Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-109
Managing (Almost) Every Procedural Complication Imaginable - A Case of Right Coronary Artery Orbital Atherectomy
By Catherine Jillian Hardi, Sunanto Ng
Presenter
Catherine Jillian Hardi
Authors
Catherine Jillian Hardi1, Sunanto Ng1
Affiliation
Universitas Pelita Harapan, Indonesia1,
View Study Report
TCTAP C-109
CORONARY - Complications (Coronary)
Managing (Almost) Every Procedural Complication Imaginable - A Case of Right Coronary Artery Orbital Atherectomy
Catherine Jillian Hardi1, Sunanto Ng1
Universitas Pelita Harapan, Indonesia1,
Clinical Information
Patient initials or Identifier Number
SHLV01052616
Relevant Clinical History and Physical Exam
A 63 year old female presented with a chief complaint of angina CCS grade 3 and dyspnea on exertion. Her comorbidities were controlled hypertension. Her current medications were Aspirin 80 mg OD, Clopidogrel 75 mg OD, Atorvastatin 40 mg OD. She denied family history of coronary artery disease. She looked frail and weighed 45 kg. Her cardiopulmonary examination was normal. Non-contrast CT scan of the thorax showed a hyperdense lesion observed on the projection of the right coronary artery.
Relevant Test Results Prior to Catheterization
Her 12-lead ECG showed normal sinus rhythm with no Q waves and no ST segment and T wave deviation. Echocardiography showed normal left ventricular function and no regional wall motion abnormalities.
Relevant Catheterization Findings
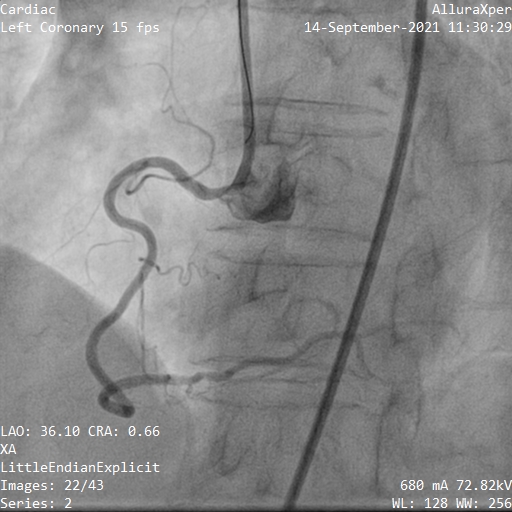
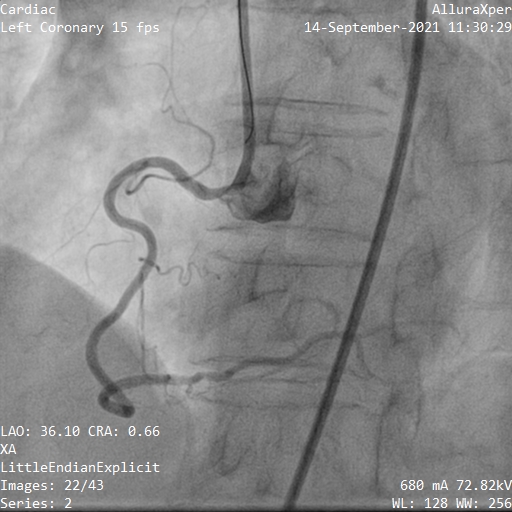
Angiography showed calcified stenosis to osteal RCA and non-significant lesions to distal RCA and proximal LAD. PCI targeted the osteal RCA lesion, with the remaining lesions to be managed conservatively.
Interventional Management
Procedural Step
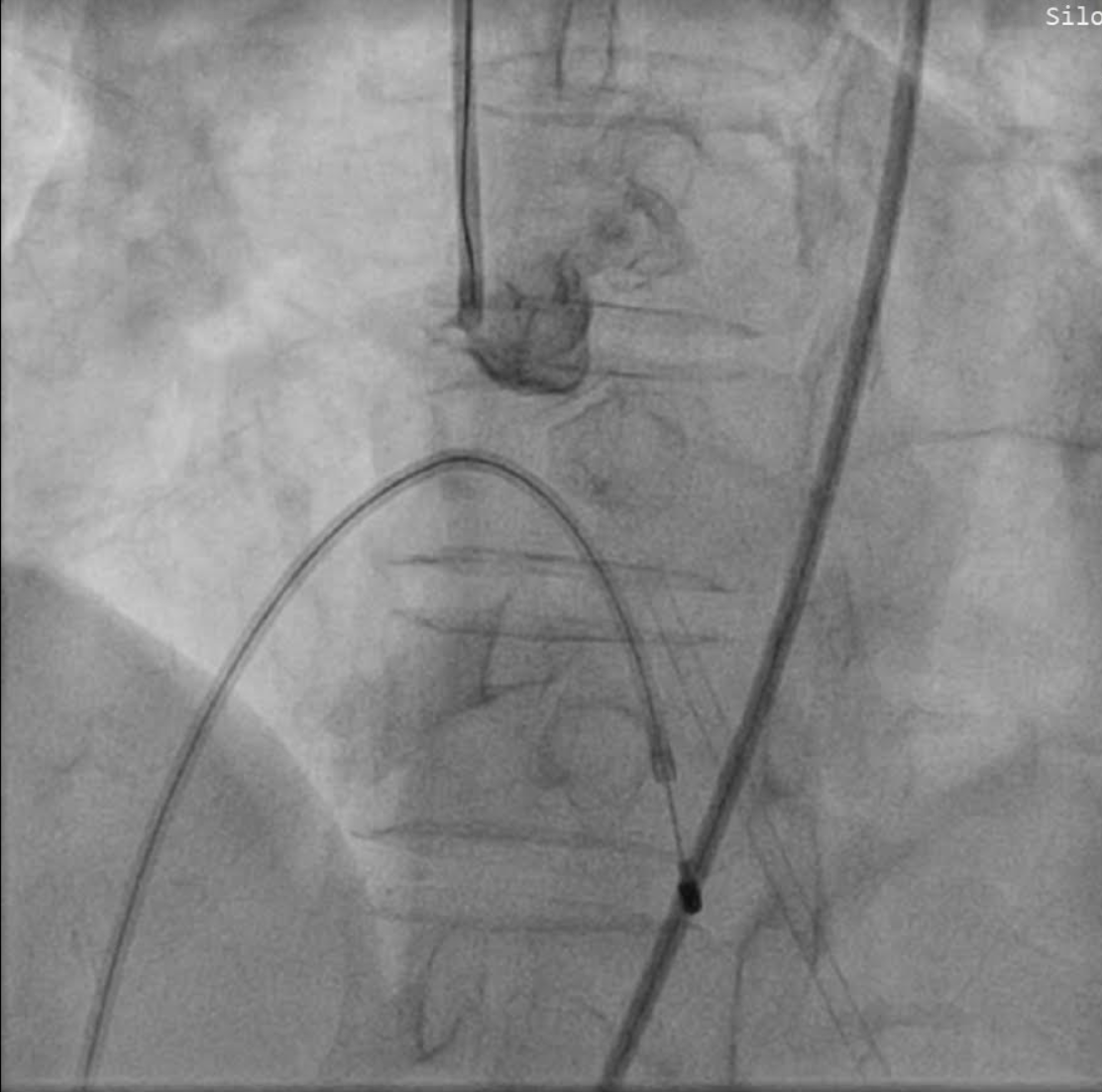
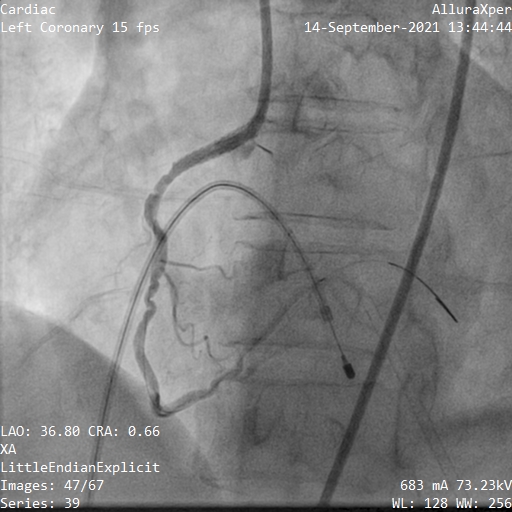
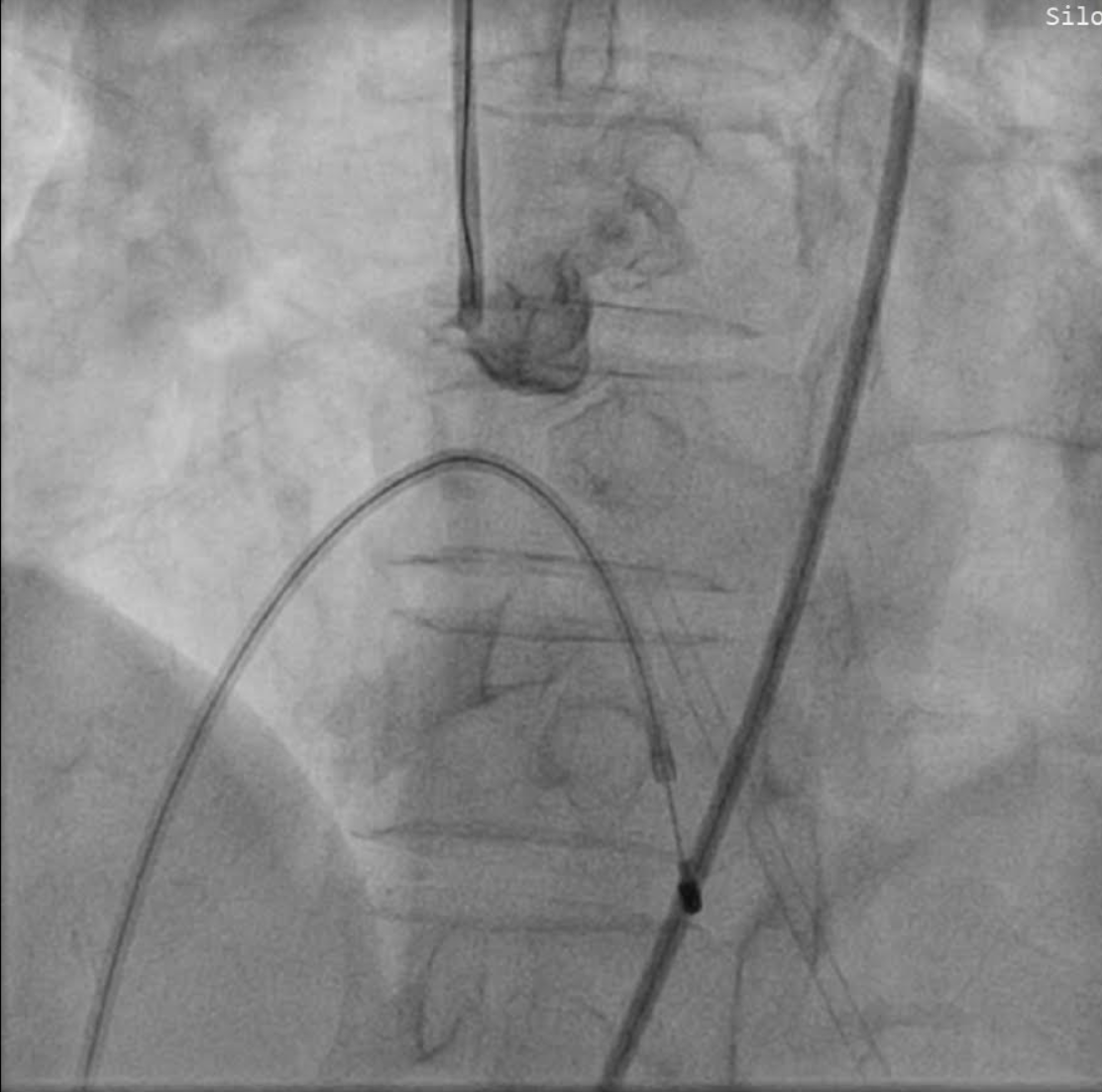
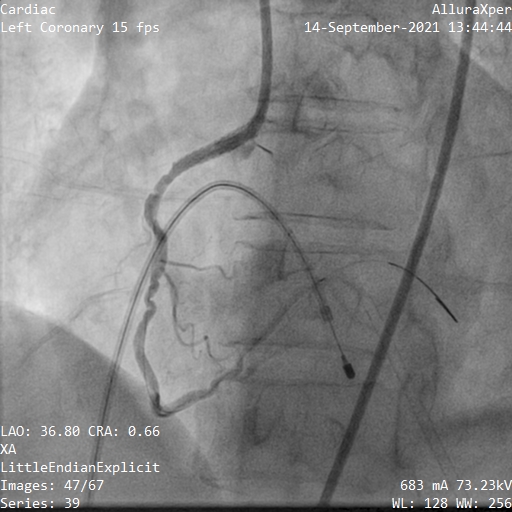
Guiding catheter used JR 3.5/7F. Initially, IVUS (Volcano Therapeutics, USA) did not cross due to severe calcification. Orbital atherectomy used Diamondback® OAS (CSI, USA) with 1 antegrade and 1 retrograde run. Post retrograde run, she was agitated and felt chest discomfort. Angiography showed aortocoronary dissection. In attempting to exchange wires, the Viper wire lost engagement. While re-wiring, she developed unstable bradycardia. Temporary pacemaker was implanted. Still unstable, echocardiography showed pericardial effusion. Pericardiocentesis evacuated 25 cc of hemorrhagic fluid, stabilizing her. Rewiring was successful. After predilation and stenting with 3.5/15 Orsiro (Biotronik, Germany), dissection persisted with contrast extravasation. Graftmaster 2.8/15 (Abbott Laboratories, USA) cover stent was placed and postdilated with NC Sapphire 3.5/10 (OrbusNeich, Hong Kong). IVUS showed MSA 7.4 mm2. In the ICU, she became dyspneic. X-ray showed pleural effusion and pleural puncture was performed. She stayed dyspneic, non-contrast chest CT showed hemopneumothorax. WSD drained hemorrhagic fluid. She stabilized and was discharged with DAPT Aspirin 80 mg OD and Ticagrelor 90 mg BD. 3 days later, she suffered GI bleeding, Haemoglobin 9.7 g/dl, BARC 3A likely due to potent antiplatelet. Ticagrelor was switched to Clopidogrel 75 mg OD and her condition improved.
Case Summary
We have presented a patient with a series of orbital atherectomy related complications such as aortocoronary dissection, cardiac tamponade, hemopneumothorax and GI bleeding. These complications are mitigated by adequate anticipation and a systematic approach of management.


