Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-060
Rock-Hard Right Coronary Artery Chronic Total Occlusion Intervention and Thrilling Complication
By Chieh-Shou Su, Yu-Cheng Hu
Presenter
Yu-Cheng Hu
Authors
Chieh-Shou Su1, Yu-Cheng Hu1
Affiliation
Taichung Veterans General Hospital, Taiwan1,
View Study Report
TCTAP C-060
CORONARY - Chronic Total Occlusion
Rock-Hard Right Coronary Artery Chronic Total Occlusion Intervention and Thrilling Complication
Chieh-Shou Su1, Yu-Cheng Hu1
Taichung Veterans General Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Mr. Yu
Relevant Clinical History and Physical Exam
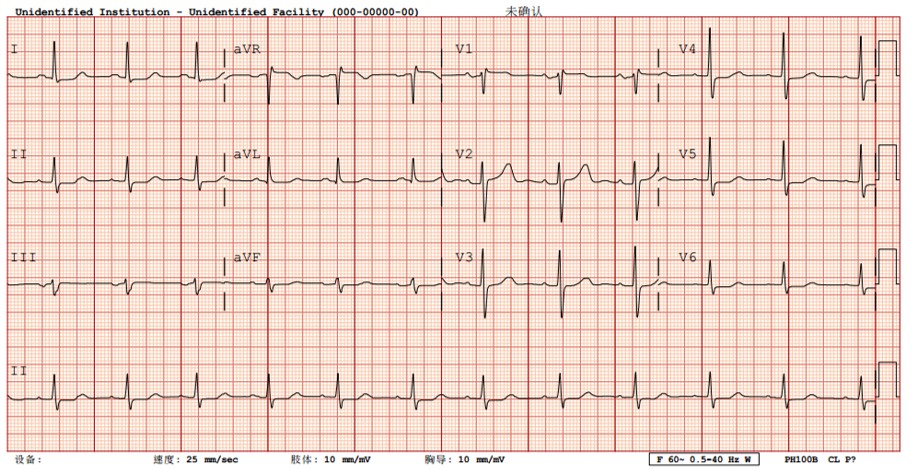
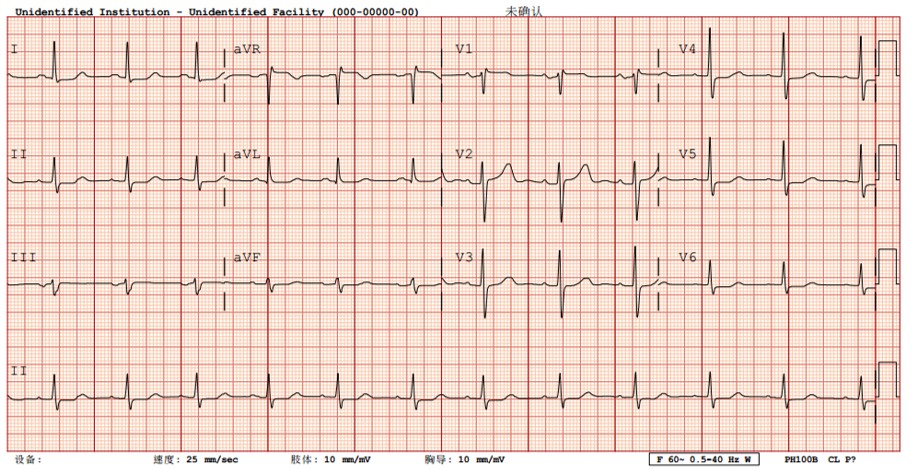
Mr. Yu was an 80-year-old man, he had pasthistory of HTN, DM, hyperlipidemia, CAD-III, he received PCI and CABG before. In July 2017 he was again admitted due to persistedchest pain, physical exam revealed BT=36.5'C, HR=65bpm, RR=18, BP=160/92mmHg, clear breathing sound in both lungs, regular heartbeat with no murmur or S3, S4. Multiple ST depressionin ECG, inferolateral LV hypokinesia in echo, CK/MB and troponin-I were normal, we decided to do PCI to remaining RCA CTO due to unstable angina.
Relevant Test Results Prior to Catheterization
CK: 61mg/dL, CKMB: 4mg/dL, troponin-I: <0.16ng/mL.Creatinine: 1.05mg/dLHbA1C: 6.2%LDL: 79mg/dL
Relevant Catheterization Findings
LCA supply collateral to PL branch and LAD-septal supply to PDA. LAD middle-distal showed competing flow from LIMA. RCA was total occluded at proximal segment, with heavy calcification. OM1 ostium showed 80% stenosis.


Interventional Management
Procedural Step
SAL 1.5 7Fr guiding catheter (GC) was used for antegrade approach, Sion blue with Corsair microcatheter was used to approach RCA, then Sion blue was exchanged to GAIA 2 wire, Sion blue was sent into conus branch to increase support. After GAIA 2 entered distal PDA true lumen, a 1.0 x 8 mm and a 1.2 x 6 mm balloon catheter was used to dilate RCA proximal CTO lesion. Corsair still could not pass RCA calcification with support of 6F guideliner, a Tornus microcatheter to drill through RCA proximal-middle calcified lesions, dilated by 2.0x20mm balloon; the RCA middle-distal lesion was again passed with Tornus microcatheter. A retrograde coronary dissection occured during antegrade injection, no chest tightness/pain, drop in BP or ECG change at that time, cardiac echo showed no pericardial effusion, contrast stasis decaded after few minutes, therefore we decided to continue PCI. After few failed attempts to dilate RCA middle-distal calcification, we decided to perform rotablation, with 1.5mm burr debulking proximal-middle RCA and 1.25mm burr for middle-distal RCA. The RCA distal to proximal was scaffolded by 2.25 x 28 mm, 2.75 x 38 mm and 3.5 x 18 mm DES and were inflated up to 10-14 bars and post dilated by 2.5 x 12 mm, 3.0 x 12 mm NC balloon up to 12-20 bars. RCA distal 50% stenosis was dilated by 2.0x20mm balloon, no further stenting due to small vessel size. Final angiogram showed TIMI 3 flow without contrast stasis.
 wire in PDA.AVI
wire in PDA.AVI
 Dissection.AVI
Dissection.AVI
 Final.AVI
Final.AVI
Case Summary
1. In patients with severe calcified coronary artery stenosis, debulking devices are mandatory for revascularization.2. When retrograde dissection occurs, the most important part is to maintain stable vital signs, and ensure no compromise to coronary flow or extravasation, if no any hemodynamic disturbance.