Lots of interesting abstracts and cases were submitted for TCTAP 2022. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-065
Percutaneous Coronary Intervention in Elderly Population : Asian Perspective
By Quah Wy Jin, Mugilan Sundarajoo, Jayakhanthan Kolanthaivelu
Presenter
Quah Wy Jin
Authors
Quah Wy Jin1, Mugilan Sundarajoo2, Jayakhanthan Kolanthaivelu3
Affiliation
National Heart Institute, Malaysia1, National Heart Institute Ijn, Malaysia2, Cardiovascular Sentral Kuala Lumpur, Malaysia3
View Study Report
TCTAP A-065
Others (Unclassified)
Percutaneous Coronary Intervention in Elderly Population : Asian Perspective
Quah Wy Jin1, Mugilan Sundarajoo2, Jayakhanthan Kolanthaivelu3
National Heart Institute, Malaysia1, National Heart Institute Ijn, Malaysia2, Cardiovascular Sentral Kuala Lumpur, Malaysia3
Background
Definition of elderly varies amongst countries worldwide especially in studies on percutaneous coronary intervention (PCI). According to the guidelines, elderly was defined as patients more than 75 years of age which is the cut-off for this study. PCI in the elderly carries high risk of morbidity and mortality. However with advent of newer generation of drug eluding stents, increase usage of radial access and better understanding of antithrombotic therapies, there has been a trend towards reduction of cardiac mortality and improvement in quality of life. However , this group of patients are often excluded from most trials and there are lacking of data in regards to outcome and safety of PCI in this group. Hence we aim to look mainly at the outcome and safety of PCI in this group.
Methods
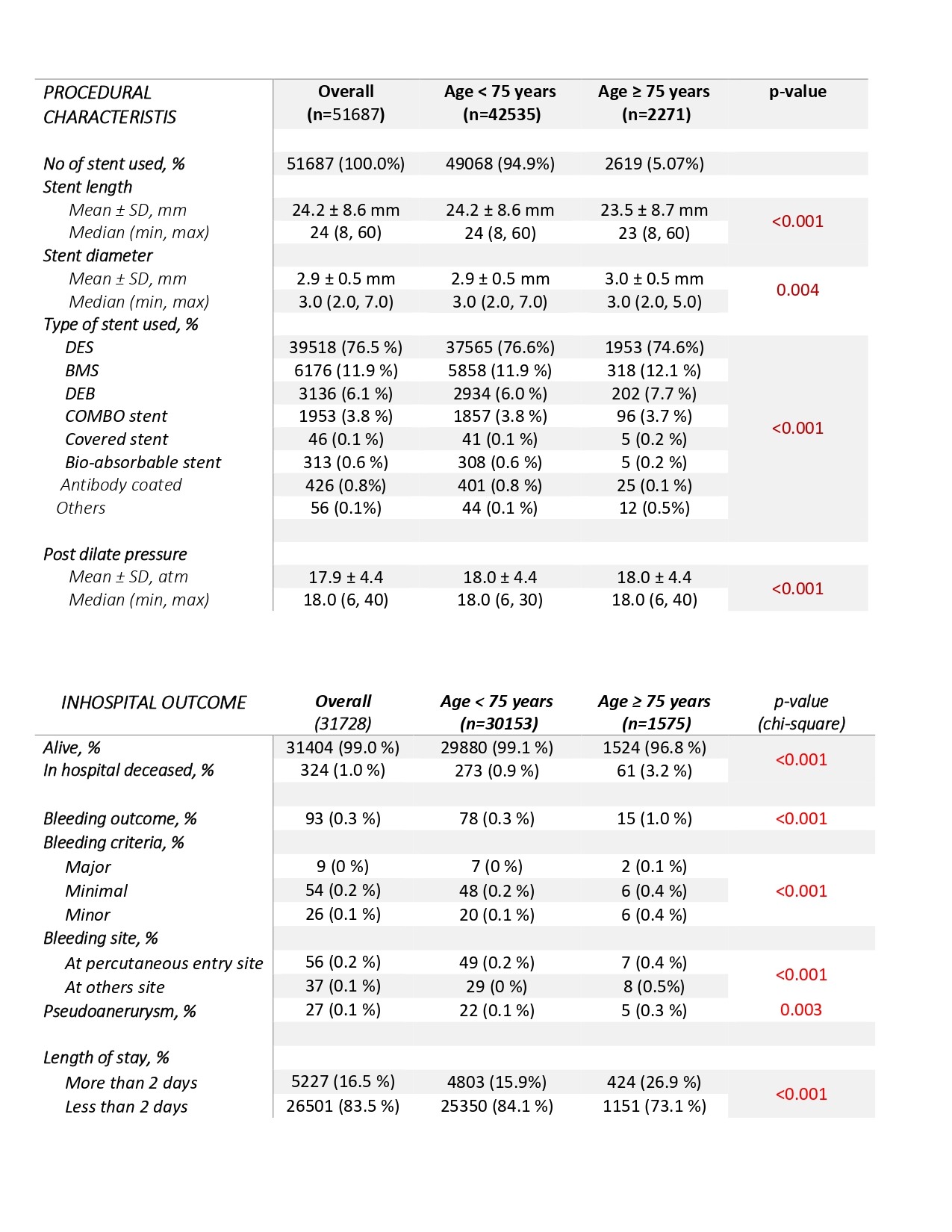
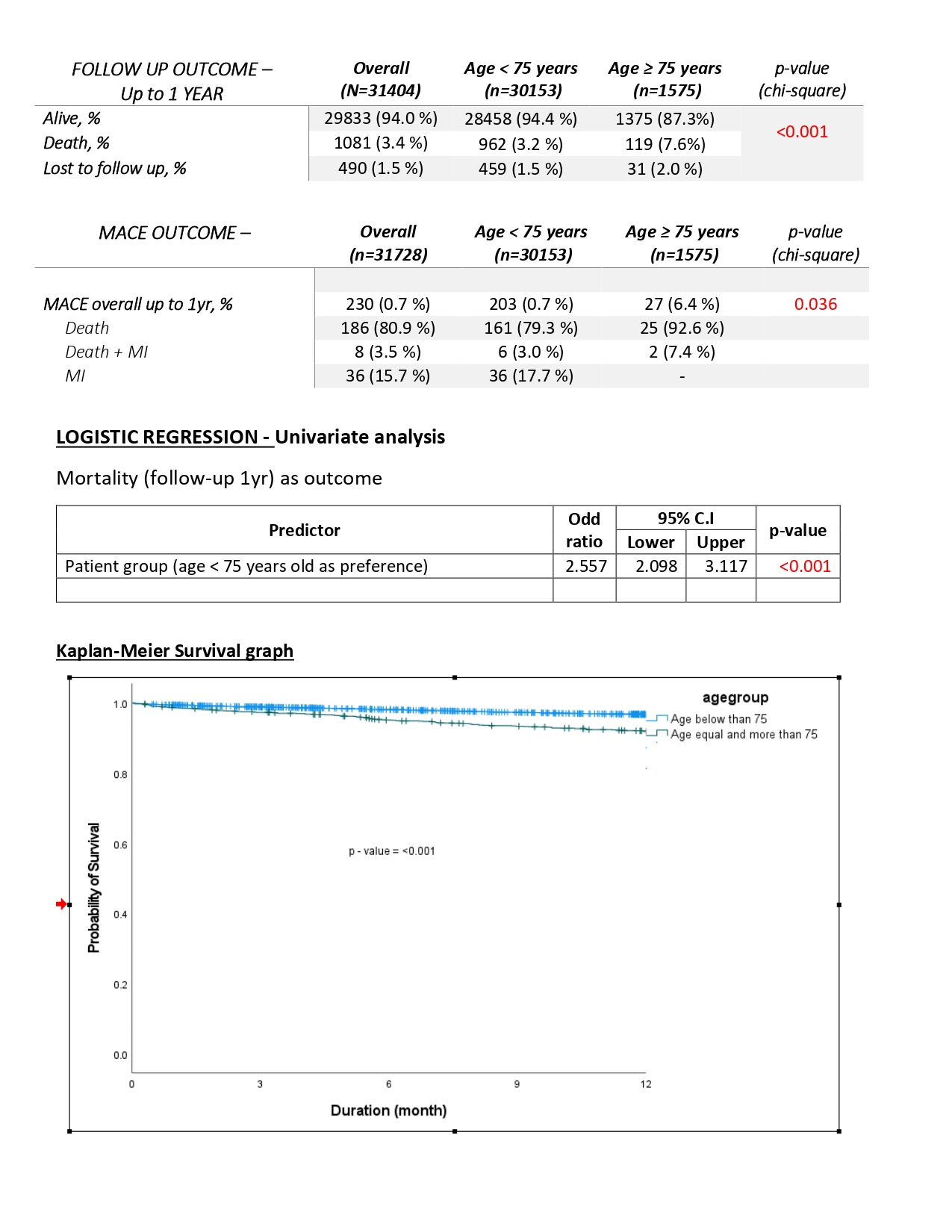
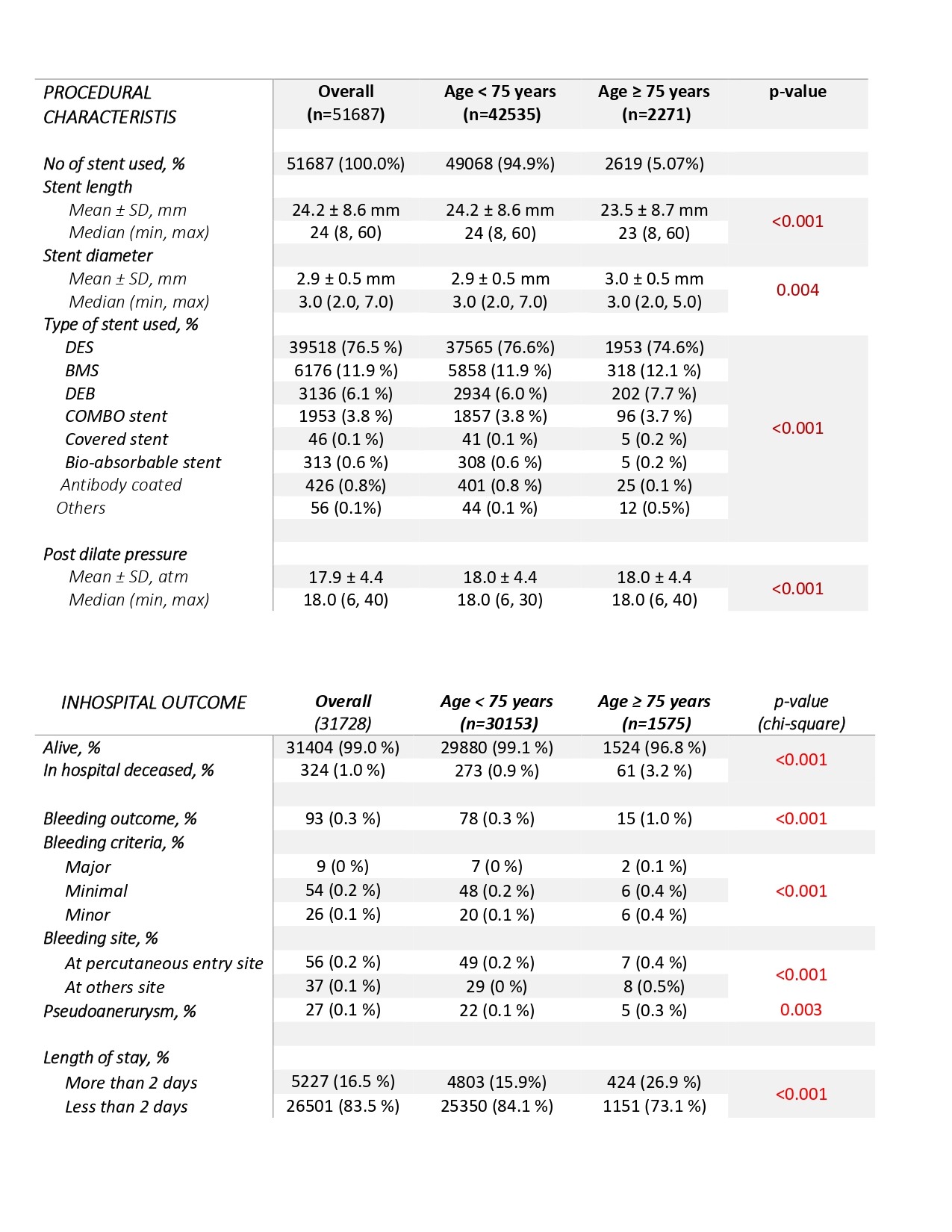
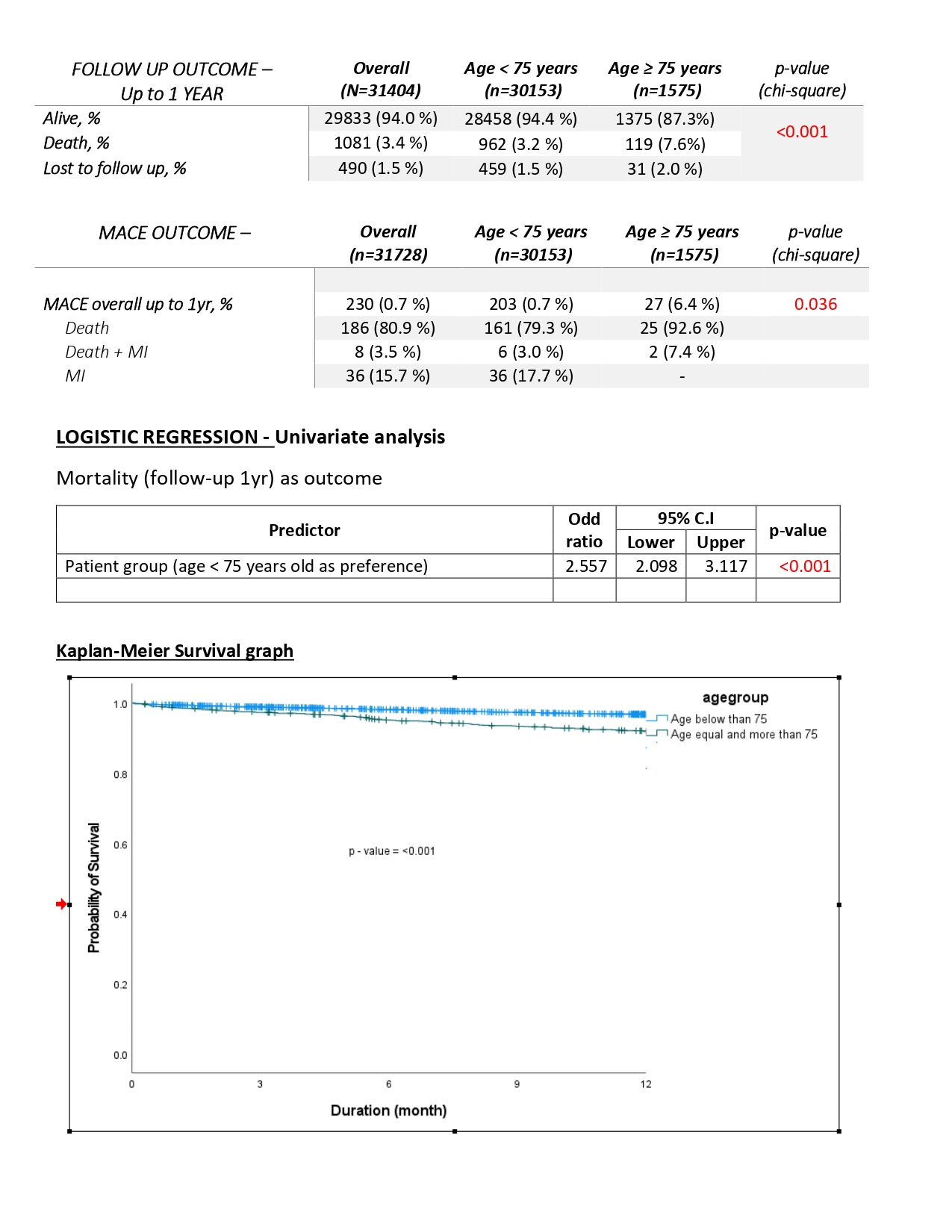
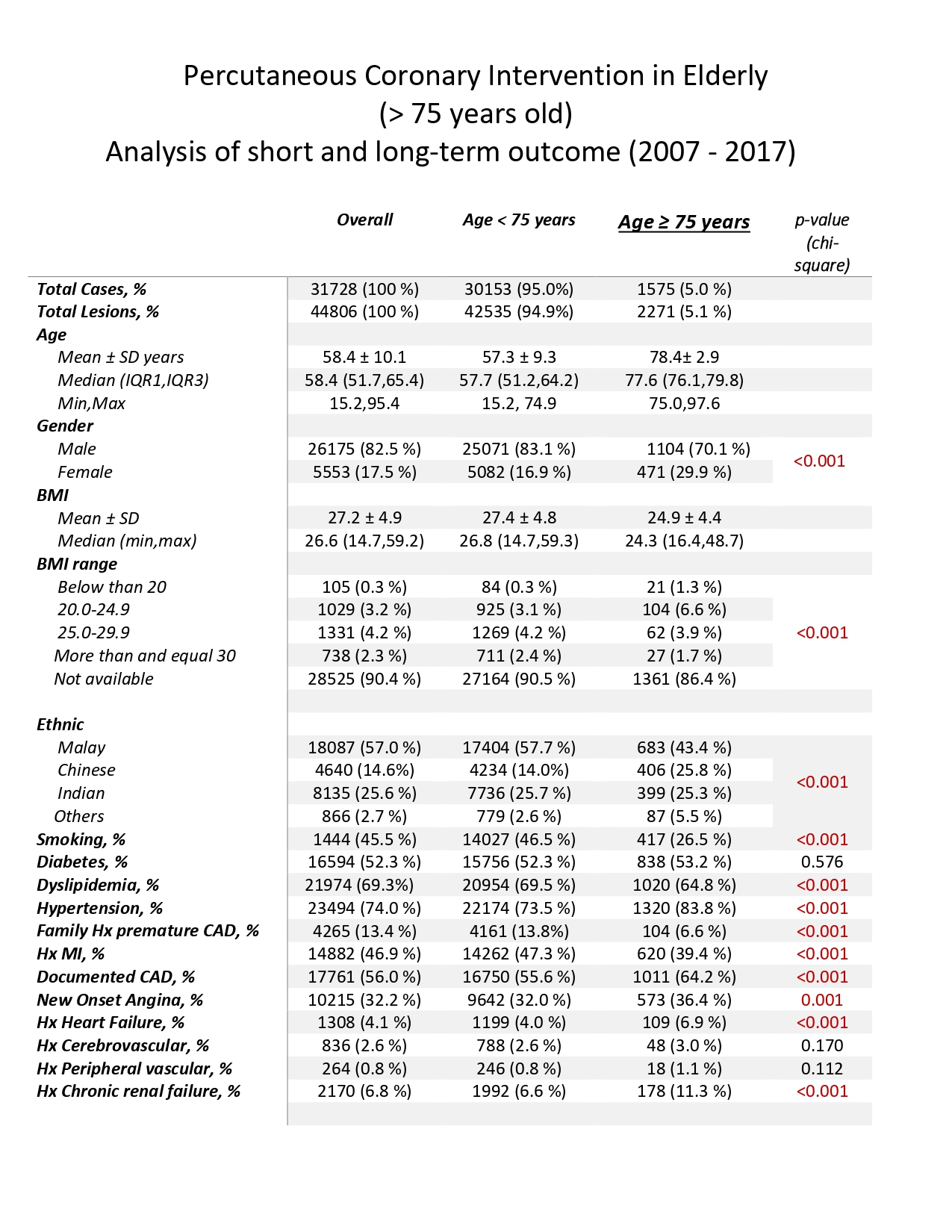
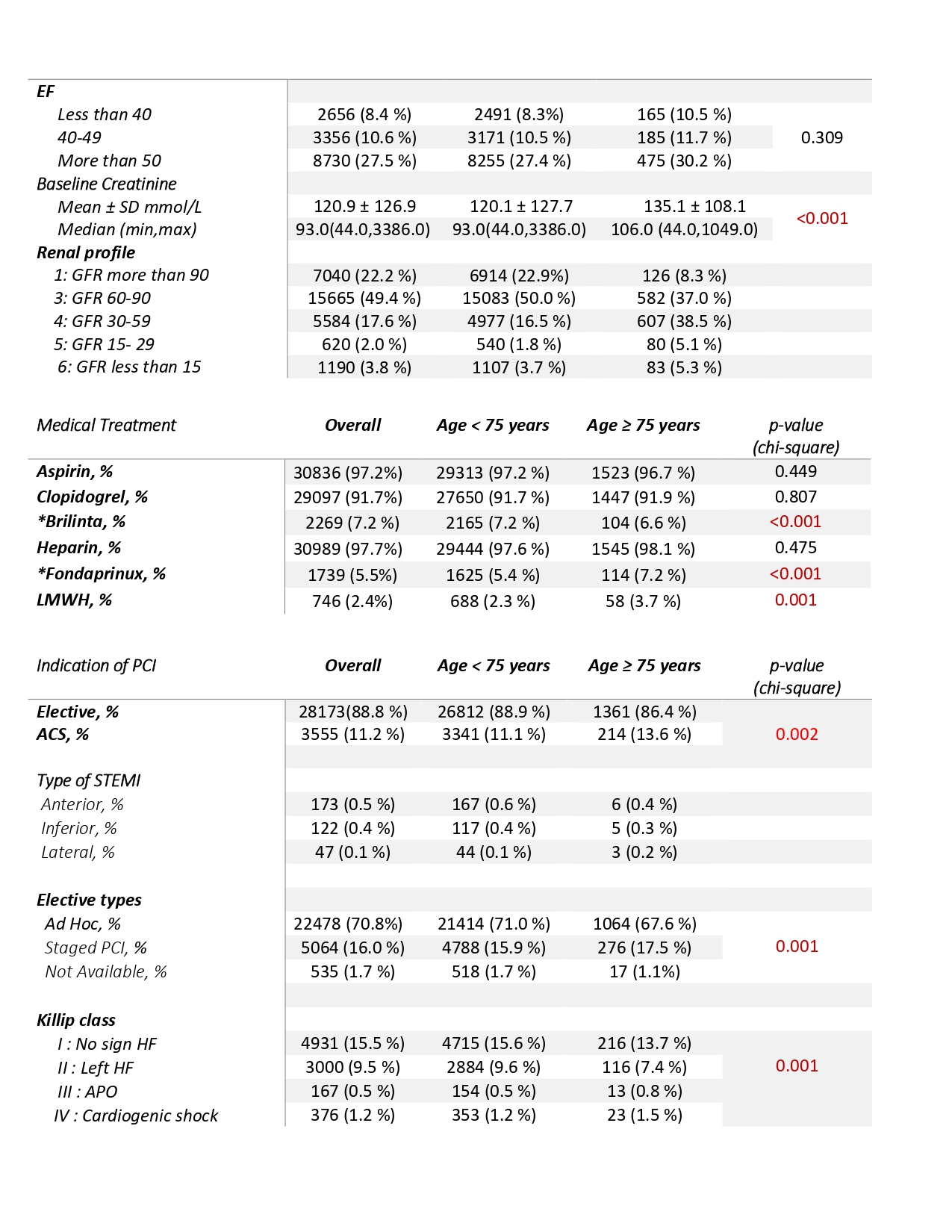
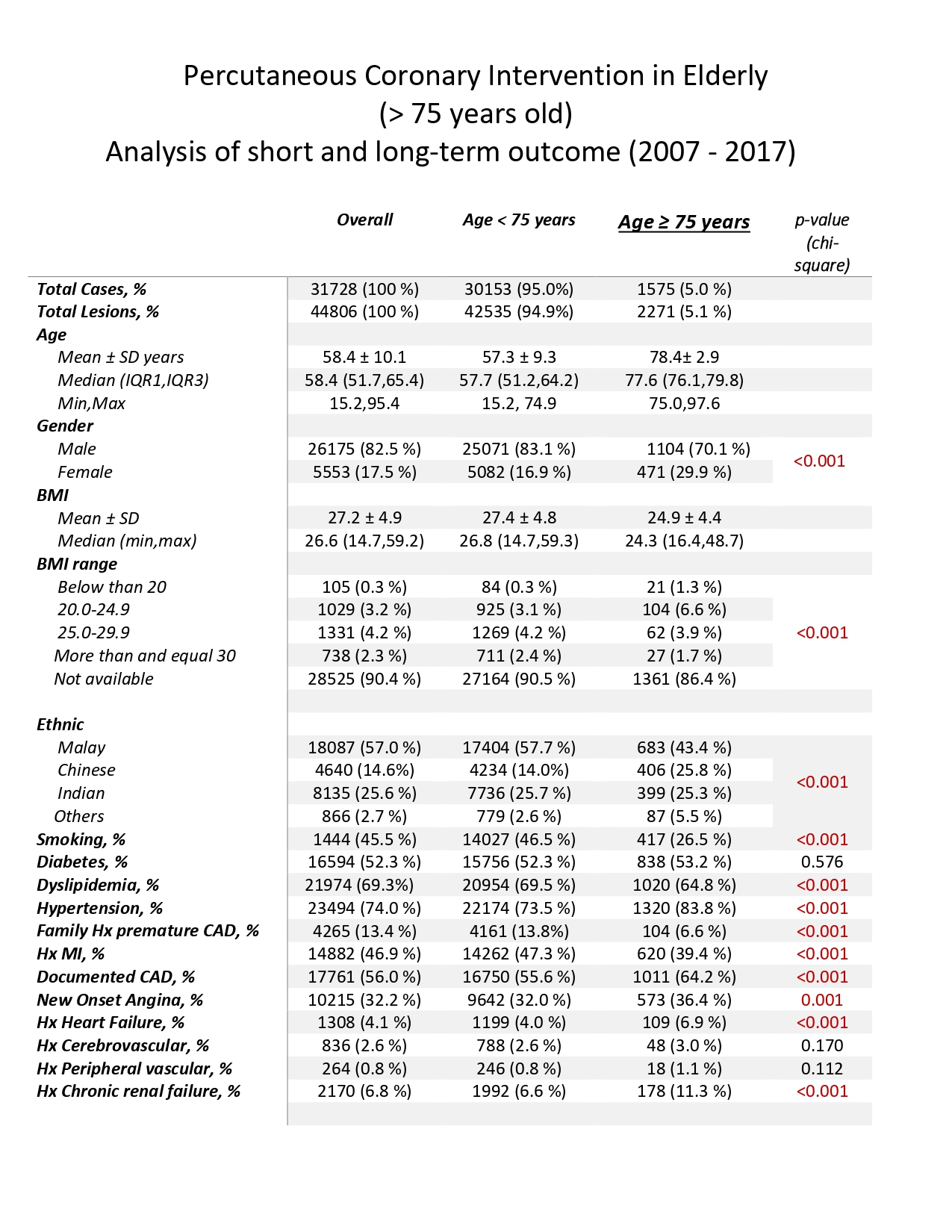
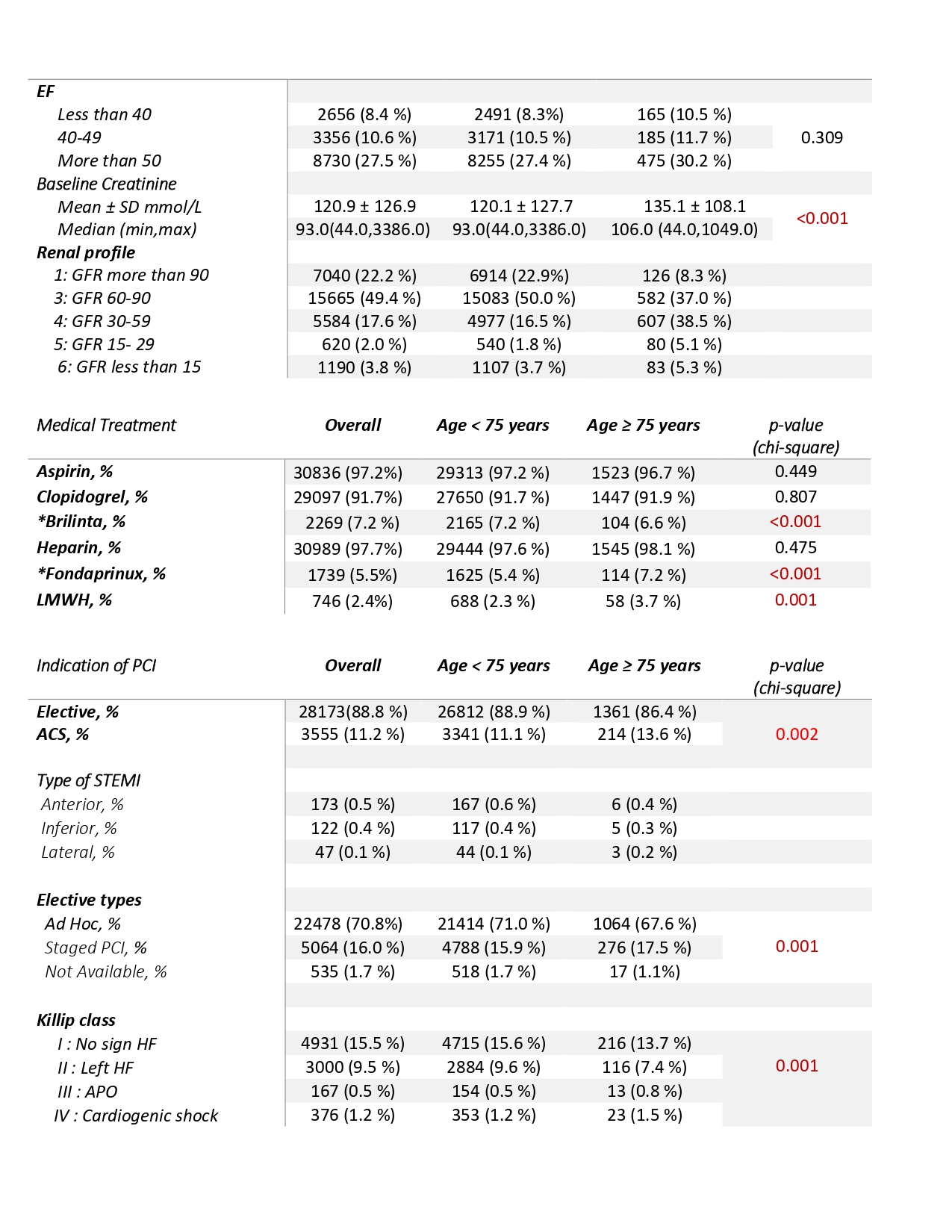
This is an observational retrospective analysis. 1575 patients whose age was equal or more than 75 years old (5% of total PCI cases) admitted in the National Heart Institute from January 2007 till December 2017 were included in this study. Patients' demographics, risk factors and procedural characteristics were evaluated. Comparison was made with the patients of age less than 75 years old (main group) in terms of hospitalization and 1 year follow-up outcome. Multivariate logistic regression analysis performed with Kaplan-Meier survival graph plotted.
Results
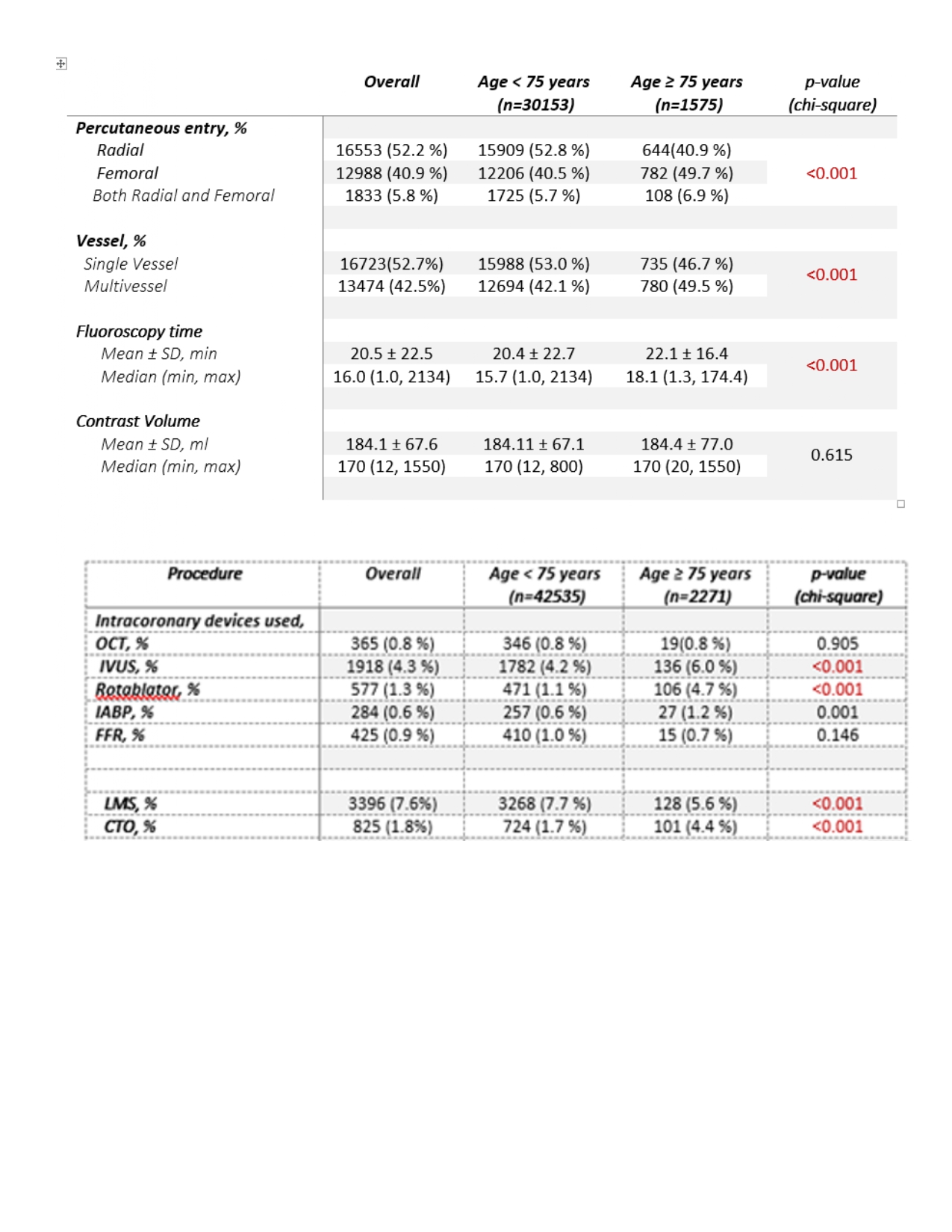
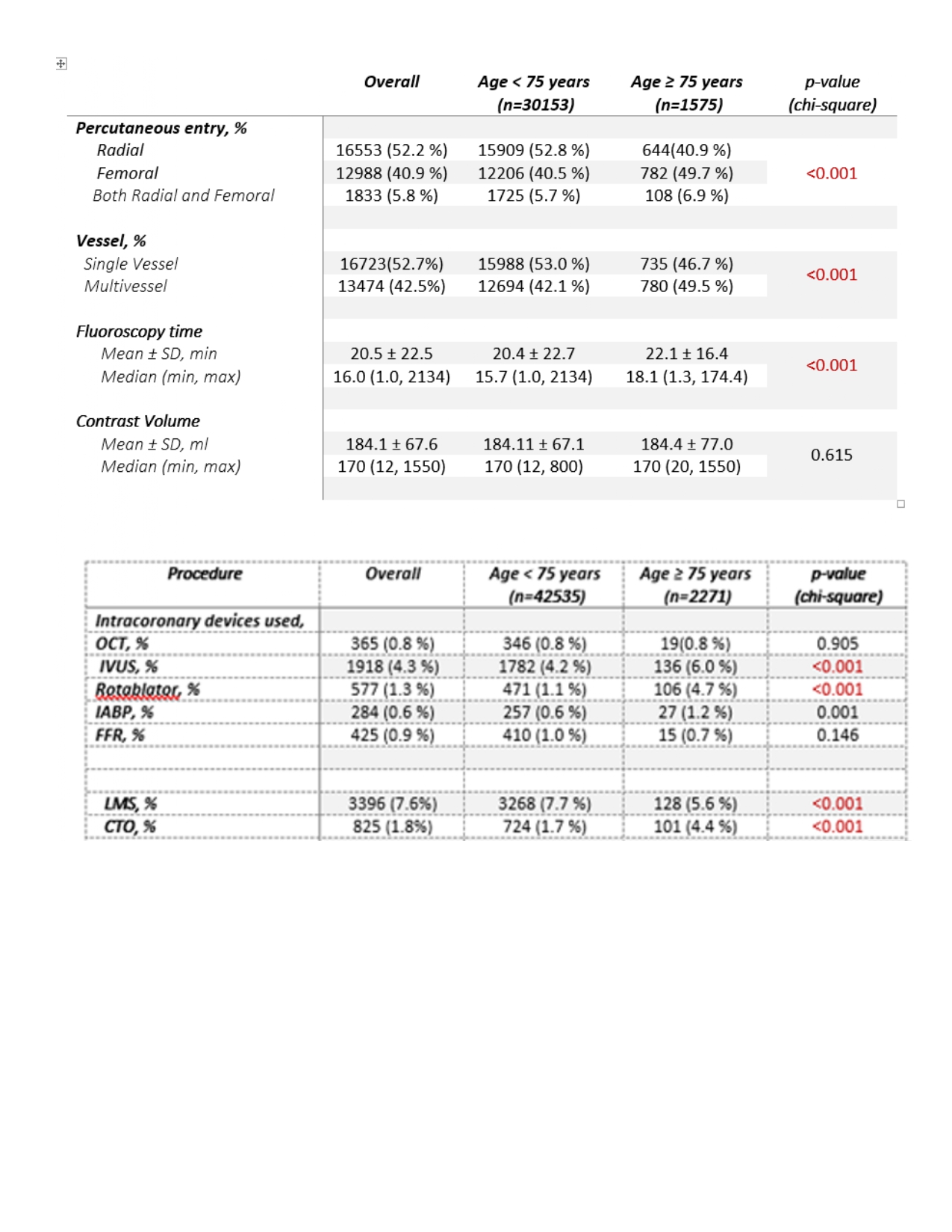
Over period of 11 years, 1575 patients were analyzed. Mean age was 78.4 +/- 2.9 years old. Minimum age was 75 whereas the oldest patient was 97 years old. Patients were predominantly male (70.1%) with female (29.9%) but significantly more females than the main group (p < 0.001). Race was mainly Malay (43.4%), Chinese (25.8%) then Indian (25.3%). The elderly group has more patients with hypertension (83.8%), history of CAD (64.2%), heart failure (6.9%) and chronic kidney disease (11.3%). The PCI indication of acute coronary syndrome (ACS) was 13.6% for elderly group vs 11.1% for main group while elective procedures favored the main group (88.9%) over the elderly group (86.4%). In regards to vascular access, femoral access alone was significantly more in elderly group (49.7 %) compared to main group (40.5%) with a p value of < 0.001. Multi-vessel disease (MVD) is more common in elderly group (49.5%) than main group (42.1%). Intravascular ultrasound (IVUS), rotational atherectomy (RA) and intra-aortic balloon pump (IABP) were used significantly more in the elderly group compared to the main group (p value < 0.001). Fluoroscopy time was longer too in elderly group (p < 0.001) with no significant difference between the contrast volume (p value 0.615). The elderly group had worse in-hospital outcome than the main group (3.2 % Vs 0.9%) with higher bleeding outcome (1% Vs 0.3%). Naturally, the hospital stay was longer as well in this older group of patients (26.9% Vs 15.9%). During follow up till 1 year, outcome was poorer for the elderly group compared to the rest (7.6% Vs 3.2%) with significant (p value of 0.036) overall MACE (Major Adverse Cardiovascular Events) . Thus, mortality at 1 year follow up is higher (odds ratio, 2.557; 95% CI, 2.098 - 3.117) in this elderly group. In terms of in hospital outcome, it was also noted that the number of cardiac deaths were higher, respectively 80.4% (41 patients) in elderly group and 86.8% (237 patients) in main group (< 75 years old) but there was no significant difference between both groups (p value of 0.403).
Conclusion
In our study, the elderly group had poorer outcome during in hospital stay and at follow up up till 1 year. This finding is consistent with the J-PCI registry of more than half a million patients by Yohei Numasawa et al. This is likely due to more patients having multi- vessel disease, significantly higher number of bleeding events with femoral punctures in comparison with the main group and longer hospital stay. Therefore, age does play an important prognostic role. In contrast to other studies, the number of non cardiac deaths were lower than cardiac deaths in the elderly group. This elderly group also consists of CHIP-PCI cases whereby patients have poor LVEF, chronic renal failure, significantly high CTOs, more use of IABP and rotational atherectomy. Antithrombotic therapy was another interesting aspect of PCI in elderly as we noticed Ticagrelor (Brilinta) was used lesser but yet bleeding events were higher. Use of drug eluting stents (DES) and drug coated balloons (DEB) were comparable between both groups. Generally, it is widely known that elderly patients are typically treated less aggressively compared to their younger counterparts due to the concern of higher mortality which is clearly seen in this study. However, decision to perform PCI should be individualized as there are other studies which have proven good long term outcomes especially in specific clinical situations such as STEMI (PAMI-I, GUSTO-IIB and DANAMI-2 trials) and NSTEMI (TACTICS-TIMI 18). In regards to elective cases such as in our study, the TIME trial has taught us that there is still benefit in regards to relief of angina and improvement in quality of life. In our study, most of the elective cases were symptomatic and had functional studies done to assess for ischemia before proceeding for PCI. Overall, many societies such as AHA, ESC and SCAI have recommended patient-centered approaches for PCI in the elderly group therefore age should not be the sole factor in making such a crucial decision.