Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-159
Precise PCI
By Chen Ting Tan
Presenter
Tan Chen Ting
Authors
Chen Ting Tan1
Affiliation
Sarawak Heart Centre, Malaysia1,
View Study Report
TCTAP C-159
IMAGING AND PHYSIOLOGIC LESION ASSESSMENT - Physiologic Lesion Assessment
Precise PCI
Chen Ting Tan1
Sarawak Heart Centre, Malaysia1,
Clinical Information
Patient initials or Identifier Number
VS
Relevant Clinical History and Physical Exam
66 years old gentleman who is an ex-smoker with underlying medical history of hypertension, dyslipidaemia, and history of Pontine Stroke in 2020 which recovered without residual weakness. He presented with recurrent chest tightness with shortness of breath after stroke and this is not related with exertion. Otherwise, physical examination was unremarkable.
 VOON ECHO 1.mp4
VOON ECHO 1.mp4
 VOON ECHO 2.mp4
VOON ECHO 2.mp4
Relevant Test Results Prior to Catheterization
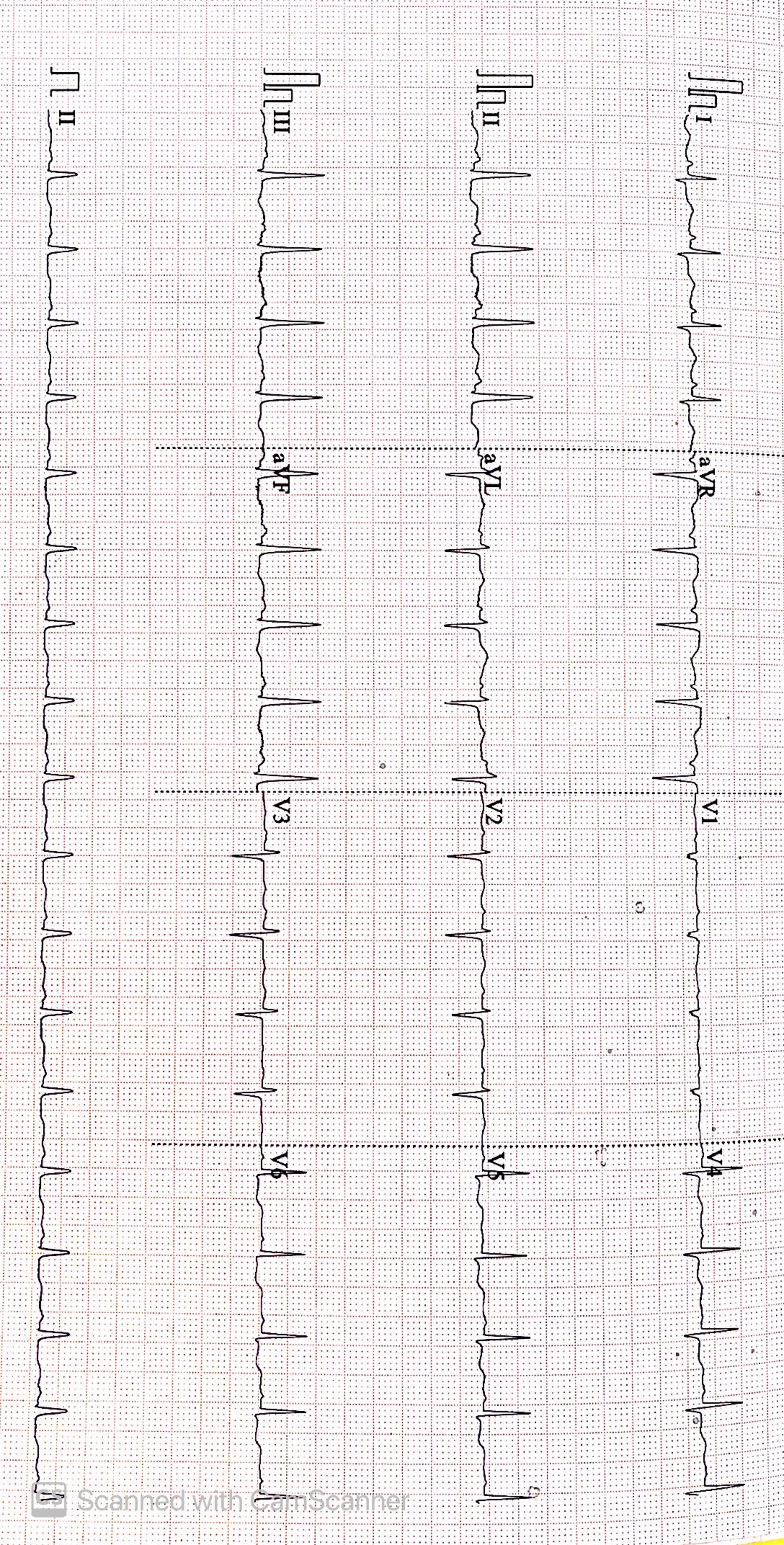
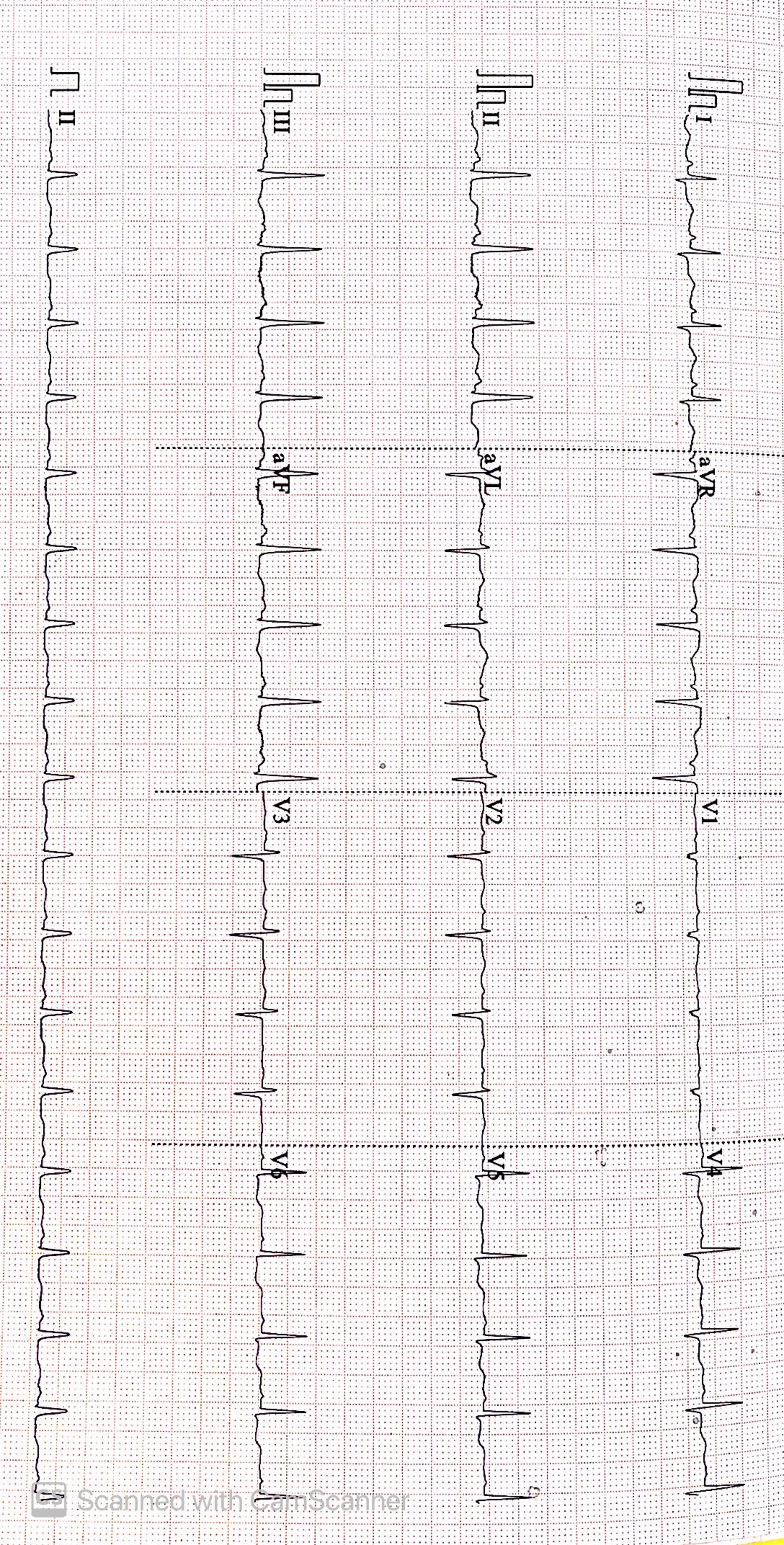
Baseline ECG normal sinus rhythm and no ischemic changes. Exercise Stress Test (EST) done but terminated at stage 2 due to shortness of breath. The EST Mets 5.7 and there is no dynamic ischemic changes in the ECG. His echocardiogram showed EF> 55% and no regional wall motion abnormalities.
 VOON XA 1.mp4
VOON XA 1.mp4
 VOON XA 2.mp4
VOON XA 2.mp4
 VOON XA 5.mp4
VOON XA 5.mp4
Relevant Catheterization Findings
Diagnostic coronary angiogram done via trans radial approach using 6F radial sheath using 5F TIG Catheter. It showed single vessel disease (SVD) with tandem lesions at the proximal, mid and distal left anterior descending artery (LAD). Otherwise, left circumflex artery (LCX) normal and 30-40% stenosis at the mid segment of right coronary artery (RCA).
Interventional Management
Procedural Step
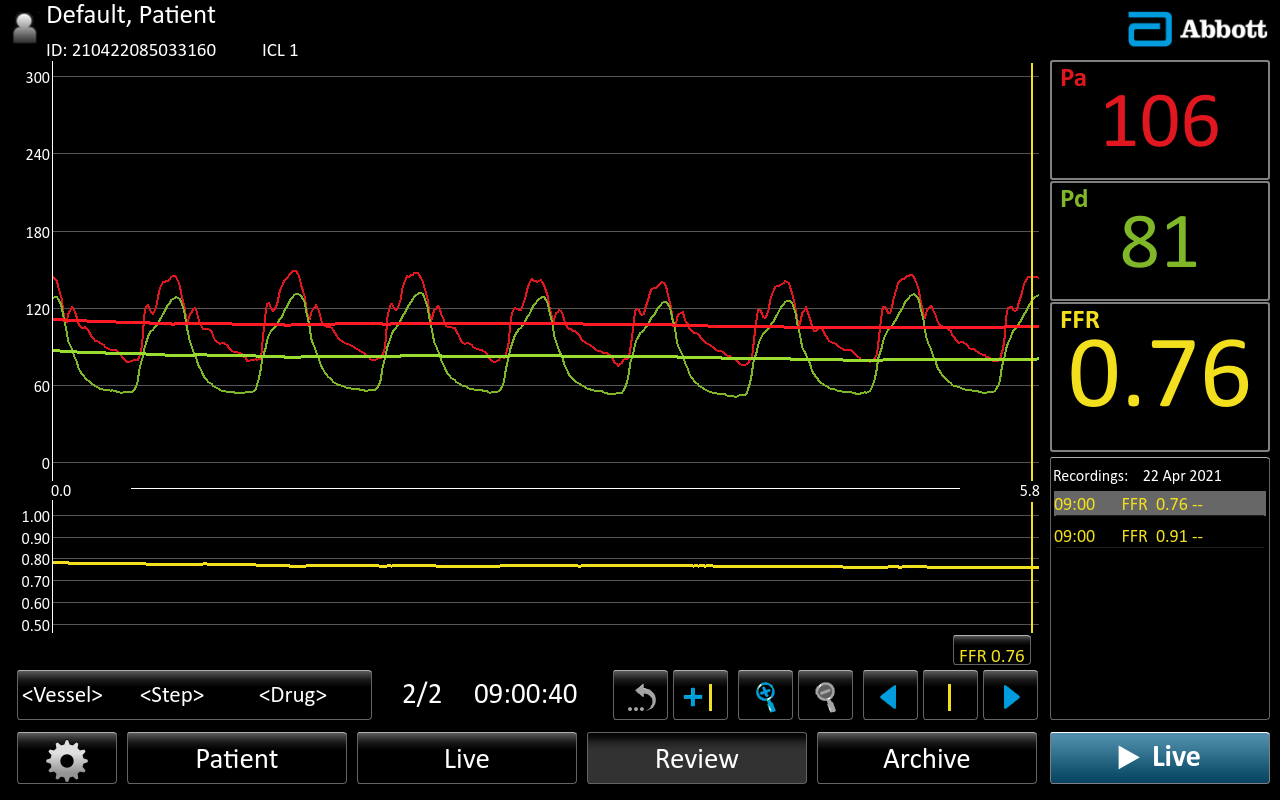
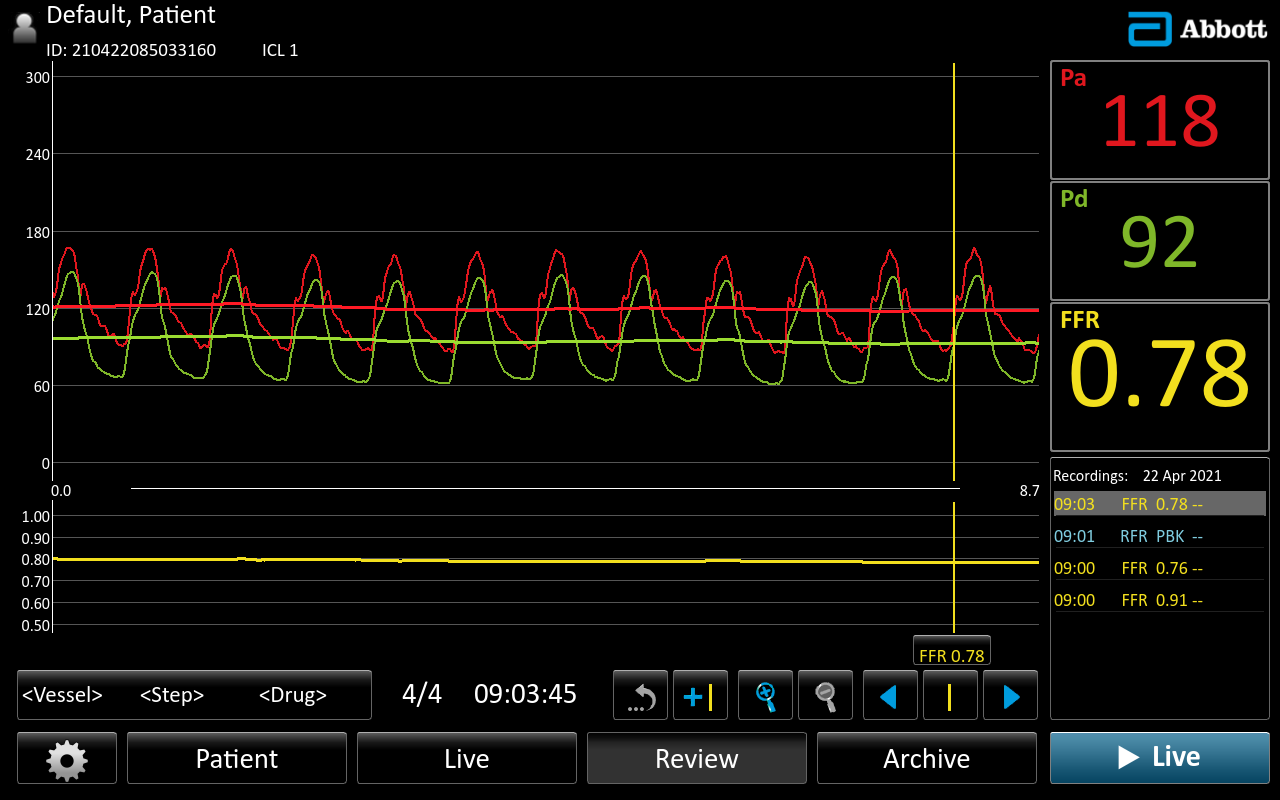
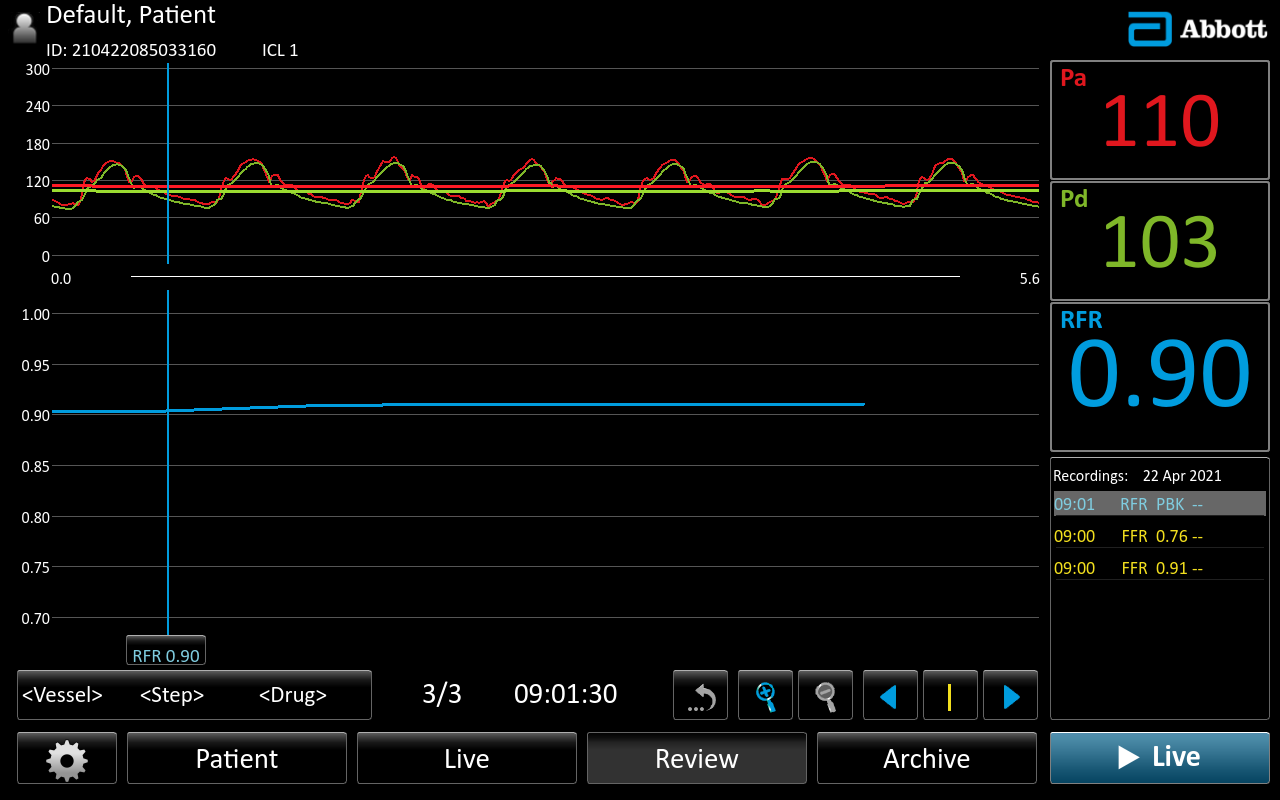
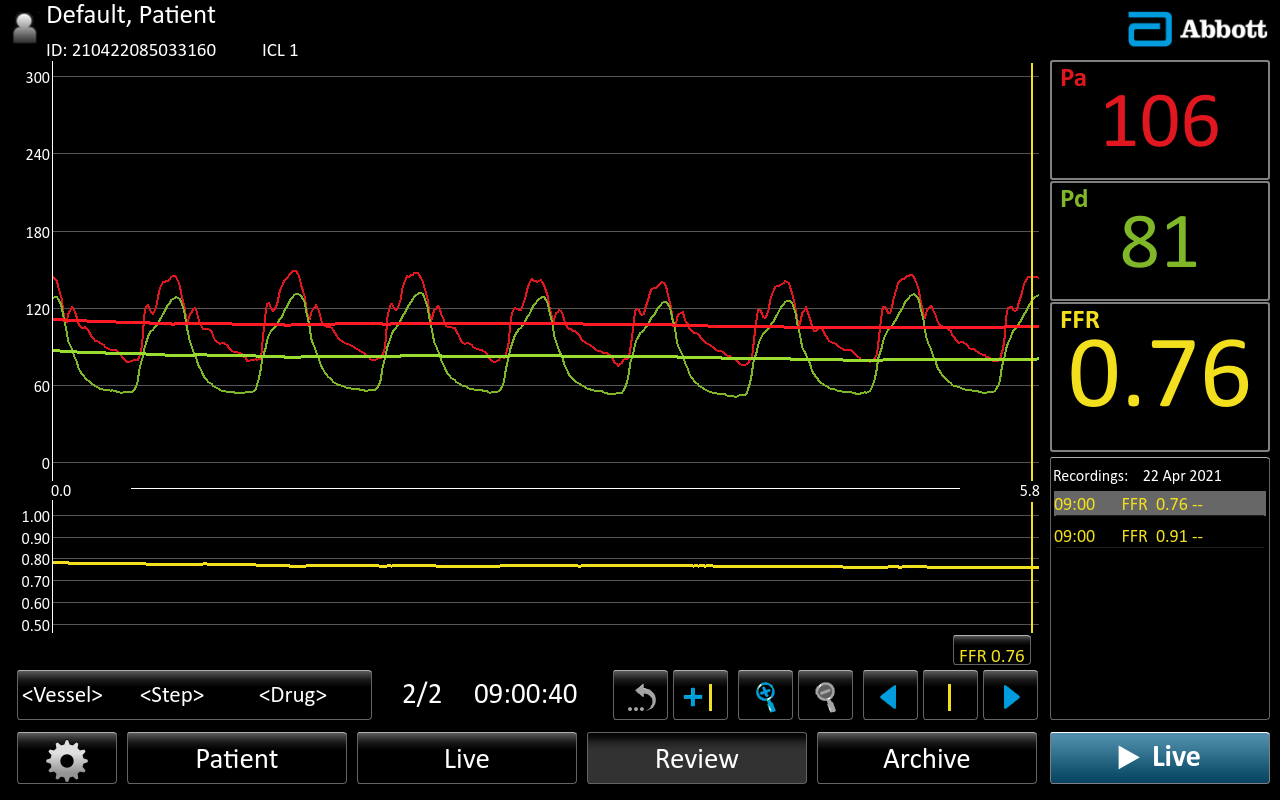
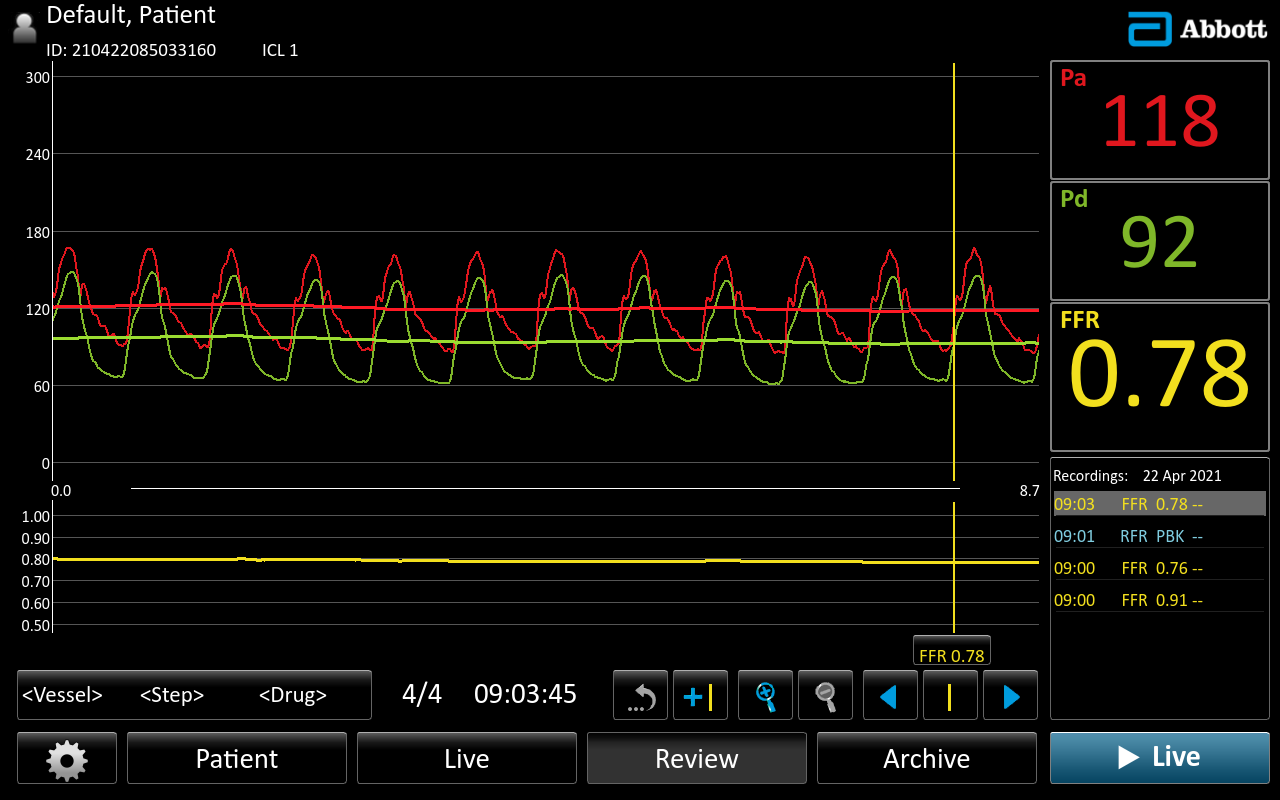
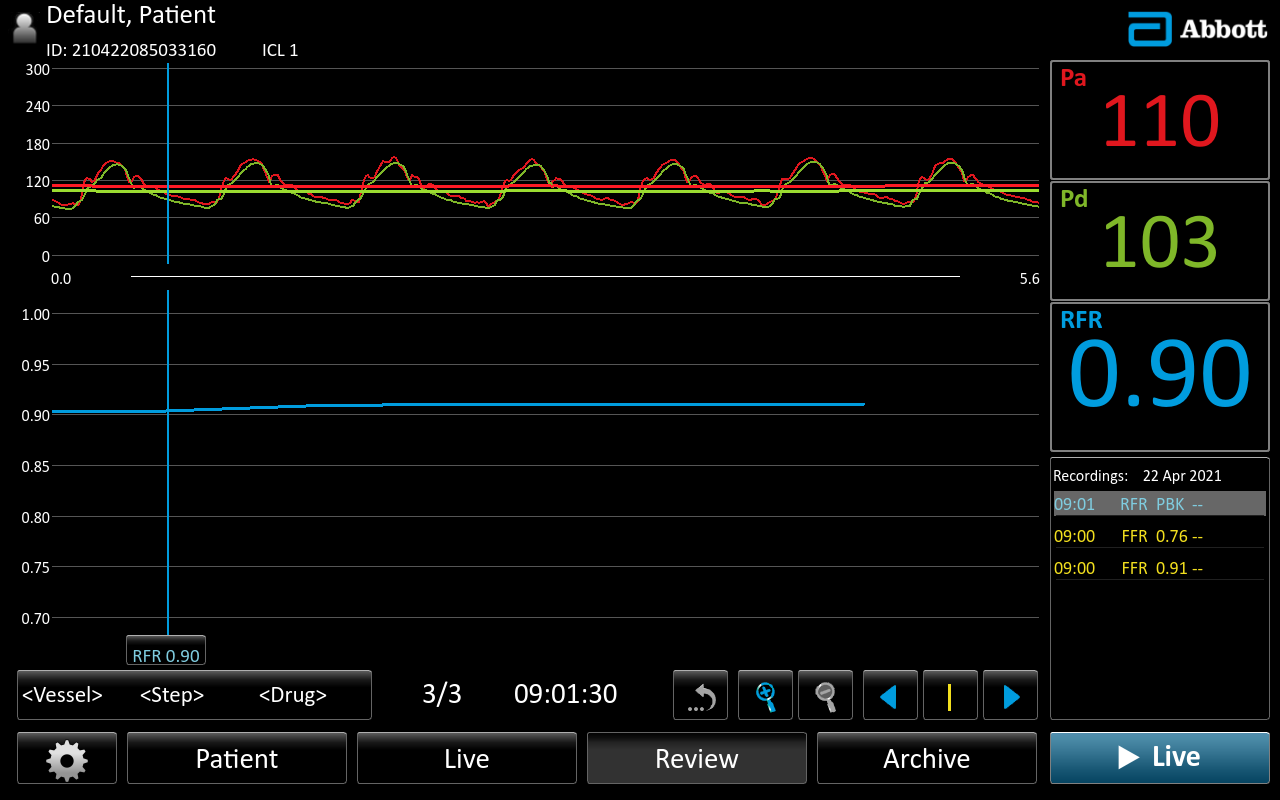
In view of tandem lesions at the LAD, we decide to do physiological assessment of LAD. A 6F EBU 3.5 engaged to left coronary artery (LCA). A 0.014” Pressure Wire X passed down to distal LAD. Intracoronary (IC) Glycerine Trinitrate (GTN) 200mcg given. Resting FFR: 0.93 and after IC adenosine 60mcg : 0.85. Proceeded with higher dose of adenosine. IC adenosine 120mcg, FFR: 0.76. FFR wire pullback to mid LAD. Resting FFR: 0.94 and after IC adenosine 120mcg, FFR: 0.78. Therefore, the significant lesion is at the proximal and mid LAD. In view of the lesion near to the ostium of LAD, we decide to do intravascular ultrasound (IVUS) guided PCI. A 40MHz Opticross catheter was used. Based on the IVUS information, the ostia LAD is not the ideal proximal landing zone due to plaque burden 53% with 2 quadrant attenuated plaque. Hence, we decide to PCI LM to Lad with drug eluting stent(DES). From IVUS, distal vessel size is 4mm, proximal LAD is 4.5mm and LM is short in length 3.5mm, 7mm in size. The lesion was pre-dilated with Nc balloon 3.0 x 12 mm up to 20 atm then treated with DES 3.5 x 48mm at 11atm. Post-dilated with NC balloon 4.0 x15 mm up to 24atm then proximal optimisation (POT) with NC balloon 5.0 x 8mm up to 20atm. Final IVUS done. The distal expansion index (EI) > 100%. The ostia LAD minimum stent area (MSA) is 12.98mm2 and LM MSA 14.93mm2.
 VOON XA 21.mp4
VOON XA 21.mp4
 PRE PCI IVUS.mp4
PRE PCI IVUS.mp4
 NC 4.0 IVUS.mp4
NC 4.0 IVUS.mp4
Case Summary
Physiological guided management of coronary stenosis is an appropriate strategy while dealing with patients with diffuse disease. This helps in stratifying lesions and deciding which lesions will benefit from revascularization. It transforms into a physiology driven complete revascularization. Together with intravascular imaging, this optimise the PCI result which lead to better clinical outcome.