Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-091
Unexpected Coronary Involvement After Emergent Ascending Aortic Replacement
By Tzu-Yang Chen, Ying-Hsien Chen
Presenter
Tzu-Yang Chen
Authors
Tzu-Yang Chen1, Ying-Hsien Chen1
Affiliation
National Taiwan University Hospital, Taiwan1,
View Study Report
TCTAP C-091
CORONARY - Complex and Higher Risk Procedures for Indicated Patients (CHIP)
Unexpected Coronary Involvement After Emergent Ascending Aortic Replacement
Tzu-Yang Chen1, Ying-Hsien Chen1
National Taiwan University Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
6373888
Relevant Clinical History and Physical Exam
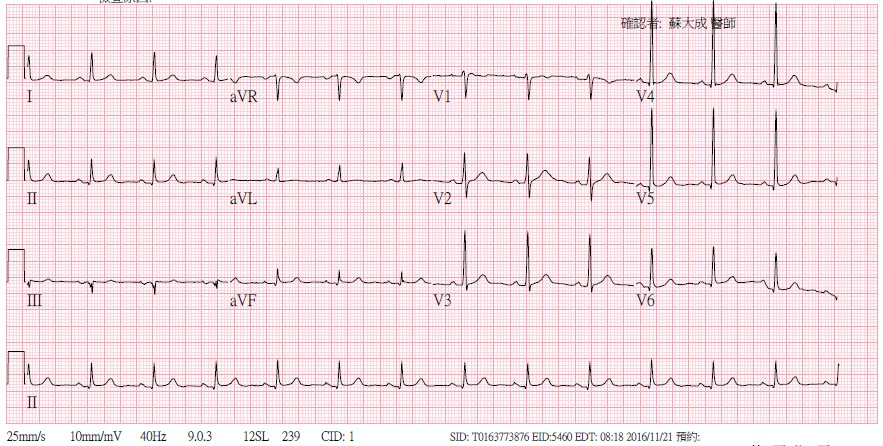
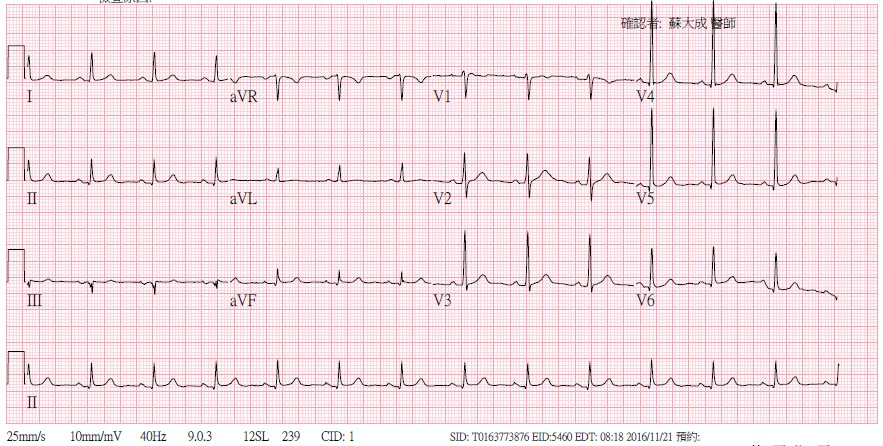
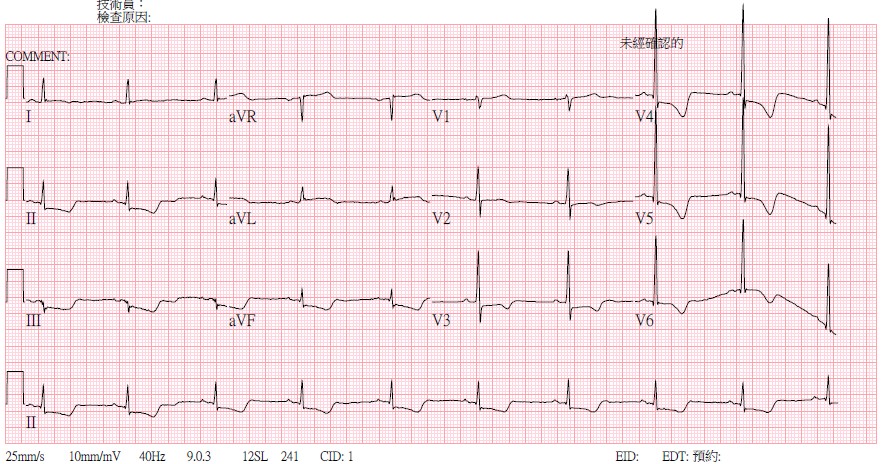
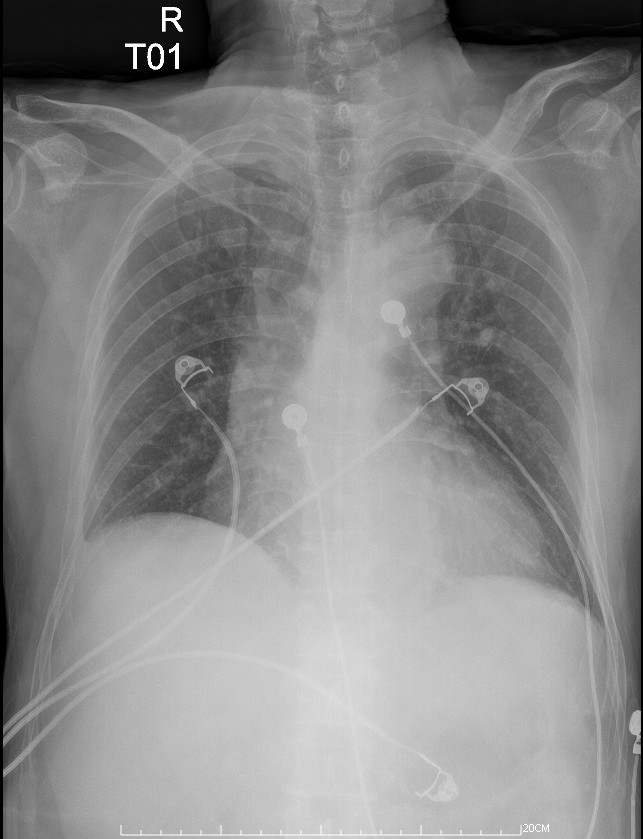
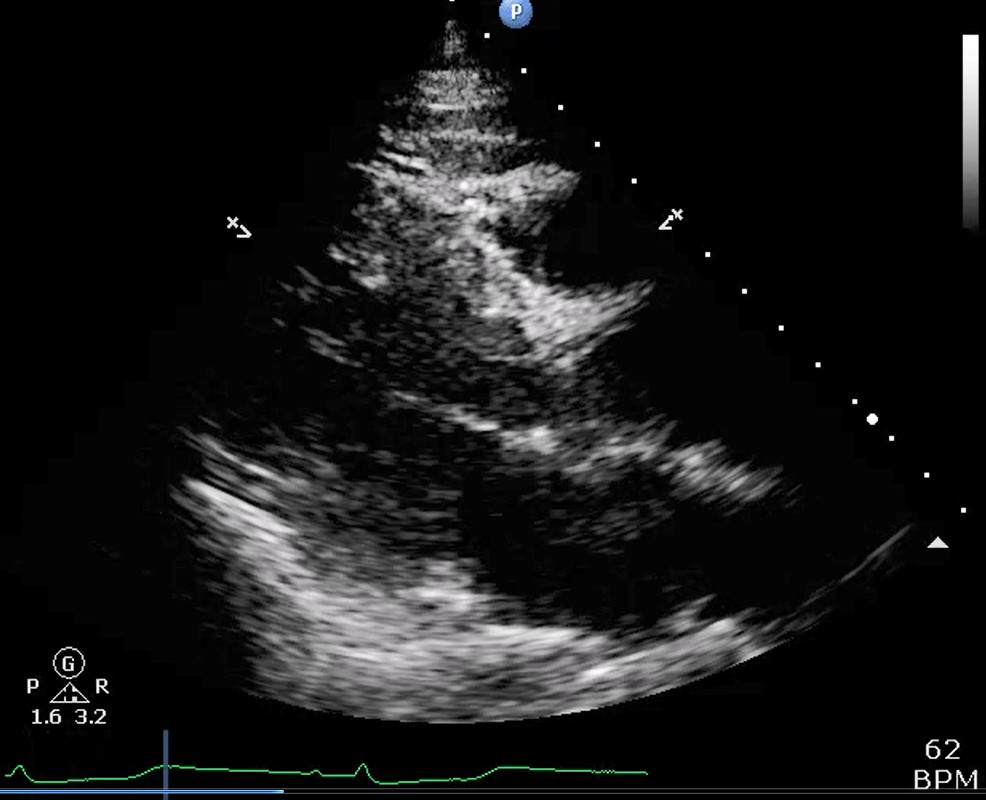
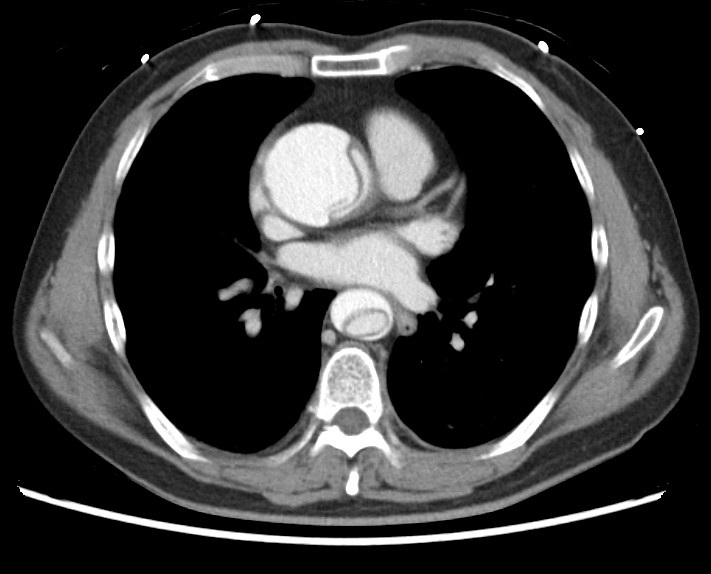
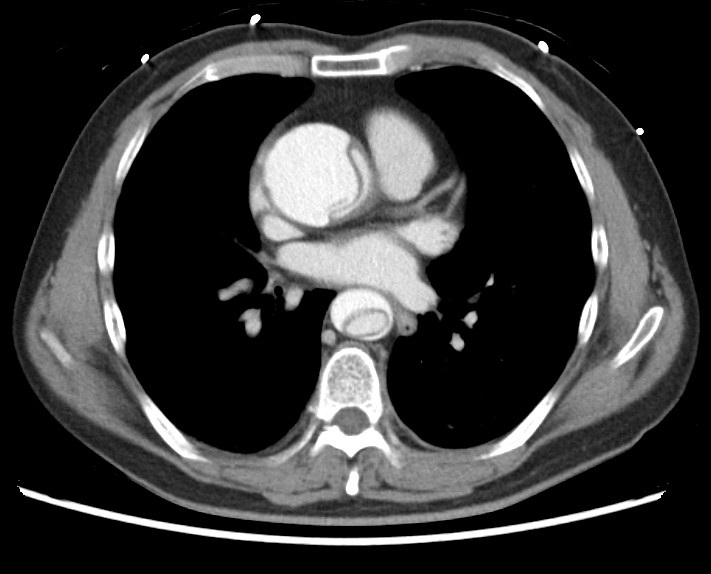
This 62-year-old male complained of sudden onset of chest pain, with radiation to back, in the early morning while sleeping. Accompanied with hands and legs numbness. Initial EKG in our emergent department showed ST elevation at aVL and ST depression at inferior and lateral leads. Cardiac echo showed dilated aortic root with moderate aortic regurgitation and akinesia of LV lateral wall. CT revealed type A aortic dissection. CV specialist and surgeon were consulted. Emergent surgery was arranged.
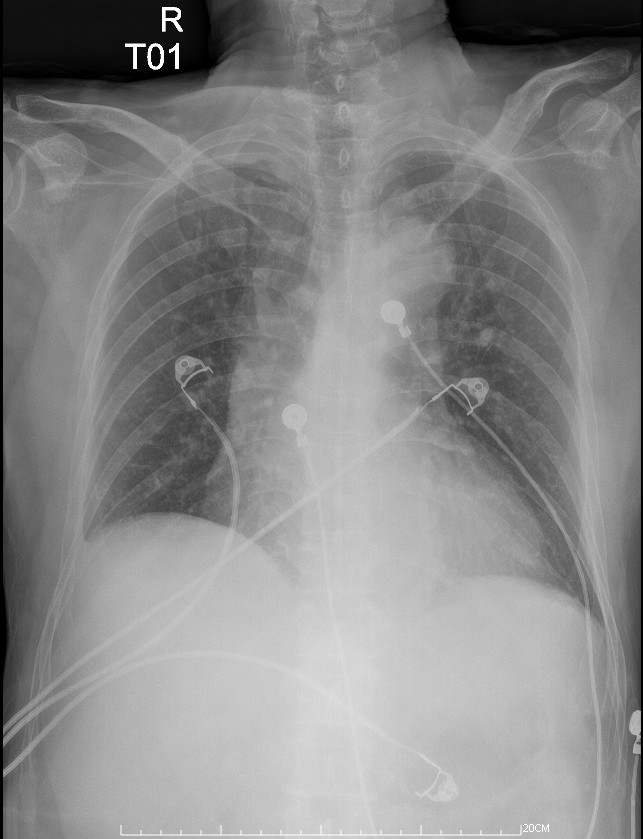
Relevant Test Results Prior to Catheterization
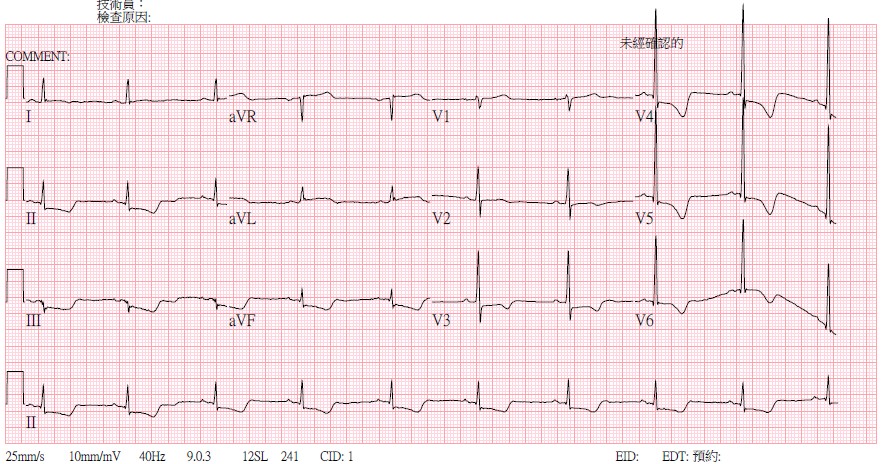
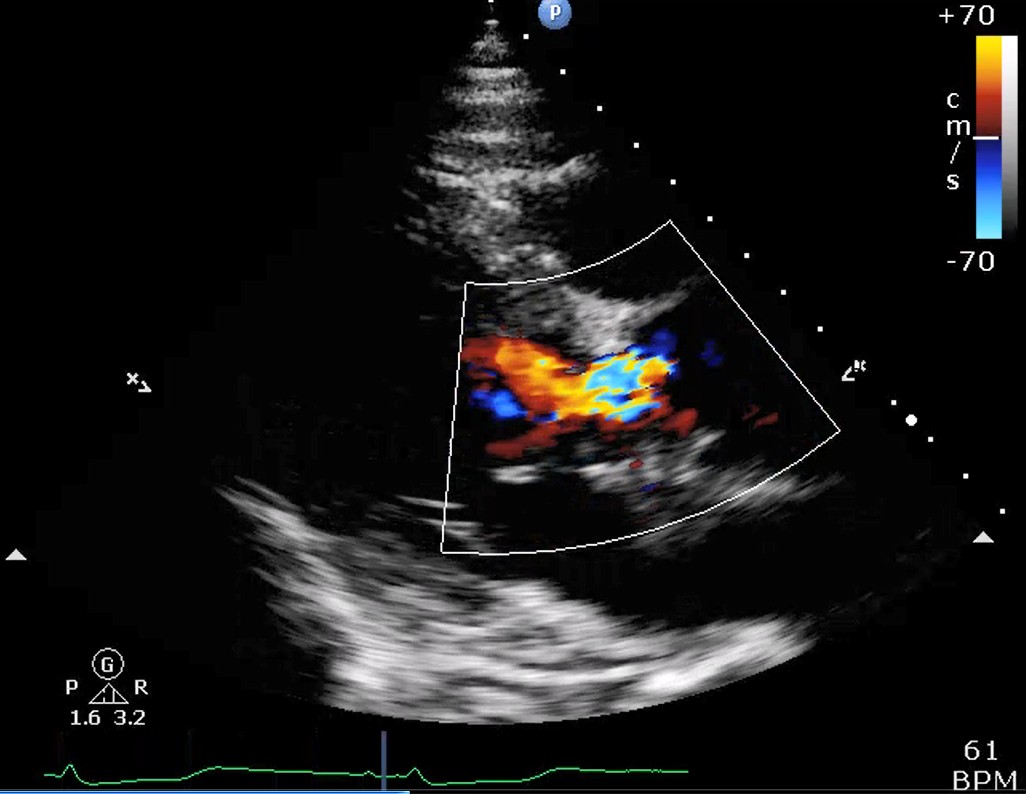
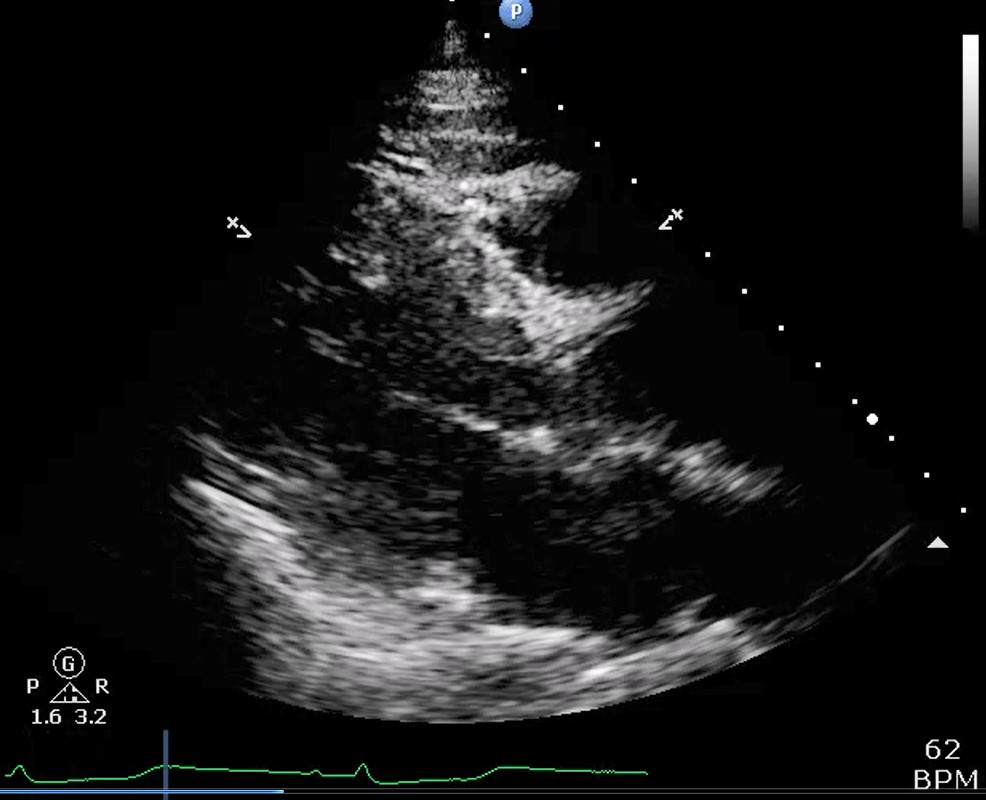
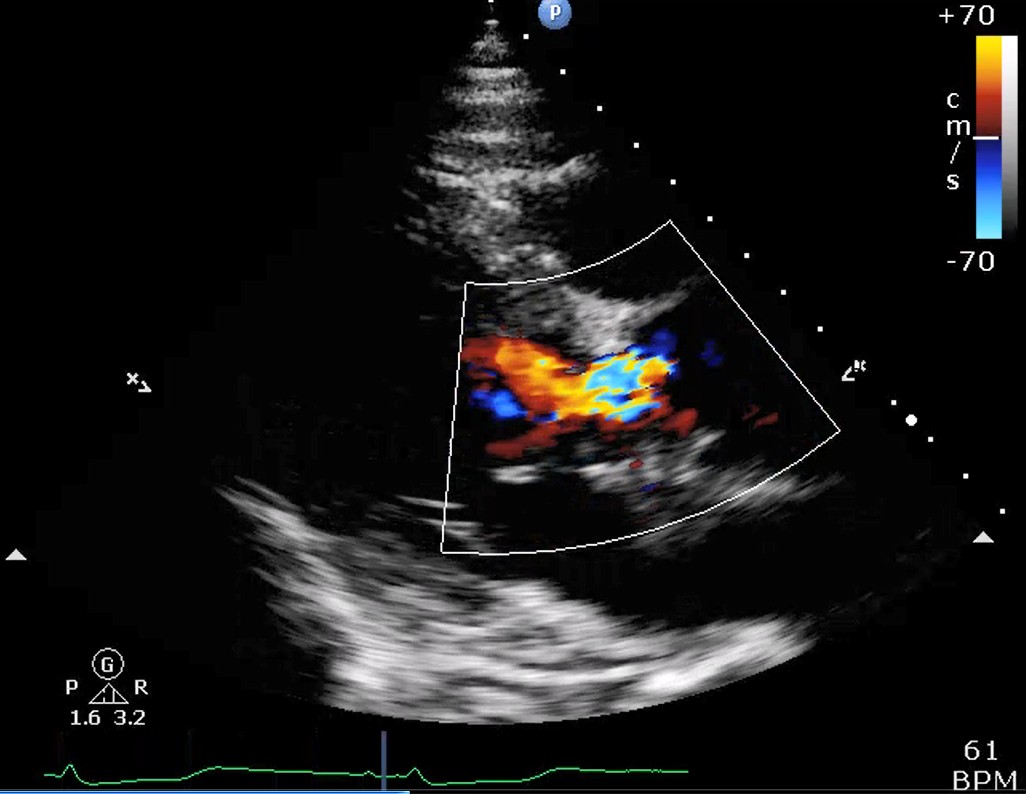
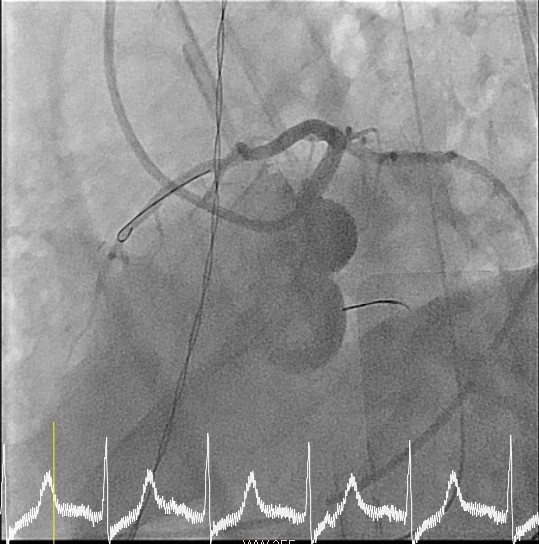
Patient was intubated under anesthesia. Intra-operative TEE showed intact RCA and LCA ostia. After set up of cardiopulmonary bypass (CPB), mid diseased ascending aorta was replaced with graft. Entry site of intimal tear was found to be located at proximal and lesser curvature of aortic arch. LV hypokinesia with cardiogenic shock was found during weaning from CPB. Follow up TEE revealed poor LCA ostium flow. CPB thus switched to VA ECMO, and interventional cardiologist was consulted for ACS.
Relevant Catheterization Findings
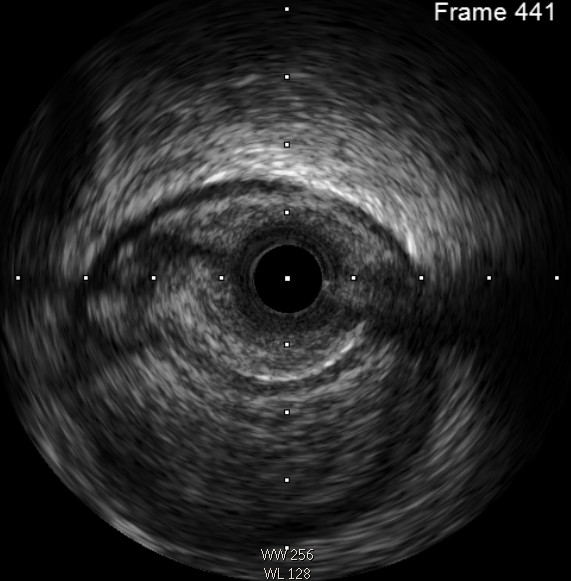
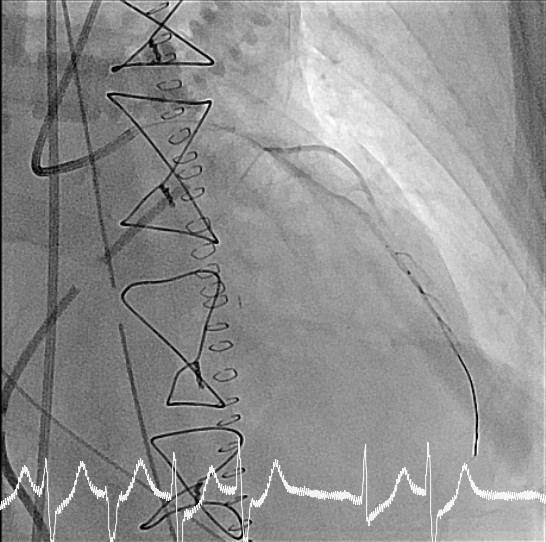
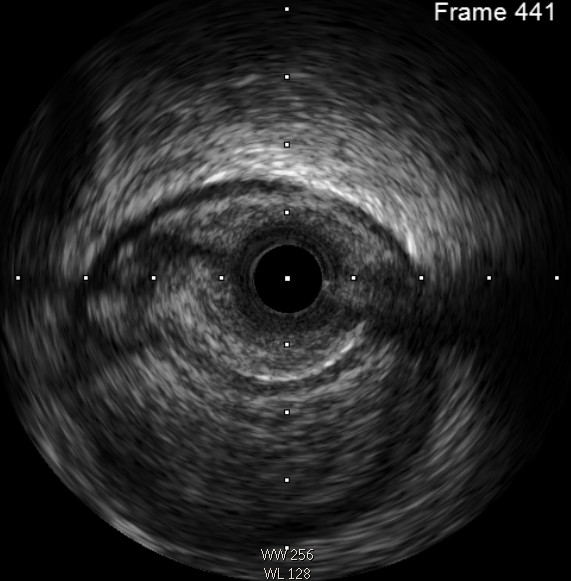
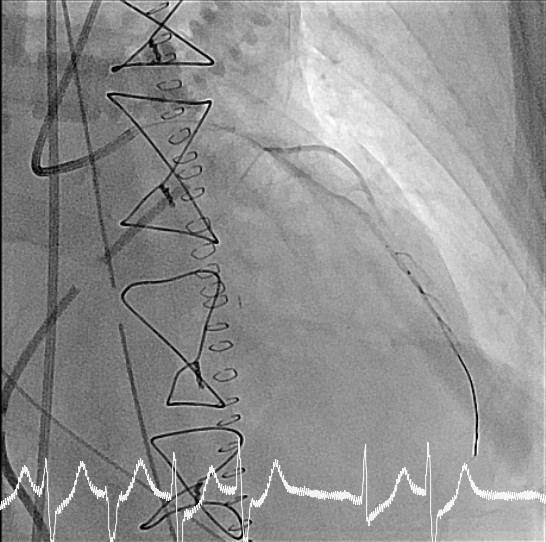
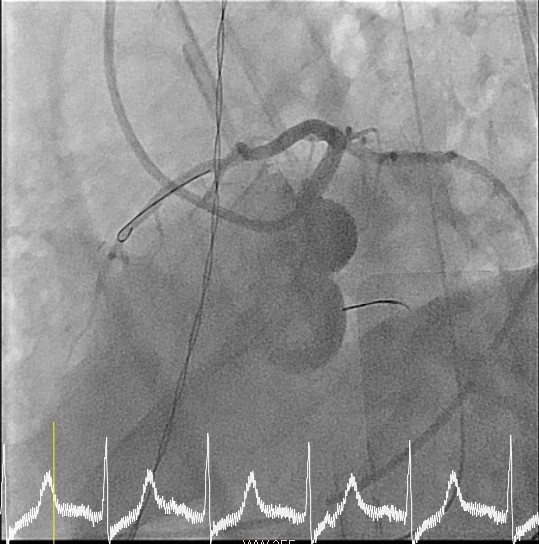
Diagnostic coronary angiography showed 80% stenosis of left main artery shaft, total occlusion of proximal LAD, total occlusion of proximal left circumflex artery, and patent right coronary artery. Intravascular ultrasound revealed coronary artery stenosis due to intramural hematoma compression, which was compatible with the mechanism of aortic dissection with coronary involvement.






Interventional Management
Procedural Step
1. Right femoral artery was punctured with 6F sheath. Performed diagnostic coronary angiography first. Engaged 6F guiding catheter Medtronic JL3.5 to left coronary, and carefully wired ASAHI Sion wire (GW1) to distal LAD.2. Performed thrombosuction with Medtronic Export aspiration catheter to LM-LAD, while no thrombus was aspirated.3. Pre-dilated stenotic site with balloon (Terumo Ryurei 2.0 x 15 mm) to proximal LAD.4. Evaluated lesion with IVUS from distal LAD to LM, which showed LAD diffuse stenosis due to external intramural hematoma compression and loss of intima continuity. Coronary dissection was favored.5. Advanced Crusade catheter to distal LAD for contrast tip injection, which showed patent distal vessel with TIMI2 flow.6. Wired Terumo Runthrough floppy wire (GW2) to distal LCx, and deployed stent (BOSTON REBEL 3.0 x 28 mm) to proximal LAD.7. Evaluated lesion with IVUS from distal LCx to proximal LCx, which showed diffuse stenosis due to external intramural hematoma compression, and we suspected that partial wire segment was in false lumen (true-false-true).8. Re-wired GW2 to distal LCx, and pre-dilated with balloon (Medtronic Euphora 2.0 x 15 mm) to dLCx.9. Rechecked IVUS showed true lumen wiring.10. Deployed 2 identical stents (Abbott MULTI-LINK8 2.5 x 38 mm) from distal LCx to proximal LCx. LCx flow was noted after stenting.11. Deployed stent (Medtronic INTEGRITY 3.5 x 30 mm) from proximal LAD to LM.12. The final flow improved so we closed the procedure.
Case Summary
We presented with a case of type A aortic dissection while acute coronary syndrome was not suspected initially. Coronary involvement was not documented in intra-operative TEE either. However, acute coronary syndrome developed in the end of ascending aortic replacement surgery. Cardiac cath was performed under VA ECMO support, which revealed coronary stenosis due to intramural hematoma compression. Fortunately, successful wiring and stenting were provided. Delicate coronary evaluation should be performed initially in every patient with type A aortic dissection and also in patients who received ascending aortic surgery.


