Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-110
Stuck Rotational Atherectomy Burr During Percutaneous Coronary Intervention of Left Main Plus Proximal Left Circumflex Artery Total Occlusion
By Hao-Yun Chang, Hsien-Li Kao
Presenter
Hao-Yun Chang
Authors
Hao-Yun Chang1, Hsien-Li Kao1
Affiliation
National Taiwan University Hospital, Taiwan1,
View Study Report
TCTAP C-110
CORONARY - Complications
Stuck Rotational Atherectomy Burr During Percutaneous Coronary Intervention of Left Main Plus Proximal Left Circumflex Artery Total Occlusion
Hao-Yun Chang1, Hsien-Li Kao1
National Taiwan University Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
C.S.C.
Relevant Clinical History and Physical Exam
A 70-year-old male presented with non-ST elevation acute coronary syndrome 2 months ago. Successful percutaneous coronary intervention (PCI) with stenting was done to right coronary artery (RCA) and left descending coronary artery (LAD). Coronary artery disease risk factors included diabetes mellitus and dyslipidemia. He was admitted due to recurrent exertional dyspnea and chest tightness for 1 month. Physical examination was essentially normal.
Relevant Test Results Prior to Catheterization
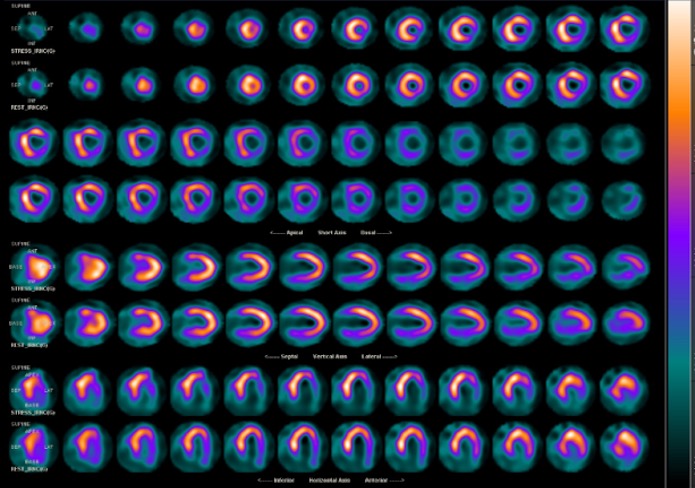
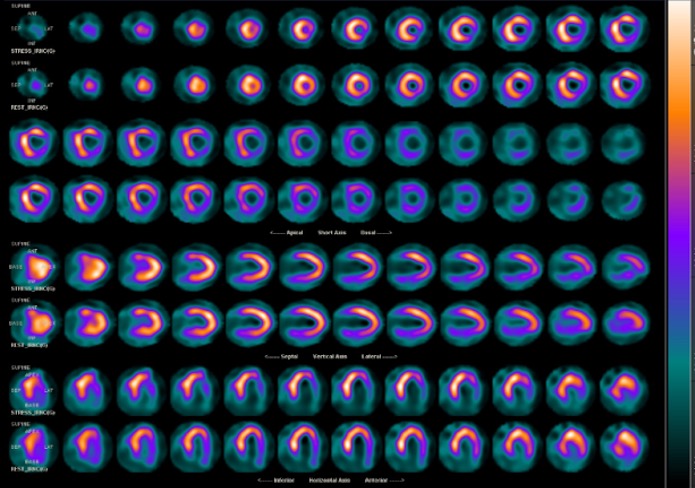
Electrocardiogram showed ST depression over lateral leads. Myocardial perfusion image revealed mixed significant viable ischemic and nonviable myocardium at inferolateral wall. Left ventricular ejection fraction was normal (59.1%) with regional wall motion abnormality at lateral wall by echocardiography.
Relevant Catheterization Findings
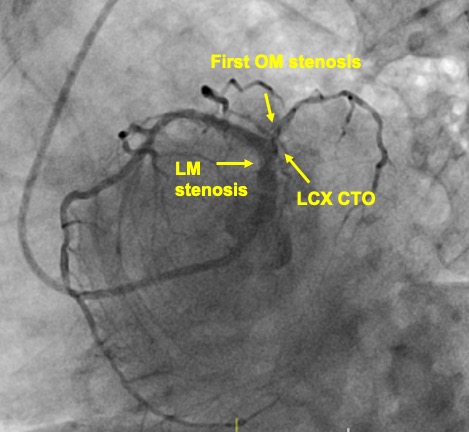
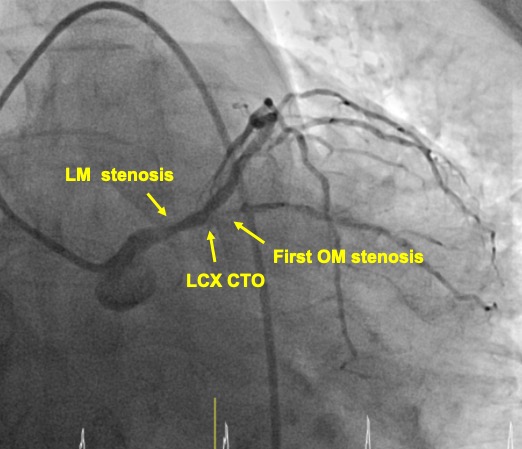
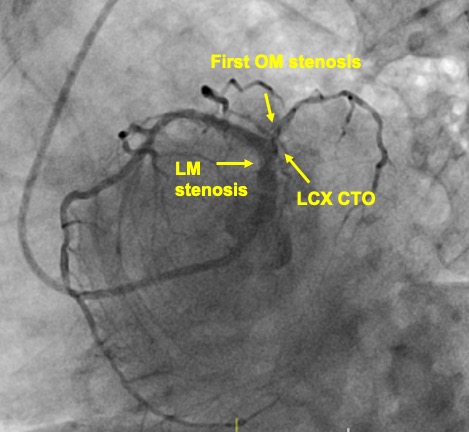
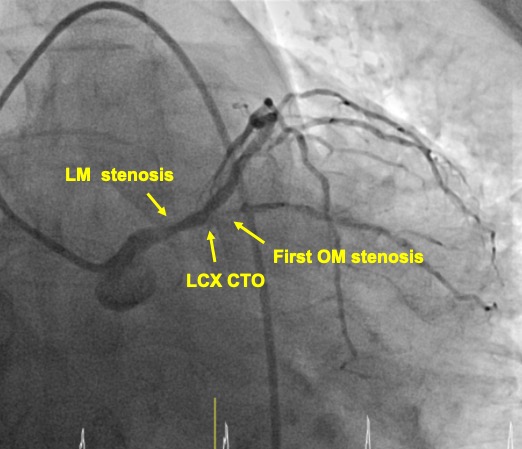
The coronary angiography revealed 80% stenosis at left main (LM) shaft. Proximal LAD had no significant instent restenosis. Chronic total occlusion (CTO) was found in proximal left circumflex coronary artery (LCX) with heavy calcification, and with the first obtuse marginal artery (OM) 80% stenosis. RCA was patent without ISR, providing collaterals to distal LCX.
Interventional Management
Procedural Step
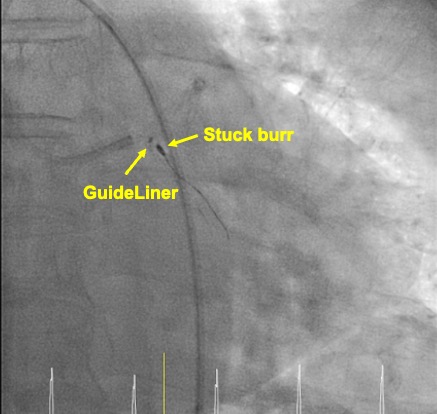
Right femoral access was chosen. LM was engaged with 7Fr BL4 guide catheter(GC) and RCA was engaged with 6Fr AL1 catheter. A Sion Blue was passed to distal LAD, and a Fielder XTA was delivered into the OM through the side port of a Sazuke dual lumen microcatheter(MC). OM was dilated with 1.5mm balloon before intravascular ultrasound(IVUS), to identify LCX entry. The XTA was exchanged to Sion through Corsair Pro MC. Sazuke was loaded over the Sion, and a Gaia Second wire successfully crossed the CTO through the side port of Sazuke. Once the distal true lumen position was confirmed by contralateral injection, Gaia Second was exchanged to Runthrough floppy. Both 2.5mm semi- and non-compliant(NC) balloons failed to dilate the lesion fully, and delivery of a Scoreflex balloon with the support of a 6Fr GuideLiner failed. Runthrough was exchanged to Rotawire Extrasupport wire. A 1.5mm burr was activated at 175000 rpm, but the burr stalled and was stuck in the process. Manual pullback failed to retrieve the burr. We cut the driveshaft and Rotawire, advanced the GuideLiner over the remaining shaft/wire, and successfully pulled out the GC/GuideLiner/burr as an unit. After reengaging, we found the LCX had good flow. Due to extreme angulation and calcification at LM-LCX junction, we decided not to further intervene. A 3.0mm drug-eluting stent was deployed at LM-LAD, followed by proximal optimization technique with a 4.0mm NC balloon. IVUS confirmed good result, with final TIMI 3 flow.
 success pullout.mp4
success pullout.mp4
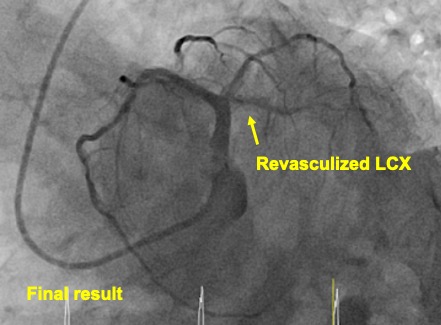
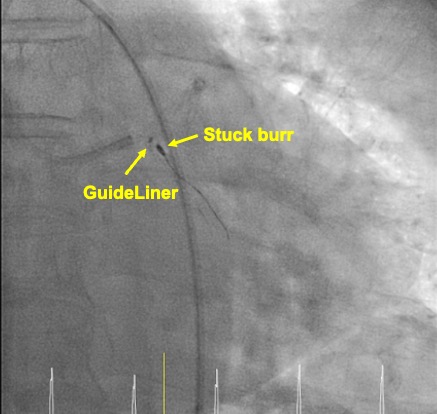
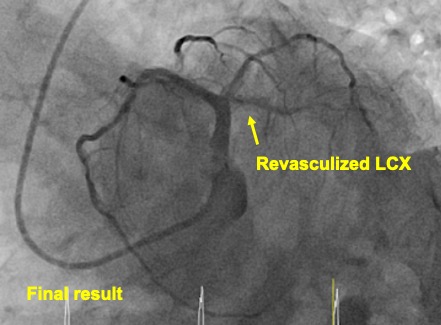
Case Summary
This case demonstrated a complicated LM stenosis, involving a totally occluded LCX. The acute bend from LM into LCX, and severe calcification complicated successful rotablation burr passage, resulting in burr stuck. We introduced a maneuver to retrieve the burr, preventing surgical removal. Despite this unexpected complication, in addition to other challenging characteristics of the lesion complexity, procedure results were acceptable. Familiarity with devices and techniques is the key to bail the interventionist as well as the patient out of this dire situation.