Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-074
High-Risk Coronary Intervention to the ‘Last Standing’ Left Circumflex Artery
By Huzairi Sani, Khairul Shafiq Ibrahim, Muhammad Hanis Muhmad Hamidi, Ahmad Bakhtiar Md Radzi, Raja Ezman Raja Shariff, Johan Rizwal Ismail, Abdul Wahab Undok, Hafisyatul Aiza Zainal Abidin, Sazzli Kasim
Presenter
Huzairi Sani
Authors
Huzairi Sani1, Khairul Shafiq Ibrahim2, Muhammad Hanis Muhmad Hamidi2, Ahmad Bakhtiar Md Radzi2, Raja Ezman Raja Shariff3, Johan Rizwal Ismail4, Abdul Wahab Undok5, Hafisyatul Aiza Zainal Abidin2, Sazzli Kasim2
Affiliation
Hospital Pantai Klang, Malaysia1, Universiti Teknologi MARA (UiTM), Malaysia2, Hospital Universiti Teknologi MARA (UiTM), Malaysia3, Prince Court Medical Centre, Malaysia4, Kpj Rawang Specialist Hospital, Malaysia5,
View Study Report
TCTAP C-074
CORONARY - Complex and Higher Risk Procedures for Indicated Patients (CHIP)
High-Risk Coronary Intervention to the ‘Last Standing’ Left Circumflex Artery
Huzairi Sani1, Khairul Shafiq Ibrahim2, Muhammad Hanis Muhmad Hamidi2, Ahmad Bakhtiar Md Radzi2, Raja Ezman Raja Shariff3, Johan Rizwal Ismail4, Abdul Wahab Undok5, Hafisyatul Aiza Zainal Abidin2, Sazzli Kasim2
Hospital Pantai Klang, Malaysia1, Universiti Teknologi MARA (UiTM), Malaysia2, Hospital Universiti Teknologi MARA (UiTM), Malaysia3, Prince Court Medical Centre, Malaysia4, Kpj Rawang Specialist Hospital, Malaysia5,
Clinical Information
Patient initials or Identifier Number
Madam ZR
Relevant Clinical History and Physical Exam
A 48-year-old with long-standing poorly controlleddiabetes mellitus, hypertension, dyslipidaemia, and 3 vessels coronary arterydisease was referred for progressive angina. She also had symptoms of orthopnoeaand bilateral leg swelling. Clinically she was in warm and wet decompensated heartfailure requiring oxygen supplement 3 L/minute via nasal prong. Heart Team meetingdiscussion decided not to surgical intervene due to poor vessel targets.
Relevant Test Results Prior to Catheterization
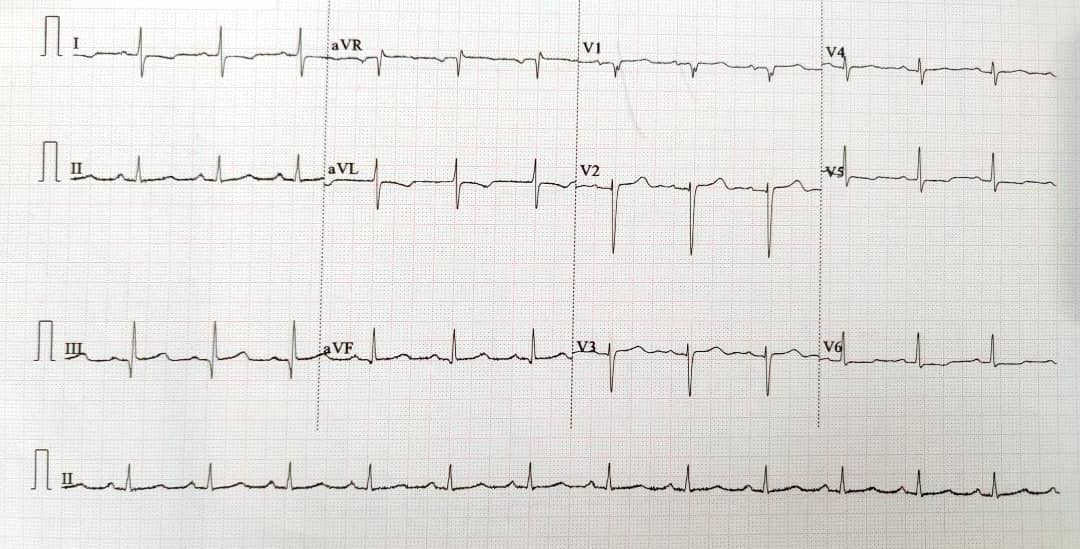
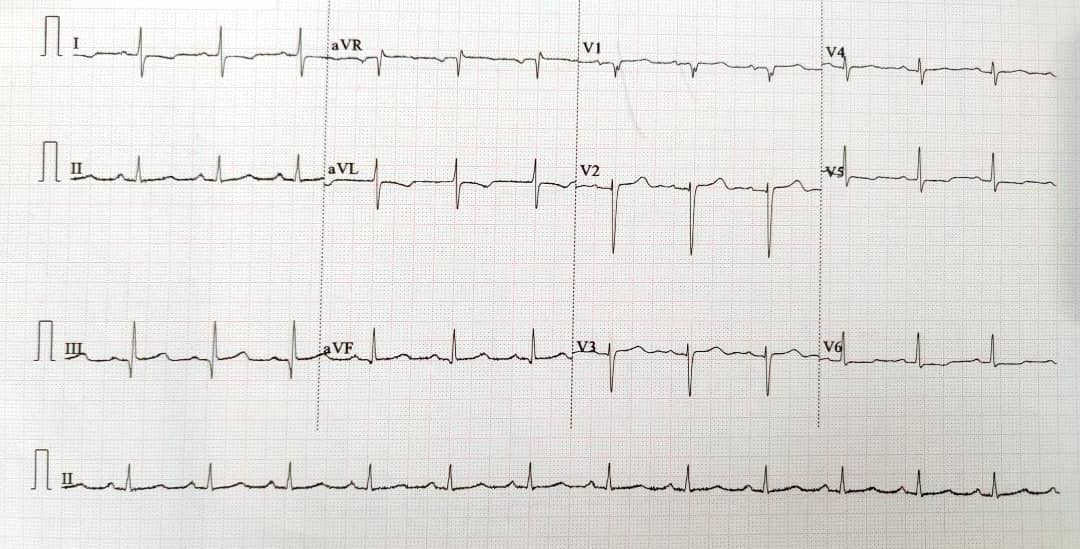
The electrocardiogram showed ST-depression at lead I, aVL,V5, and V6 with poor R-wave progression. The NT-proBNP reported was 2361 pg/ml andTroponin T of 19 ng/L. Her HBA1c was 11.2 %. Otherwise, routine blood testsprior to catheterization procedure were unremarkable. Cardiac MRI revealed a leftventricular ejection fraction of 15% and non-viable mid to apical rightcoronary artery territories on gadolinium study. There was an atrial septaldefect causing right ventricular dilatation.


Relevant Catheterization Findings
Coronaryangiogram revealed: Severe stenosis at distal left main; diffuse subtotalstenosis of the left anterior descending artery; severe stenosis at the ostialleft circumflex artery and chronic total occlusion at mid-right coronary artery.
 diagnostic AP caudal.mp4
diagnostic AP caudal.mp4
Interventional Management
Procedural Step
PCI to left circumflex artery into the left main artery. Rightfemoral artery access for PCI with Intra-Aortic Balloon Pump (IABP) supportfrom left femoral. Left main was engaged using guiding catheter JL 3.5 6Fr.Wired distal left circumflex with workhorse Runthrough wire. IVUS run for vesselsize, length, and lesion characterization. Pre dilated with a 2.5 x 15 mm balloonwith pressure up to 16 ATM. Sion blue was used as a second wire for support. A stent 3.0 x 28 mm deployed from left circumflexinto the left main artery with a pressure of 11 ATM. Stent was post dilated withan NC balloon 3.5 x 15 mm. 2nd IVUS run showed well-apposed stentand no complications i.e edge dissection or hematoma.
 IABP EBU wire.mp4
IABP EBU wire.mp4
 IVUS run 1 .mp4
IVUS run 1 .mp4
 stent deploy.mp4
stent deploy.mp4
 IVUS run post stent.mp4
IVUS run post stent.mp4
 final spider.mp4
final spider.mp4
Case Summary
The evolution of percutaneous coronary interventions (PCI)has been remarkable during the past decades. The never-ending research,innovation, development of new techniques, and new device technologies improvethe success rates. This has resulted in sicker patients with more complexlesions that can now be treated by PCI. Oursubject was a high-risk candidate with worsening angina, heart failure, and refractoryto medical therapy. It is of utmost essential to discuss the risks and benefitsof the intervention with the patient, family, and hospital personnel. Immediateappropriate measures can be taken before and during the high-risk PCI tominimize the risk of major adverse event.