Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-061
Left Atrial Appendage Occlusion With the WATCHMAN Device: Peri-Procedural Outcomes From the Prospective, Multicenter RECORD Registry
By Chao Gao, Fangju Su, Jianzheng Liu, David R. Holmes, Patrick W. Serruys, Ling Tao
Presenter
Chao Gao
Authors
Chao Gao1, Fangju Su1, Jianzheng Liu1, David R. Holmes2, Patrick W. Serruys3, Ling Tao1
Affiliation
Xijing Hospital, China1, Mayo Clinic, USA2, University of Galway, Ireland3
View Study Report
TCTAP A-061
Left Atrial Appendage Closure
Left Atrial Appendage Occlusion With the WATCHMAN Device: Peri-Procedural Outcomes From the Prospective, Multicenter RECORD Registry
Chao Gao1, Fangju Su1, Jianzheng Liu1, David R. Holmes2, Patrick W. Serruys3, Ling Tao1
Xijing Hospital, China1, Mayo Clinic, USA2, University of Galway, Ireland3
Background
Left atrial appendage occlusion (LAAO) has emerged as an alternative to anticoagulation for atrial fibrillation patients with contraindications or unsuitable for long-term oral anticoagulants. However, the performance of LAAO among East Asians is to be investigated. In the current study, we aimed to document the real-world procedural success rate and configurations, major adverse event rates, and antithrombotic medication regimens peri- and post-LAAO.
Methods
A total of 3,096 consecutive patients from 39 Chinese centers undergoing LAAO between was prospectively enrolled between 1st April 2019 and 31st October 2020.
Results
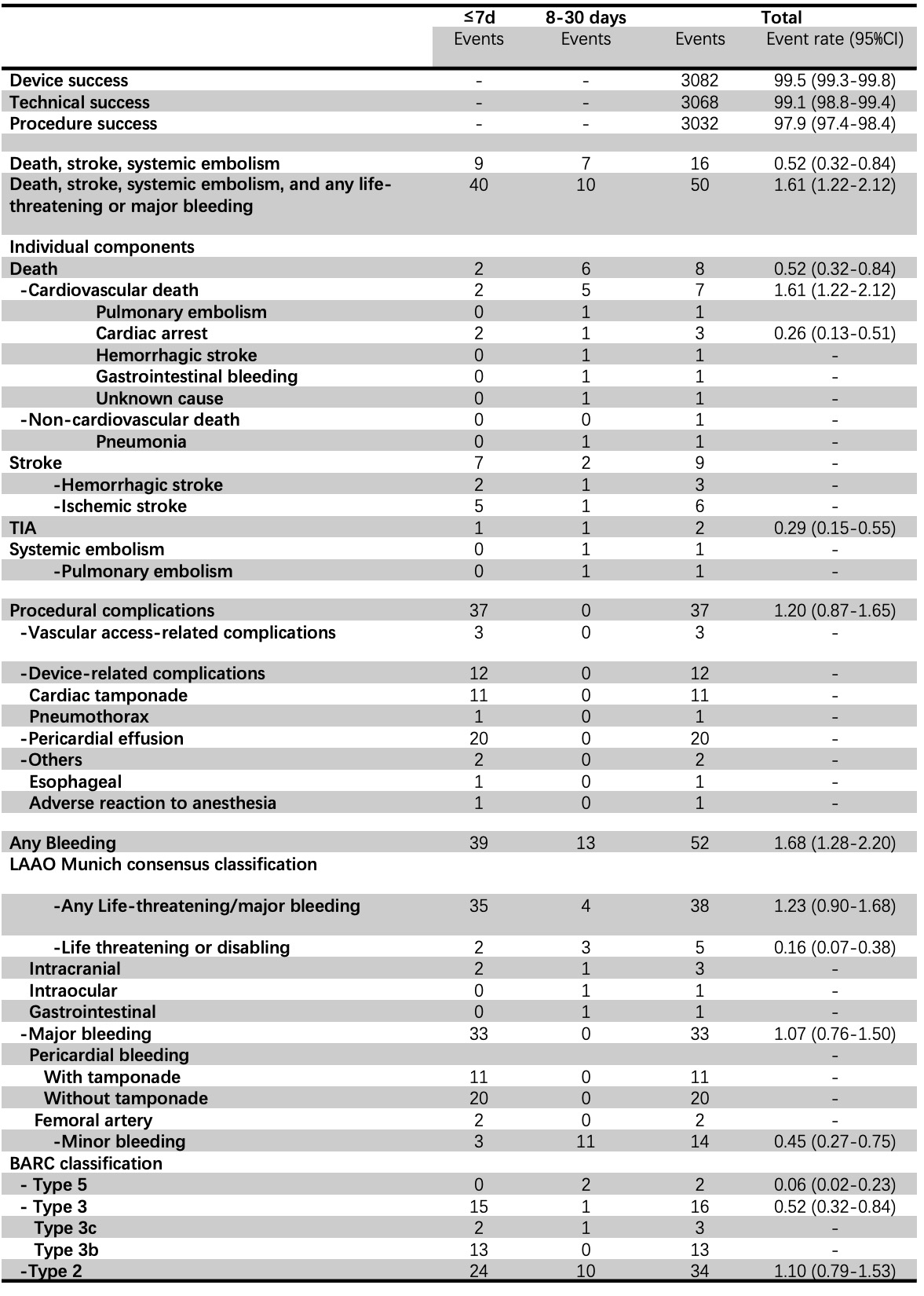
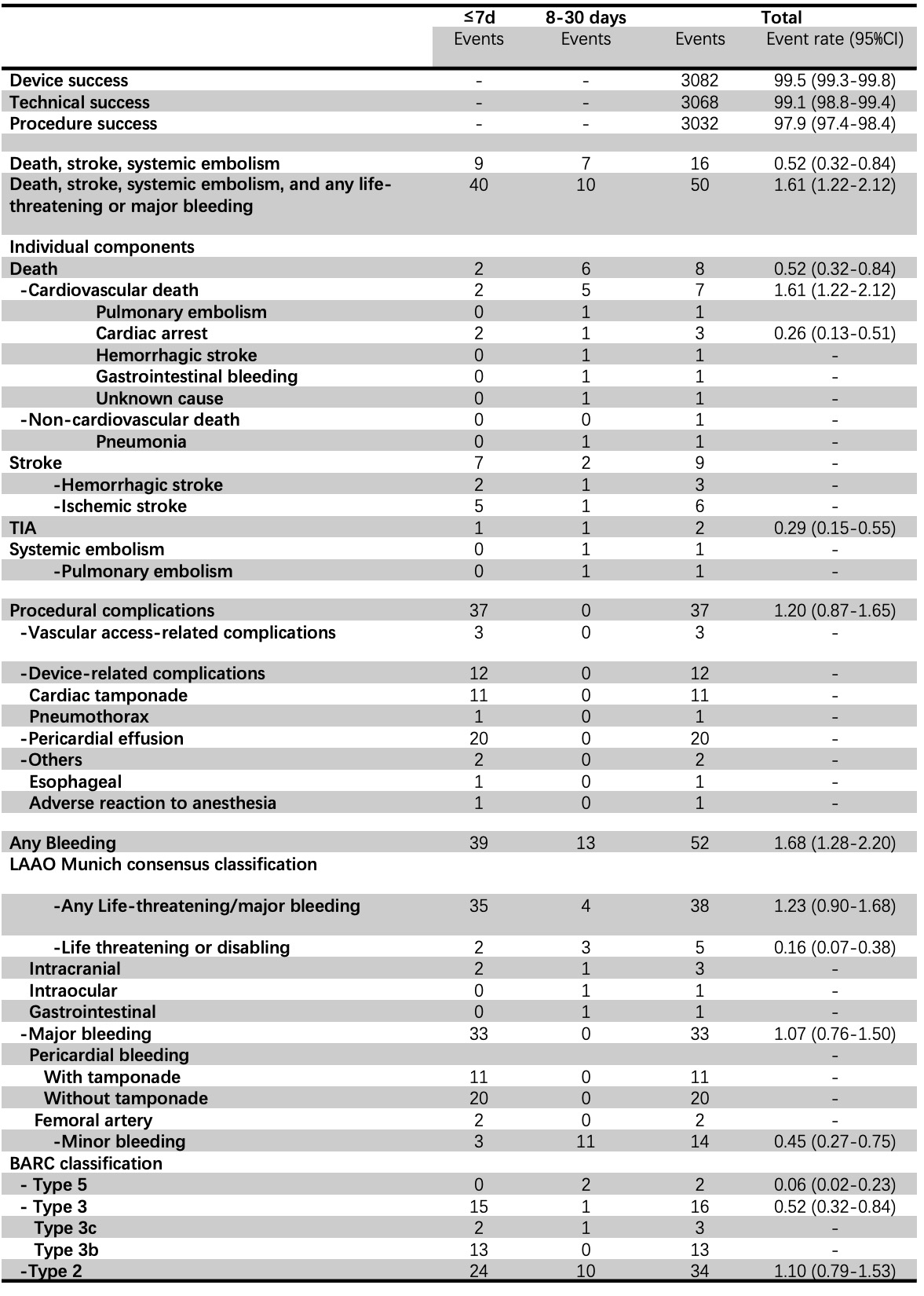
Enrolled participants had a high risk of stroke (CHA2DS2-VASc:4.0±1.8), a moderate-to-high risk of bleeding (HAS-BLED score:2.4±1.2). The number of procedures performed under local anesthesia was 1,287 (41.6%), while 493 (15.9%) used only fluoroscopy guidance. In 41.9% of cases, LAAO implantation was combined with radiofrequency ablation or cryoablation for atrial fibrillation. Device and procedural success were achieved respectively in 99.5% (3,082/3,096) and 97.9% (3,032/3,096) of cases. At 30-day follow-up, the rate of the composite endpoint of death, stroke, and systemic embolism was 0.52% (95%CI:0.32-0.84), and any life-threatening/major bleeding 1.23% (95%CI:0.90-1.68). The types of anesthesia (general/local), intra-procedural imaging (transesophageal echocardiography/fluoroscopy/intracardiac echocardiography), or whether a combined ablation procedure was performed or not, had no significant impact on the procedural success or 30-day adverse events. Procedural success was significantly higher (98.2% versus 96.5%, ORadjusted:1.97, 95%CI:1.01-3.53, P=0.023) and life-threatening or major bleeding significantly lower (2.5% versus 1.0%, ORadjusted: 0.42, 95%CI:0.21-0.87, P=0.019) in centers performing ≥40 versus <40 cases annually.
Conclusion
In Chinese centers, patients with a high risk of stroke and moderate-to-high risk of bleeding who underwent implantation of a WATCHMAN LAAO device had high rates of procedural success and low rates of short-term ischemic and bleeding events.