Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-010
Primary PCI in a Patient With Multiple Organ Failure: Is There Room for Complete Revascularization in the Index Procedure?
By Nicolaus Novian Dwiya Wahjoepramono, Antonia Anna Lukito, Riyandi Ardi Putra Fernandes, Sonia Chandra, Indah Sukmawati
Presenter
Nicolaus Novian Dwiya Wahjoepramono
Authors
Nicolaus Novian Dwiya Wahjoepramono1, Antonia Anna Lukito1, Riyandi Ardi Putra Fernandes1, Sonia Chandra1, Indah Sukmawati2
Affiliation
Siloam Hospitals Lippo Village, Indonesia1, Siloam Hospital Lippo Village, Universitas Pelita Harapan, Indonesia2,
View Study Report
TCTAP C-010
CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS)
Primary PCI in a Patient With Multiple Organ Failure: Is There Room for Complete Revascularization in the Index Procedure?
Nicolaus Novian Dwiya Wahjoepramono1, Antonia Anna Lukito1, Riyandi Ardi Putra Fernandes1, Sonia Chandra1, Indah Sukmawati2
Siloam Hospitals Lippo Village, Indonesia1, Siloam Hospital Lippo Village, Universitas Pelita Harapan, Indonesia2,
Clinical Information
Patient initials or Identifier Number
Mr. BS
Relevant Clinical History and Physical Exam
69-year-old man was admitted to the emergency department with chest pain. He was severely distressed and diaphoretic with blood pressure of 160/80 mmHg, heart rate of 128bpm, and respiratory rate of 26 x/min. He has an extensive smoking history and known chronic obstructive pulmonary disease. He also has a history of chronic kidney disease. Physical examination revealed pulmonary congestion with signs of respiratory failure. The patient was promptly intubated, and we planned for a primary PCI strategy.
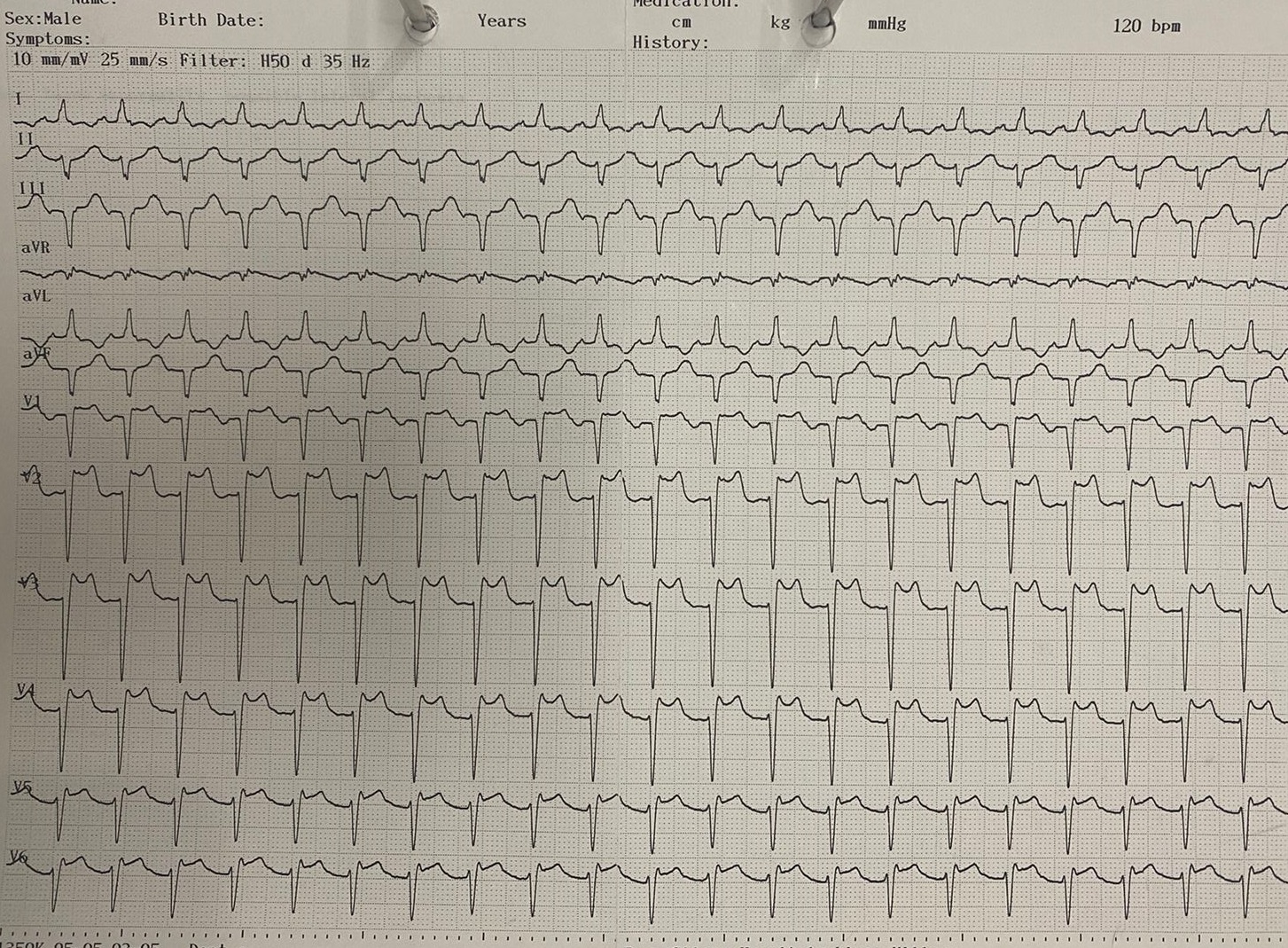
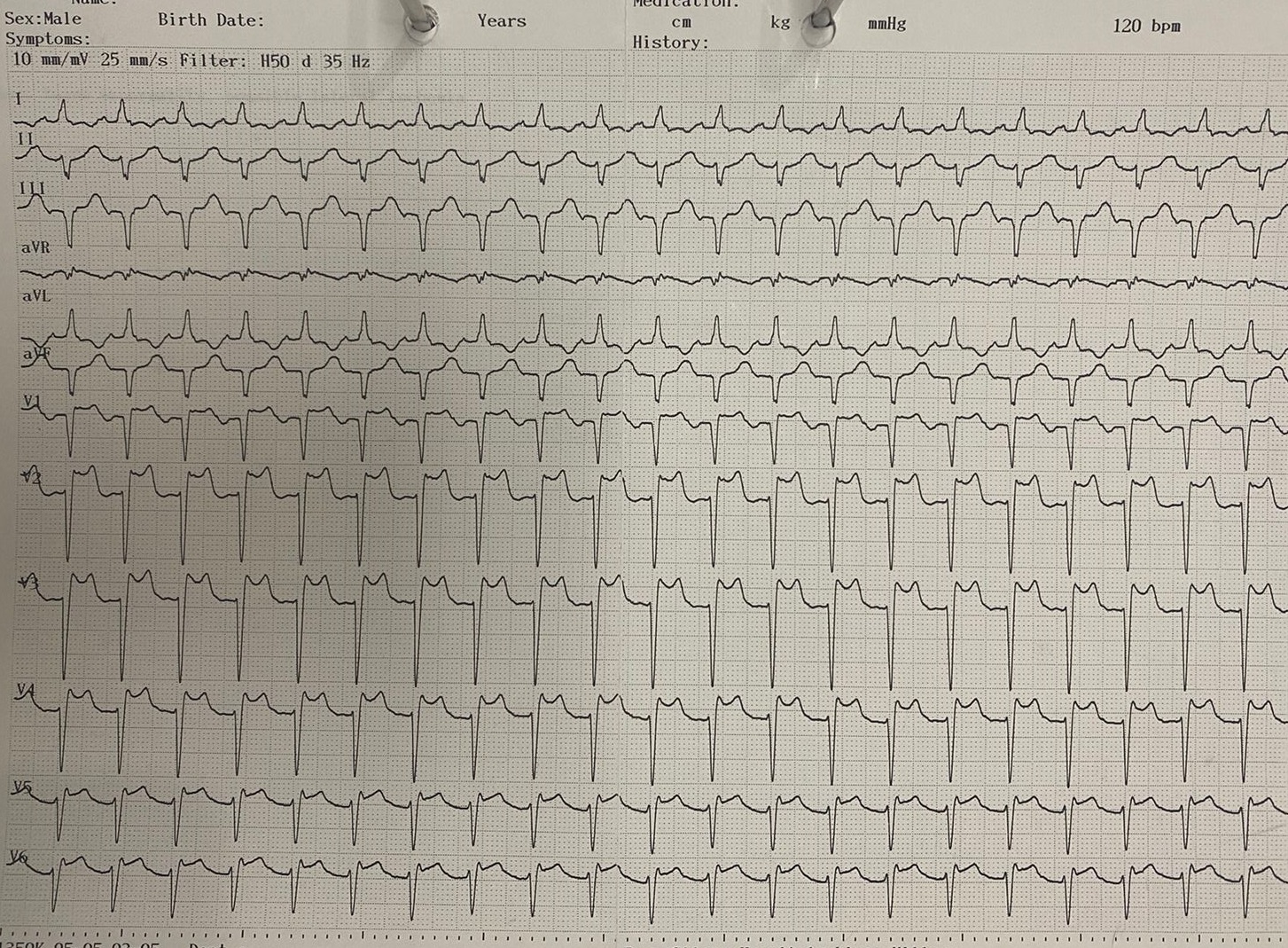
Relevant Test Results Prior to Catheterization
Initial electrocardiogram reveals sinus rhythm, 120 bpm, with an anterior STEMI. Laboratory exam confirms respiratory failure and secondary pulmonary infection, prompting early mechanical ventilation support. The patient also has acute kidney injury exacerbating his CKD, with a blood creatinine of 3.6 mg/dL, which would severely limit the amount of contrast to be used safely.
Relevant Catheterization Findings
Primary coronary angiography revealed normal left main coronary artery. There was total occlusion in the proximal left anterior descending artery with TIMI flow 0. Left circumflex artery was slightly aneurysmatic in the distal segment. Right coronary artery showed mild 40% stenosis in the ostium, mild 30% stenosis in the proximal segment with post-stenotic aneurysm, severe 90% stenosis in the mid segment, and moderate 50% stenosis in the mid-distal segment.
 LCA RAO CRA 1Pre.avi
LCA RAO CRA 1Pre.avi
 RCA LAO CRA 1Pre.avi
RCA LAO CRA 1Pre.avi
Interventional Management
Procedural Step
Intervention was first directed to the LAD. BMW guidewire was inserted through JL3.5-6F guiding catheter. Predilation was performed with Across HP Balloon 2.0-15 mm at the proximal LAD, followed by the implantation of DES Xience Sierra 3.5-15 mm at 12 atm. Postdilation was performed with the stent balloon at 16 atm. Resulting coronary flow TIMI flow 3. The procedure was continued with intervention towards the severe stenosis in the RCA. BMW Guidewire was inserted through JR3.5-6F guiding catheter. Predilation was performed with Across HP Balloon 2.0-15 mm at the mid RCA, followed by the implantation of DES Xience Sierra 3.5-18 mm at 12 atm. Postdilation was performed with the stent balloon at 16 atm. Resulting coronary flow TIMI flow 3. Acute kidney injury on CKD limited the amount of contrast the patient could safely be subjected to, but additional PCI was performed nonetheless with this in mind. In total, 65mL of Iomeron contrast was used. We felt that complete revascularization in the index procedure was a warranted strategy because the severity of the patient’s initial presentation would make any future endeavors too late. With a complete revascularization strategy, any issues the patient may face could be addressed with the knowledge that myocardial supply has been dealt with. After 6 days, the patient was able to wean off mechanical ventilation despite secondary pulmonary infection, ventricular tachycardia, and dialysis. The patient recovered well.
 LCA RAO CRA 3postStent.avi
LCA RAO CRA 3postStent.avi
 RCA LAO CRA 2positioning.avi
RCA LAO CRA 2positioning.avi
 RCA LAO CRA 3postStent.avi
RCA LAO CRA 3postStent.avi
Case Summary
Previous trials have shown the benefits of complete revascularization in reducing their primary outcomes, but recommend an initial IRA stenting strategy followed by a later routine PCI. Complete revascularization at the index primary PCI procedure exhibit additional risks and benefits that must be accounted for. Due to complete revascularization at the index procedure, we were able to secure myocardial perfusion, which may help in the recovery of a severe case of anterior STEMI. Complete revascularization of all significant stenoses in a primary PCI environment may have an increased risk, but also provide benefits not only in patients presenting with shock, but also with multi-organ dysfunction.