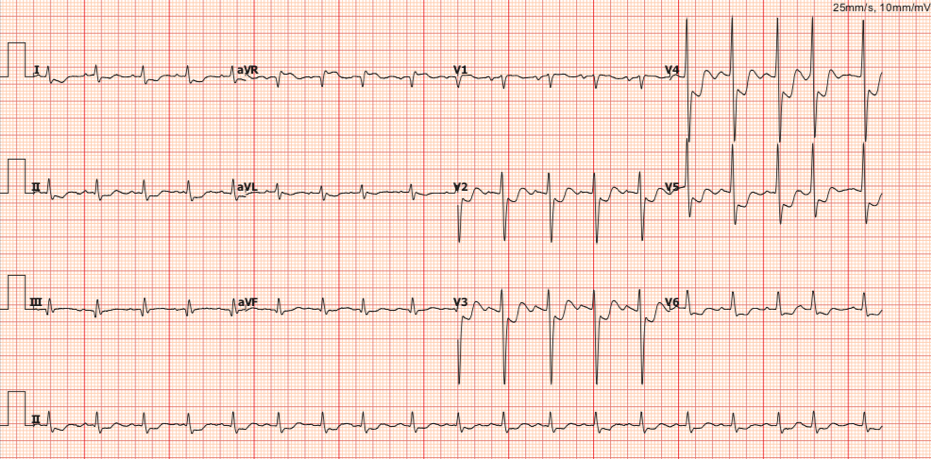
She presented with very high-risk NSTEMI and cardiogenic shock on IABP. The CAG showed TVD with severe stenosis of LM bifurcation. She was referred to our hospital for coronary bypass surgery. Unfortunately, the operation had to be postponed due to her having acute large left MCA infarction and lobar pneumonia. The heart team planned to proceed with urgent PCI after pneumonia improved. Furthermore, she developed refractory ventricular tachycardia; VA-ECMO was attempted for maintained hemodynamics.


Relevant Test Results Prior to Catheterization
Relevant Catheterization Findings
The coronary angiogram demonstrated severe stenosis of ostial left circumflex and left anterior descending arteries (LM bifurcation, Medina 0,1,1). The proximal to mid LAD had heavy calcification with moderate stenosis. The right coronary artery had chronic total occlusion that received collateral flow from left coronary system.
 LCA1.mp4
LCA1.mp4
 LCA2.mp4
LCA2.mp4
 RCA.mp4
RCA.mp4
Interventional Management
Procedural Step
The T-stenting technique via the femoral approach was used. After deployed the drug eluting stent (DES) at ostial LCx with DES 3.0 mm x 13 mm, mid LAD with DES 2.5 x 32 mm and ostial LAD with DES 3.0 x 19 mm, the coronary angiogram demonstrated moderate stenosis at the body and distal LM. As a result, the DES 4.5 x 8 mm had to be placed at the LM. Following the deployment of LM stent and post-dilated with non-compliance 5.0 mm balloon, the LM stent disappeared and was not seen along the guiding and femoral sheath. The intravascular ultrasound (IVUS) was prompted into the LAD, showing dislodgement of the partially deployed LM stent in the proximal LAD. We then optimally deployed the dislodged stent using the non-compliance balloon 3.0 x 15 mm at the proximal LAD effectively. The final IVUS showed optimal stent apposition and good expansion without stent edge dissection and we deferred to stent the LM due to the minimal luminal area of LM was 14 mm2.
 Stent LM1-2.mp4
Stent LM1-2.mp4
 IVUS pre.mp4
IVUS pre.mp4
 IVUS post.mp4
IVUS post.mp4
Case Summary
Dislodgement of the coronary stent during percutaneous coronary intervention is a serious complication. This report demonstrated the successful management of total stent loss with guide wire in situ by the recrossing technique. The IVUS is particularly helpful in the determining the characteristics within LM lesion, and its use following LM intervention improves clinical outcomes.