Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-003
A Night to Remember
By Faten Aqilah Aris, Wan Faizal Bin Wan Rahimi Shah, Chee Kiang Teoh
Presenter
Faten Aqilah Aris
Authors
Faten Aqilah Aris1, Wan Faizal Bin Wan Rahimi Shah1, Chee Kiang Teoh1
Affiliation
National Heart Institute, Malaysia1,
View Study Report
TCTAP C-003
CORONARY - Acute Coronary Syndromes (STEMI, NSTE-ACS)
A Night to Remember
Faten Aqilah Aris1, Wan Faizal Bin Wan Rahimi Shah1, Chee Kiang Teoh1
National Heart Institute, Malaysia1,
Clinical Information
Patient initials or Identifier Number
Mr CCS
Relevant Clinical History and Physical Exam
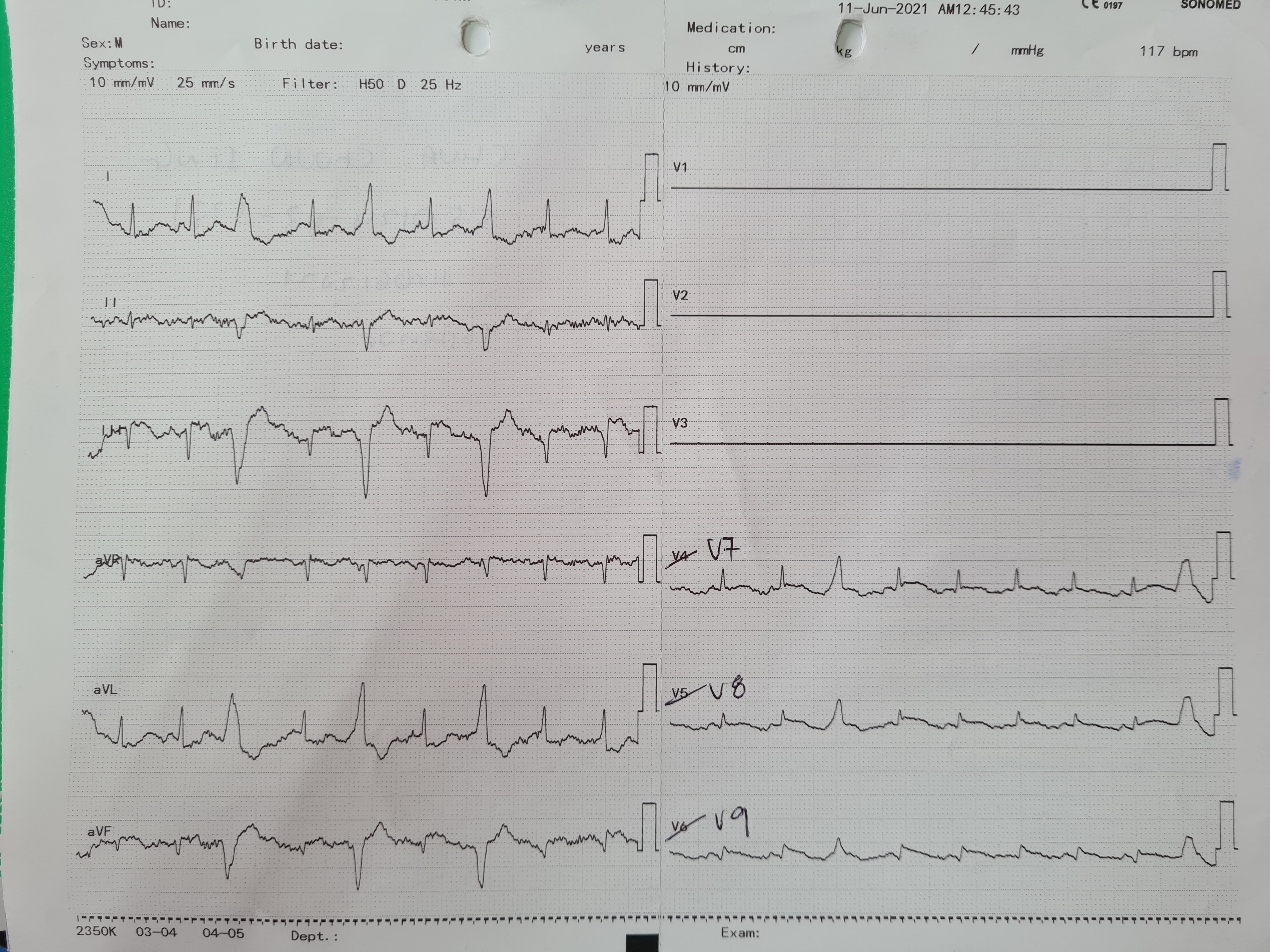
66-year-old male with underlying diabetes mellitus,hypertension, and history of CVA 2019. He presented to another hospital withcomplaints of chest pain for 6 hours, associated with difficulty breathingand diaphoresis. ECG showed SR, ST elevation inferior leads and ST depressionanterolateral leads. He required intubation in view of frank, acutepulmonary edema. Post intubation single ionotropic support was initiated priorto transfer. He was transferred to IJN at 2 am.
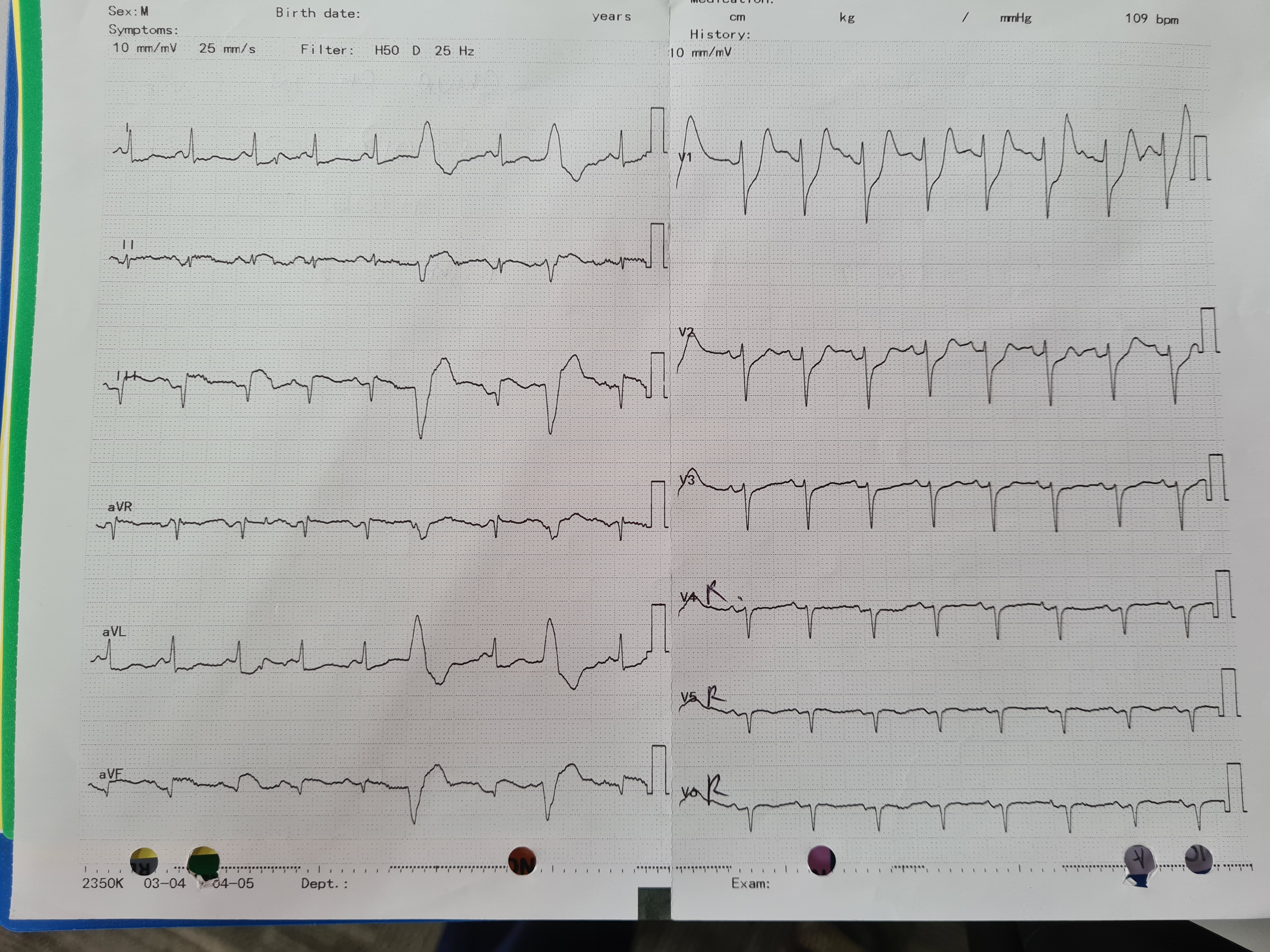
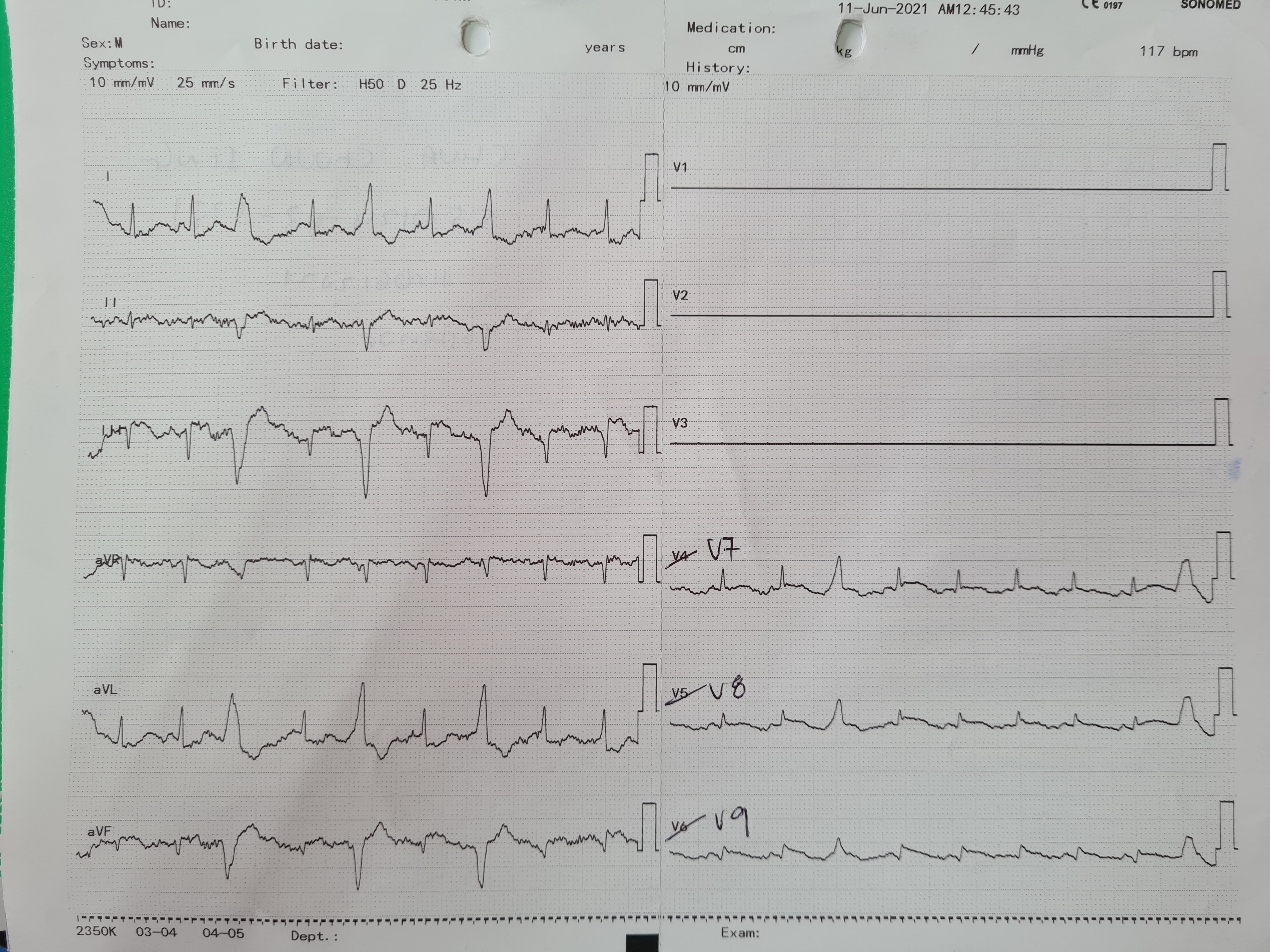
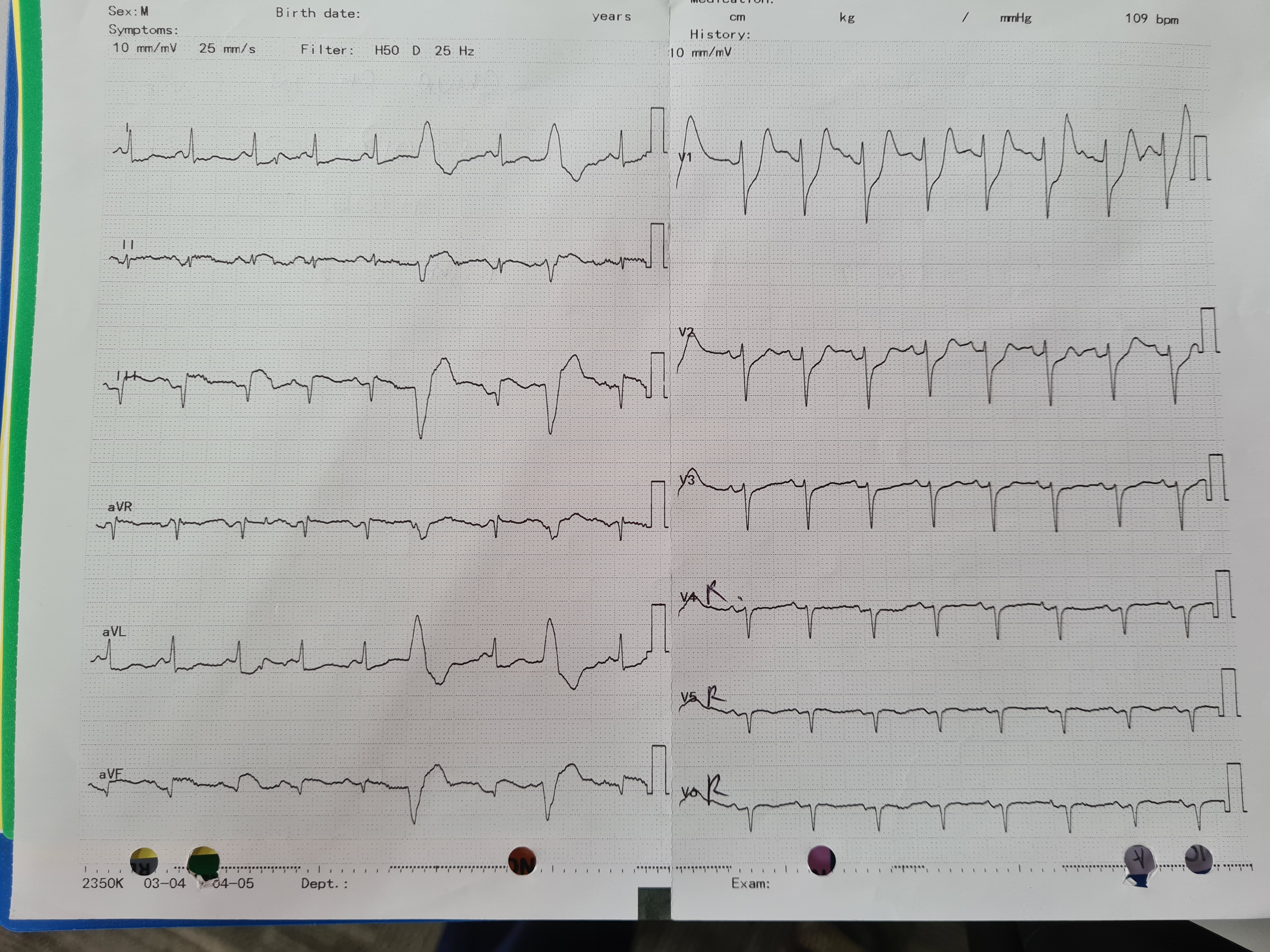
Relevant Test Results Prior to Catheterization
Bedside ECHO: global hypokinesia. EF 35%. No significant valvular lesions.
Relevant Catheterization Findings
LMS: NormalLAD: Tight mid LAD with diffuse disease distallyLCx: Occluded proximal tapering stump/ Acute or Chronic total occlusion, absent of retrograde flowRCA: Moderate ostial to proximal then occluded. Faint retrograde flow
Impression: 3VD with occluded LCx/RCA in Cardiogenic shock - ambiguous culprit artery LCx/RCA
 CAG 1.avi
CAG 1.avi
 CAG 2.avi
CAG 2.avi
 CAG 3.avi
CAG 3.avi
Impression: 3VD with occluded LCx/RCA in Cardiogenic shock - ambiguous culprit artery LCx/RCA
Interventional Management
Procedural Step
Urgent coronary angiogram on arrival showed Severe 3VD. Total occlusion of proximal LCx and RCA with tight mid LAD. RCA has antegrade flow, but ipsilateral bridging collaterals were present. LCx has tapering occlusion with no visualization of distal vessel architecture. Patient was hypotensive with BP 80/60 and had severe metabolic acidosis, pH 7.166 and bicarbonate 16.2. IABP inserted and inotropes escalated.
Facing conundrum of ambiguous culprit artery, decision was made to attempt RCA first. RCA crossed with workhorse wire then stented quickly with 2x DES (Resolute Onyx 3.0x30 mm and Orsiro 3.5x26 mm) after serial ballooning. LCx crossing proved more arduous as wiring to distal LCx failed due to acute (near retroflex) angulation between mid and distal LCx. Attempted angle of attack modification with 2.5 semi-compliant balloon but failed. POBA occlusion site into OM performed instead. Residual thrombus in distal LCx seen. LAD crossed quickly stented with 1x DES (Resolute Onyx 3.0x30 mm). Post LAD stenting, no flow seen in previous LCx-OM. Reattempted LCx again but failed, thus POBA with same 2.5 semi-compliant balloon again. Decided to stop at this juncture. Swan Ganz catheter inserted post procedure on table. Transferred to CCU with 3 inotropes.
 CAG 26.avi
CAG 26.avi
 CAG 55.avi
CAG 55.avi
 CAG 57.avi
CAG 57.avi
Facing conundrum of ambiguous culprit artery, decision was made to attempt RCA first. RCA crossed with workhorse wire then stented quickly with 2x DES (Resolute Onyx 3.0x30 mm and Orsiro 3.5x26 mm) after serial ballooning. LCx crossing proved more arduous as wiring to distal LCx failed due to acute (near retroflex) angulation between mid and distal LCx. Attempted angle of attack modification with 2.5 semi-compliant balloon but failed. POBA occlusion site into OM performed instead. Residual thrombus in distal LCx seen. LAD crossed quickly stented with 1x DES (Resolute Onyx 3.0x30 mm). Post LAD stenting, no flow seen in previous LCx-OM. Reattempted LCx again but failed, thus POBA with same 2.5 semi-compliant balloon again. Decided to stop at this juncture. Swan Ganz catheter inserted post procedure on table. Transferred to CCU with 3 inotropes.
Case Summary
In this case we demonstrated success of opening almost all major vessels in cardiogenic shock. It is a tricky situation, balancing the need of revascularization versus procedural risk in face of cardiogenic shock and severe acidosis.
In addition, meticulous post procedure intensive care is paramount to augment survival in cardiogenic shock patients. Hemodynamic monitoring is key in utilization of inotropes to prevent its deleterious effects while at the same time maximizing benefits.
In addition, meticulous post procedure intensive care is paramount to augment survival in cardiogenic shock patients. Hemodynamic monitoring is key in utilization of inotropes to prevent its deleterious effects while at the same time maximizing benefits.