Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-138
Shaking Aortic Plaque
By Sheng-Fu Liu, Ying-Hsien Chen, Po-Chih Lin, Hsien-Li Kao
Presenter
Sheng-Fu Liu
Authors
Sheng-Fu Liu1, Ying-Hsien Chen2, Po-Chih Lin2, Hsien-Li Kao2
Affiliation
National Taiwan University Hospital Hsin-Chu Branch, Taiwan1, National Taiwan University Hospital, Taiwan2,
View Study Report
TCTAP C-138
ENDOVASCULAR - Complications
Shaking Aortic Plaque
Sheng-Fu Liu1, Ying-Hsien Chen2, Po-Chih Lin2, Hsien-Li Kao2
National Taiwan University Hospital Hsin-Chu Branch, Taiwan1, National Taiwan University Hospital, Taiwan2,
Clinical Information
Patient initials or Identifier Number
80 year old lady
Relevant Clinical History and Physical Exam
An 80-year-old woman was a case of left subclavian artery stenosis and received stenting in 2010. Then she received balloon angioplasty for in-stent restenosis in 2012. This time, she presented a 6-month history of recurrent dizziness during left arm exertion.
Relevant Test Results Prior to Catheterization
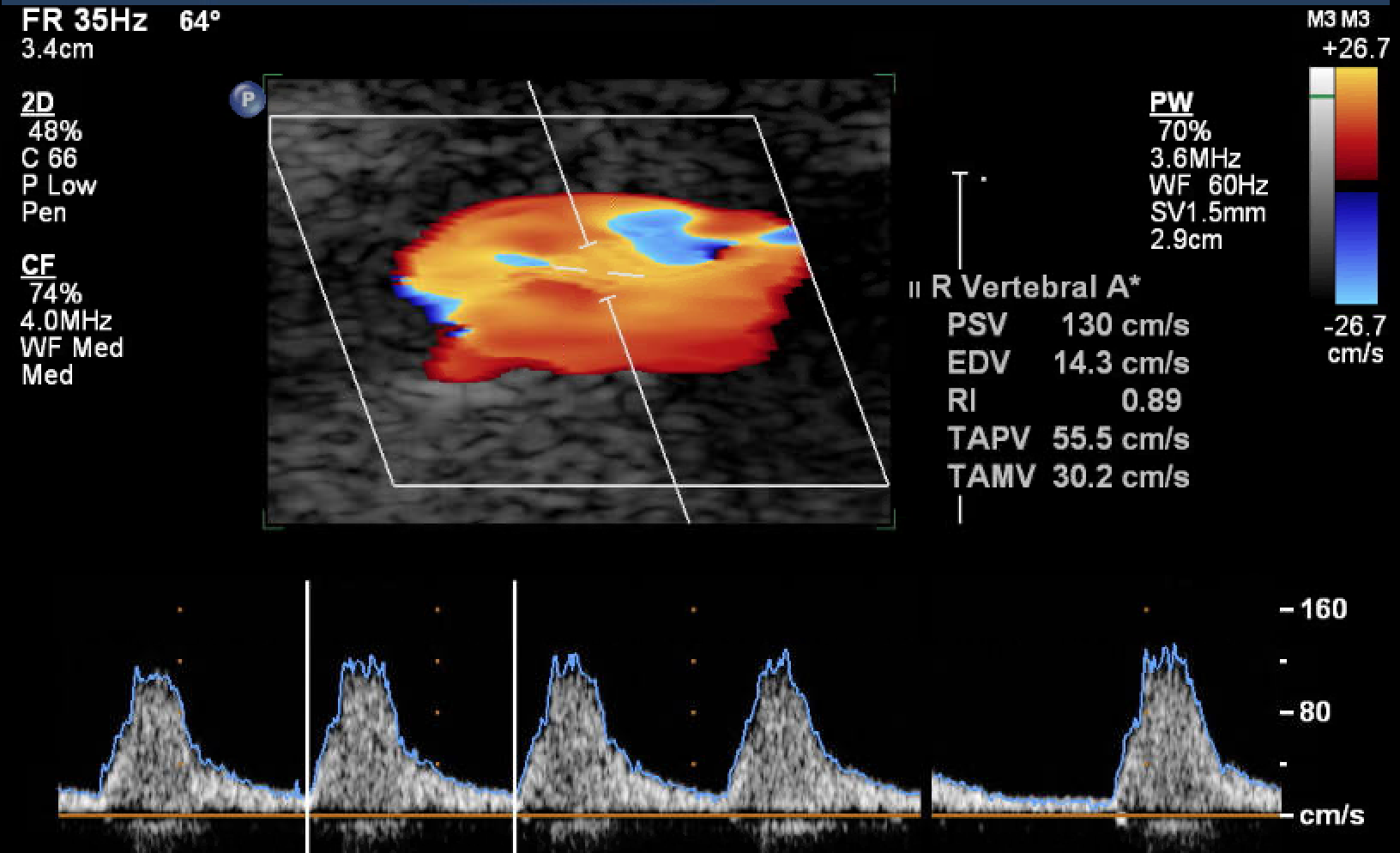
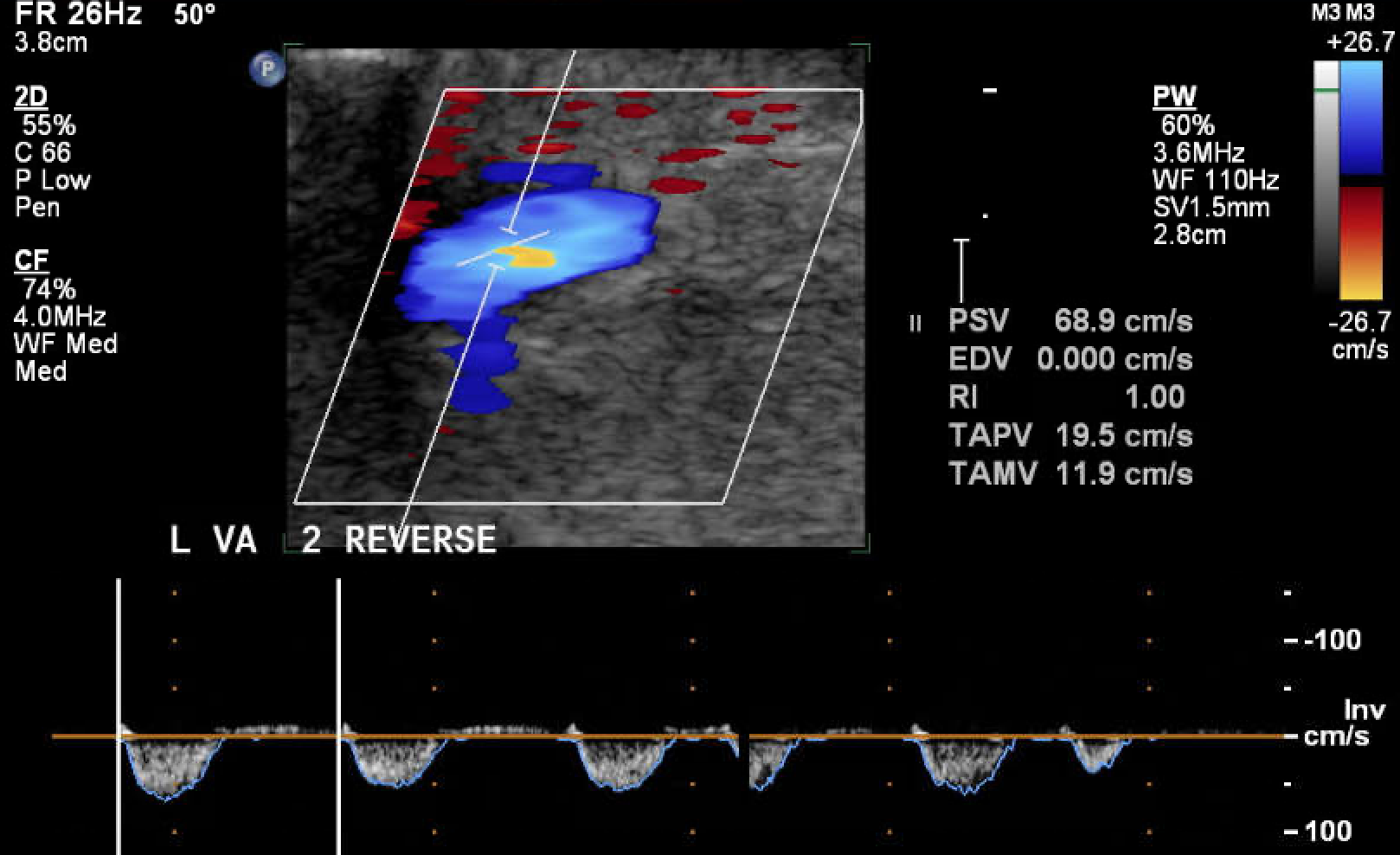
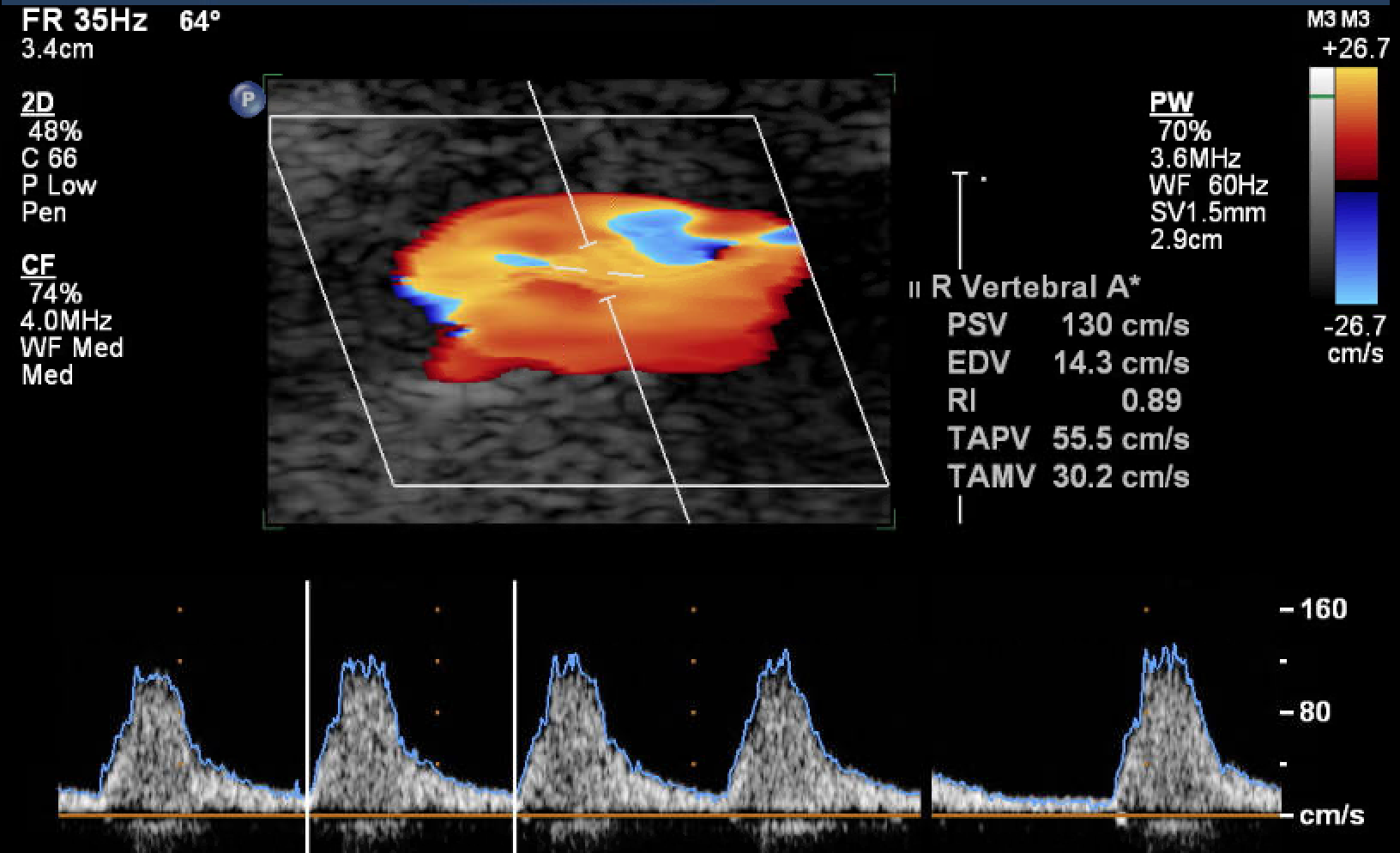
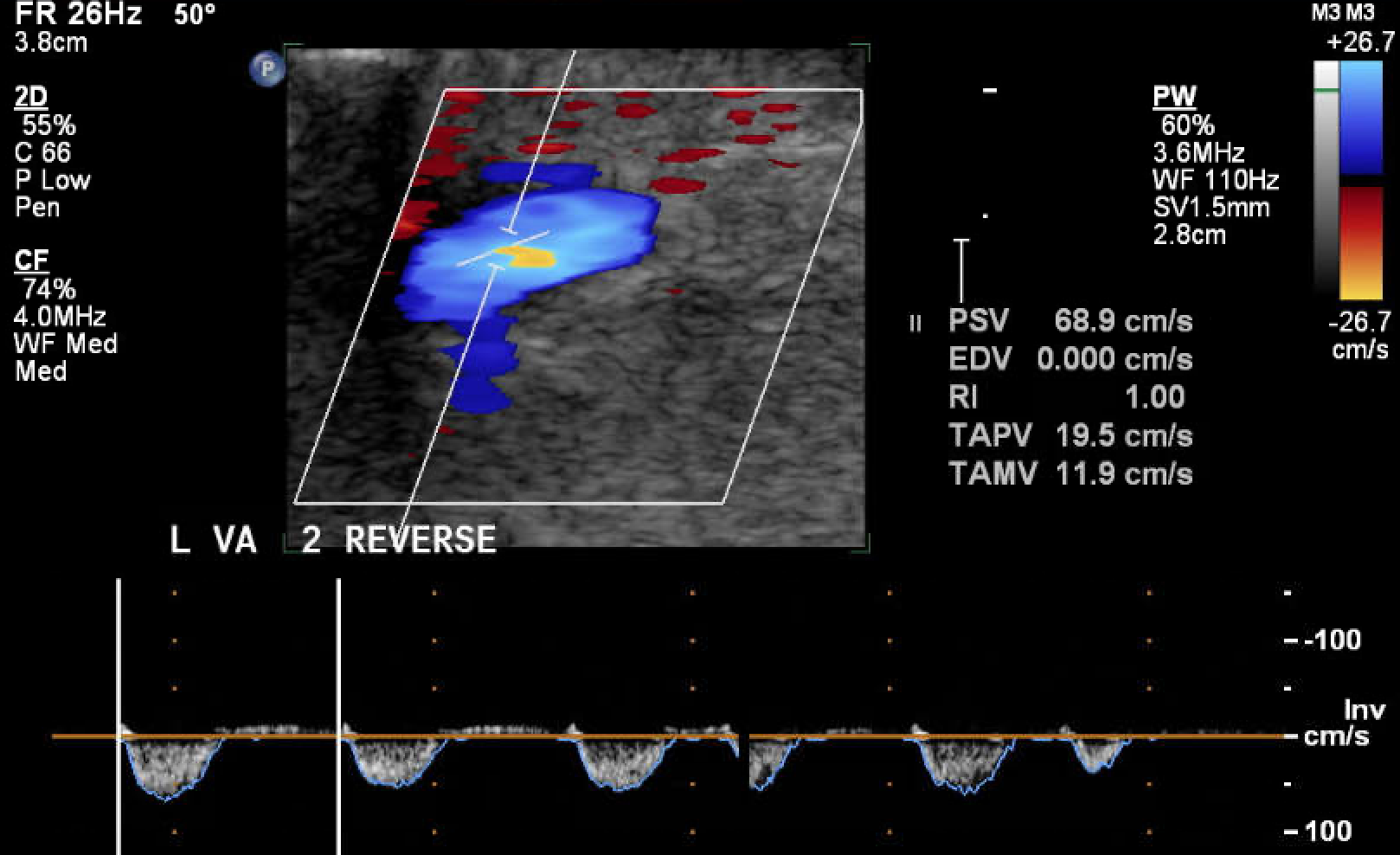
Doppler ultrasonography showed reversed flow in the left vertebral artery with the monophasic waveform in the left subclavian artery, indicating stenosis in the left proximal subclavian artery with subclavian steal phenomenon.
Relevant Catheterization Findings
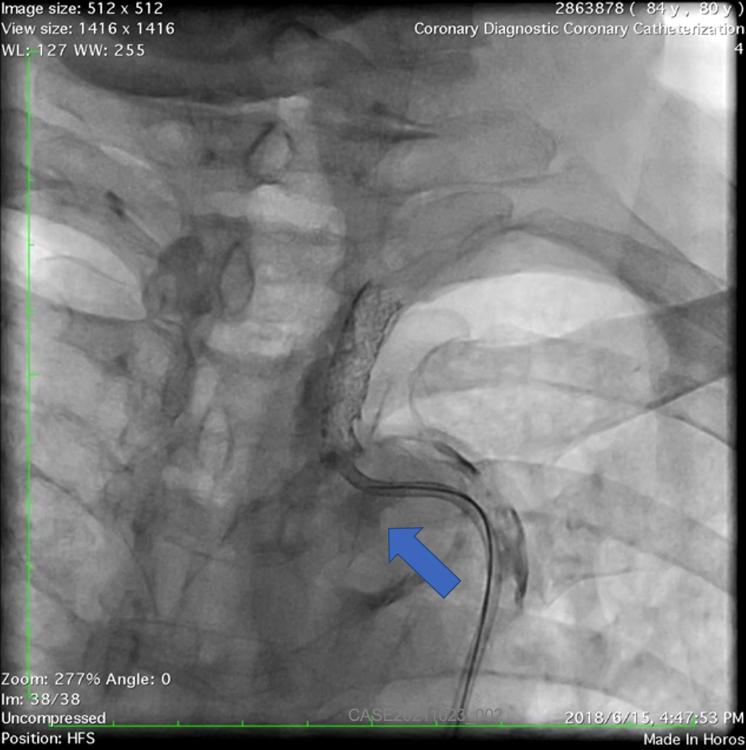
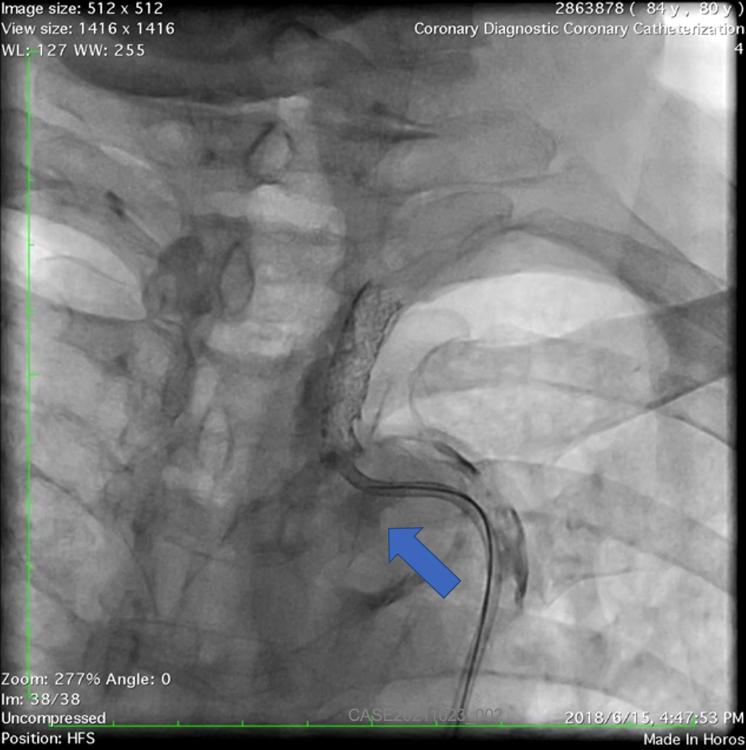
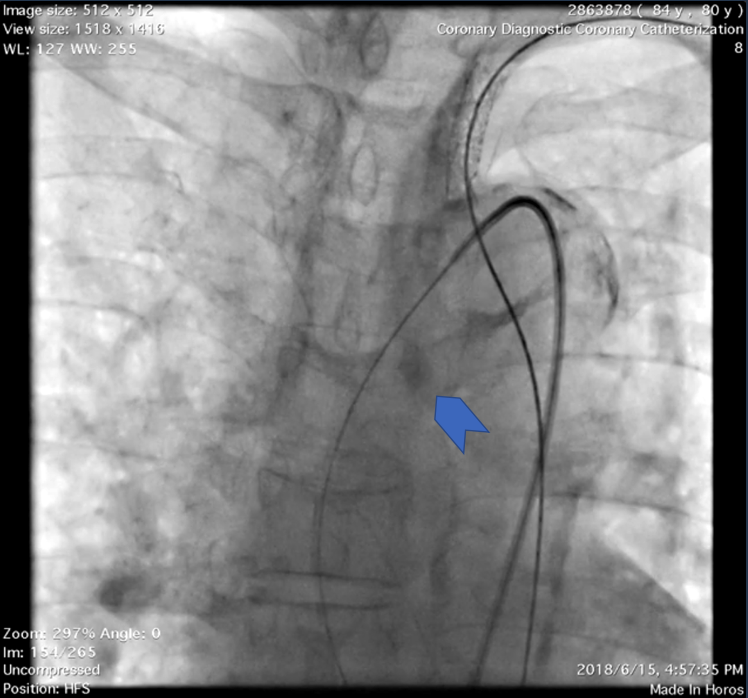
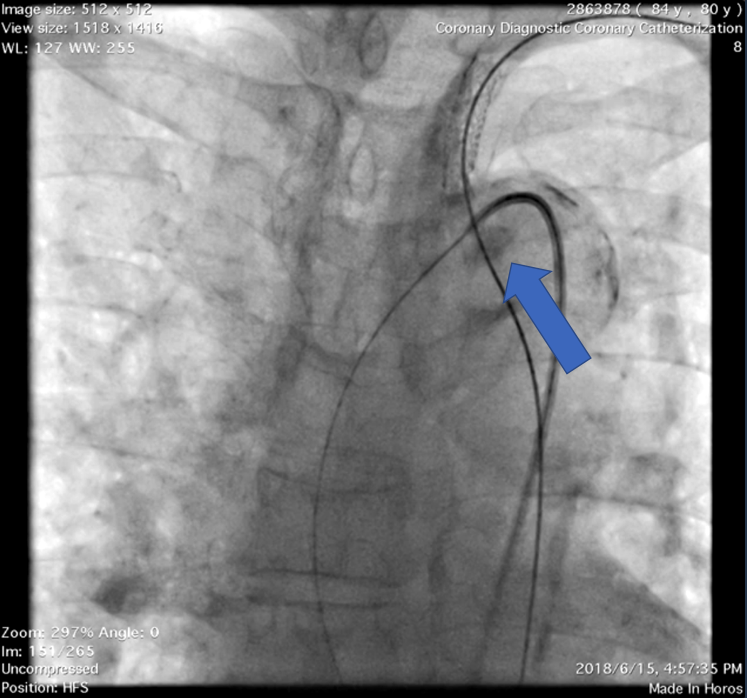
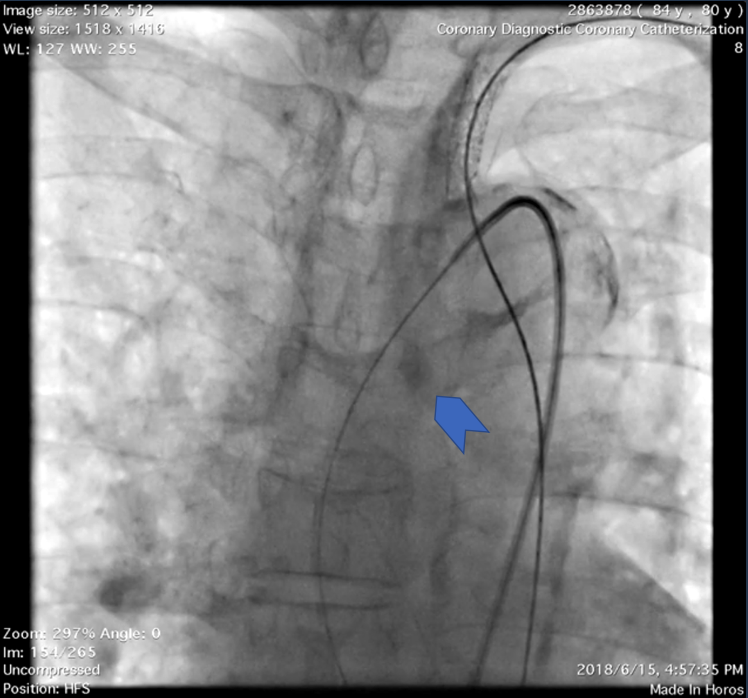
Angiography disclosed left SA ostial in-stent restenosis. A large calcified atheroma was noticed near left subclavian artery orifice (Figure 1).
Interventional Management
Procedural Step
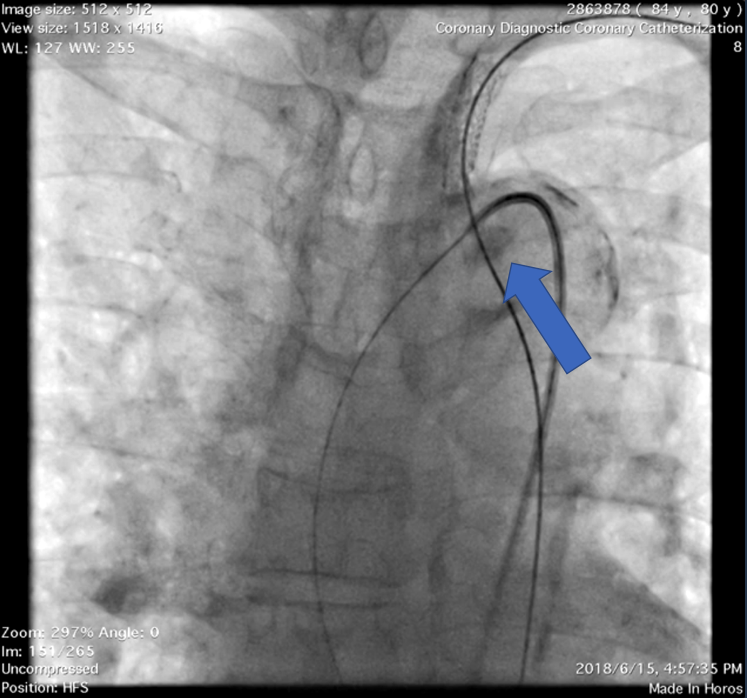
A JR4 guiding catheter was used trans-femorally to engage to left SA ostium but failed. The left radial artery was cannulated and retrograde wiring across the SA stent was successful. During manipulation, the patient developed acute neurological deficits, including aphasia and right hemiparesis. Cerebral embolization with acute stroke to the left hemisphere was suspected according to neurological localization. Unfortunately, the previous stable aortic plaque became partially mobile with a distinctive “shaking” motion pattern. The shaking plaque then broke off during the advancement of the diagnostic catheter into the left common carotid artery. It dislodged and was flushed from the arch to descending aorta (Figure 2a, 2b). Left middle cerebral artery occlusion at M1 was confirmed immediately with cerebral angiography (Figure 3), and intra-arterial thrombectomy was executed successfully.


Case Summary
Careful evaluation of the aortic plaque morphology and distribution is crucial in any procedure involving the aortic arch. When ominous sign with shaking aortic plaque is observed, termination of any further procedure should be seriously considered to avoid ensuing disaster.