Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-124
Contemporary Management of Myocardial Infarction With Cardiogenic Shock
By Jonathan Gabriel Sung, Ho Lam, Ping Wa Yam
Presenter
Jonathan Gabriel Sung
Authors
Jonathan Gabriel Sung1, Ho Lam1, Ping Wa Yam1
Affiliation
Tuen Mun Hospital, Hong Kong, China1,
View Study Report
TCTAP C-124
CORONARY - Hemodynamic Support and Cardiogenic Shock
Contemporary Management of Myocardial Infarction With Cardiogenic Shock
Jonathan Gabriel Sung1, Ho Lam1, Ping Wa Yam1
Tuen Mun Hospital, Hong Kong, China1,
Clinical Information
Patient initials or Identifier Number
YPK
Relevant Clinical History and Physical Exam
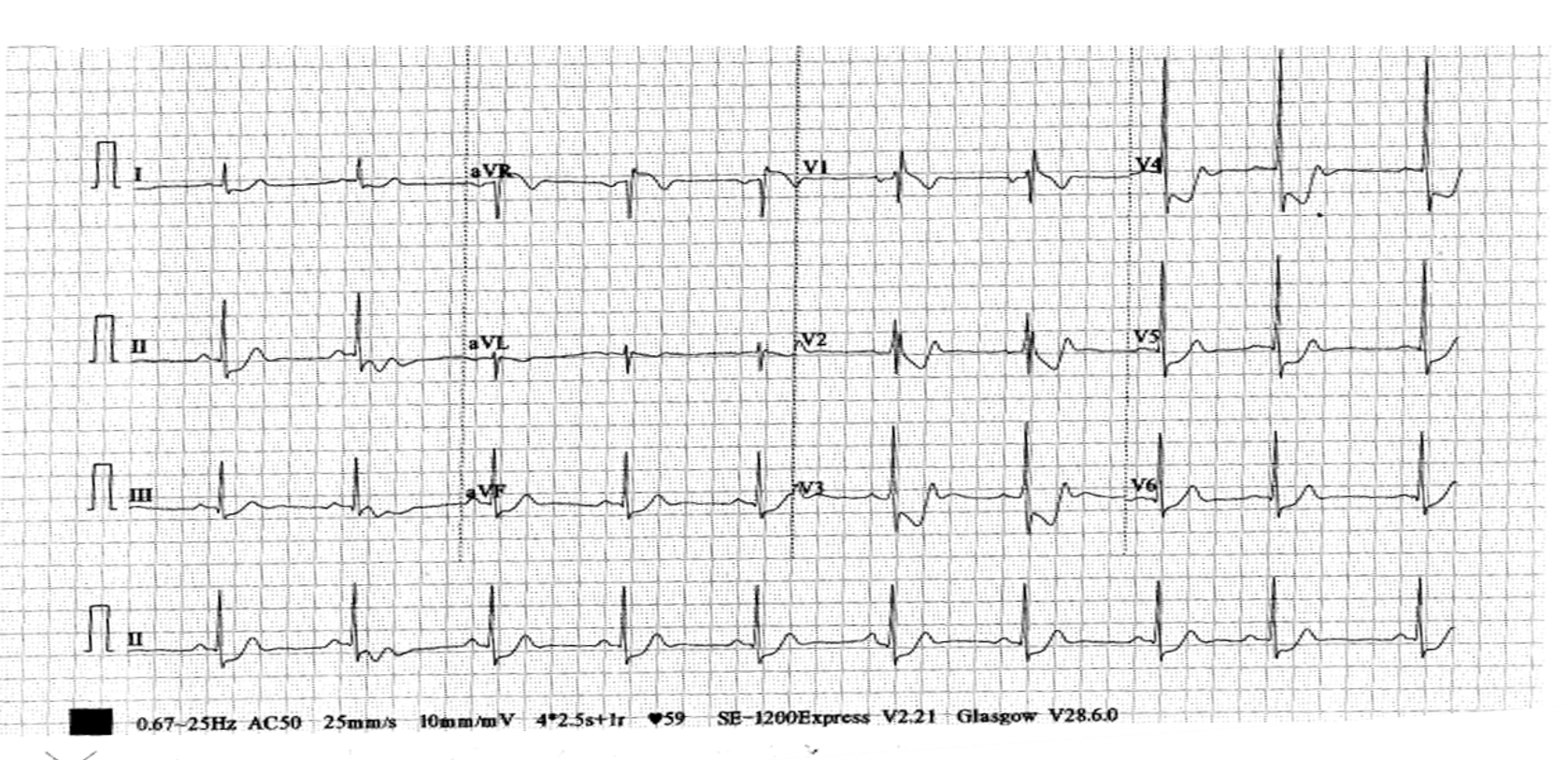
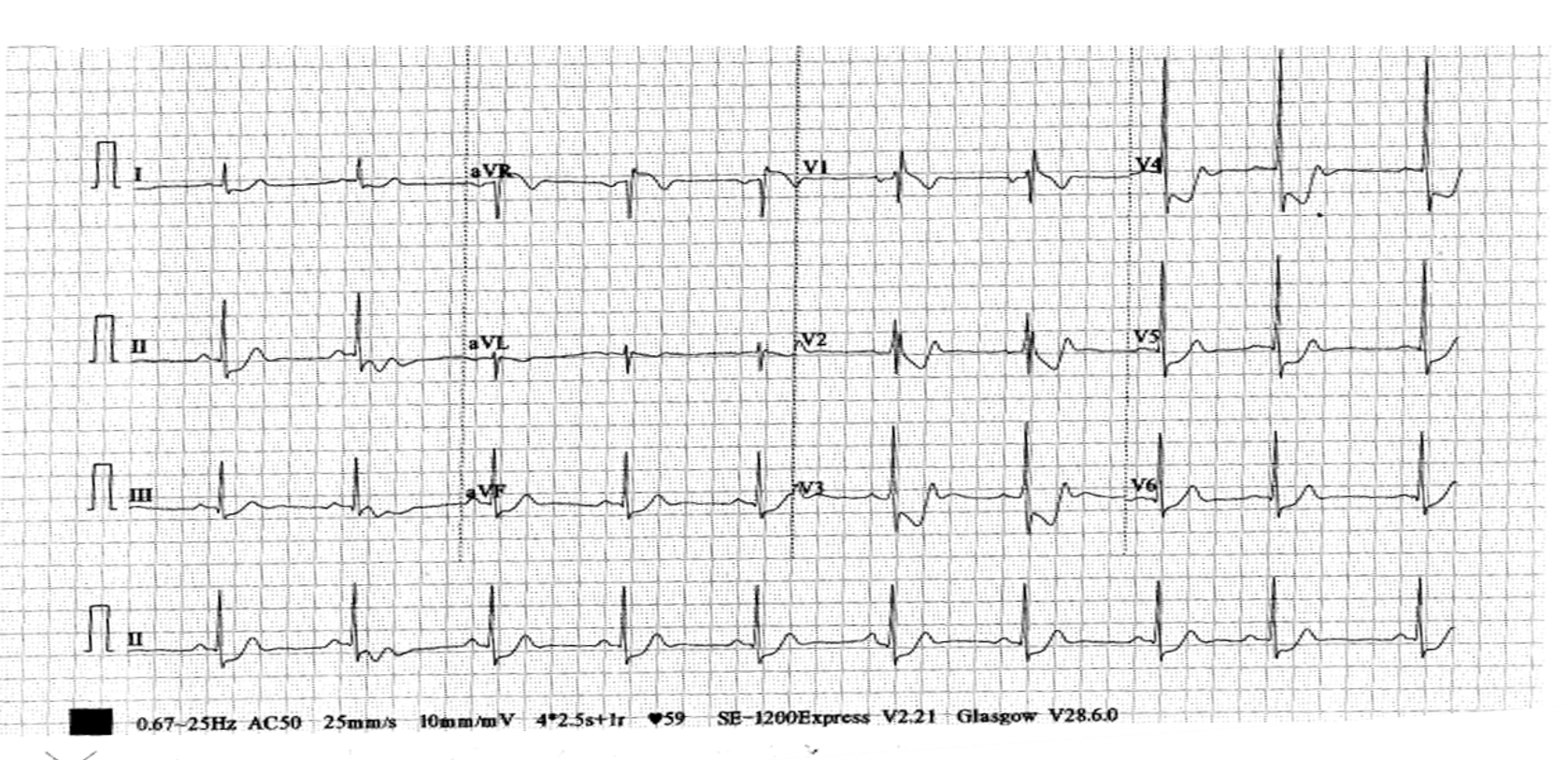
A 66-year-old man, with history of smoking and otherwise unremarkable past health, presented with acute chest pain while jogging. At the emergency department, his blood pressure was 90/60 mmHg with cool and clammy peripheries. There was no audible murmur. Chest was clear to auscultation.
Relevant Test Results Prior to Catheterization
First ECG revealed ST elevation over aVR and diffuse ST depression over precordial leads. Bedside echocardiogram showed EF of 40% with anterolateral wall hypokinesis.
Relevant Catheterization Findings
He was directly transferred to the catheterization laboratory. Right radial artery (RRA) and right femoral artery (RFA) accesses were obtained at the beginning of the procedure. Coronary angiogram demonstrated total occlusion over proximal left circumflex artery (LCx) and 99% stenosis over mid-segment of left anterior descending artery (LAD). Right coronary artery (RCA) was grossly normal. LVEDP was approximately 30 mmHg.
 1) LCA cine.mp4
1) LCA cine.mp4
 2) LCA cine.mp4
2) LCA cine.mp4
 3) RCA cine.mp4
3) RCA cine.mp4
Interventional Management
Procedural Step
In view of clinical cardiogenic shock, unstable hemodynamics and high-risk coronary anatomy, Impella was deployed via RFA before proceeding to PCI. EBU 3.5 7Fr was used to intubate the left main coronary artery. Runthrough NS crossed proximal LCx occlusion. Dottering with semi-compliant balloon restored antegrade flow in LCx. A 3.5 mm x 15 mm DES was deployed in proximal LCx. Post-stent angiogram showed distal migration of thrombus although coronary flow remained at TIMI III. Two boluses of Eptifibatide were administered in LCx via dual-lumen microcatheter while intravenous Eptifibatide infusion was commenced. While we were awaiting the action of Eptifibatide, we proceeded to PCI of LAD with a 3.0 mm x 24 mm DES. Repeated angiogram showed persistent thrombus in LCx. We performed mechanical thrombectomy with Penumbra aspiration catheter. After one run of aspiration, the thrombus in LCx was cleared and flow remained at TIMI III. Further stent optimization was performed under IVUS guidance. Impella was slowly and successfully weaned off in the catheterization laboratory.
 4) LCx post-stent.mp4
4) LCx post-stent.mp4
 5) LAD post-stent.mp4
5) LAD post-stent.mp4
 6) LCx post-thrombectomy.mp4
6) LCx post-thrombectomy.mp4
Case Summary
Firstly, optimal time of initiating MCS in high-risk PCI remains controversial. In this case, Impella support was initiated before PCI based on coronary anatomy, clinical presentation and hemodynamic status. Without MCS, patient might experience hemodynamic collapse during PCI and require bail-out MCS, which is associated with high mortality.Secondly, pharmacological and mechanical thrombolysis together successfully cleared the large thrombus burden without compromising blood flow.Thirdly, routine revascularization of non-infarct artery during primary PCI is generally not recommended in STEMI with cardiogenic shock. However, if MCS is in place, complete revascularization might be reasonable.