Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-134
Leave Nothing Behind (Drug-Coated Balloon Angioplasty for Side Branch Treatment)
By Bon-Kwon Koo, Kyu-Sun Lee
Presenter
Kyu-Sun Lee
Authors
Bon-Kwon Koo1, Kyu-Sun Lee2
Affiliation
Seoul National University Hospital, Korea (Republic of)1, Eulji medical center, Korea (Republic of)2,
View Study Report
TCTAP C-134
CORONARY - Drug-Eluting Balloons
Leave Nothing Behind (Drug-Coated Balloon Angioplasty for Side Branch Treatment)
Bon-Kwon Koo1, Kyu-Sun Lee2
Seoul National University Hospital, Korea (Republic of)1, Eulji medical center, Korea (Republic of)2,
Clinical Information
Patient initials or Identifier Number
48701451
48701451
48701451
48701451
48701451
Relevant Clinical History and Physical Exam
The patient was a 56-year-old man with several past medical histories of hypertension, dyslipidemia, and a family history of CVD. At the time of 2017, the patient’s estimated 10-year atherosclerotic CVD risk was 15.9%. In December 2017, at the time of the outpatient visit, he complained of typical chest pain. Chest pain gets worse and occurs even at rest and chest pain is only relieved by multiple doses of nitroglycerin. UA was suspected and he was admitted to our hospital.
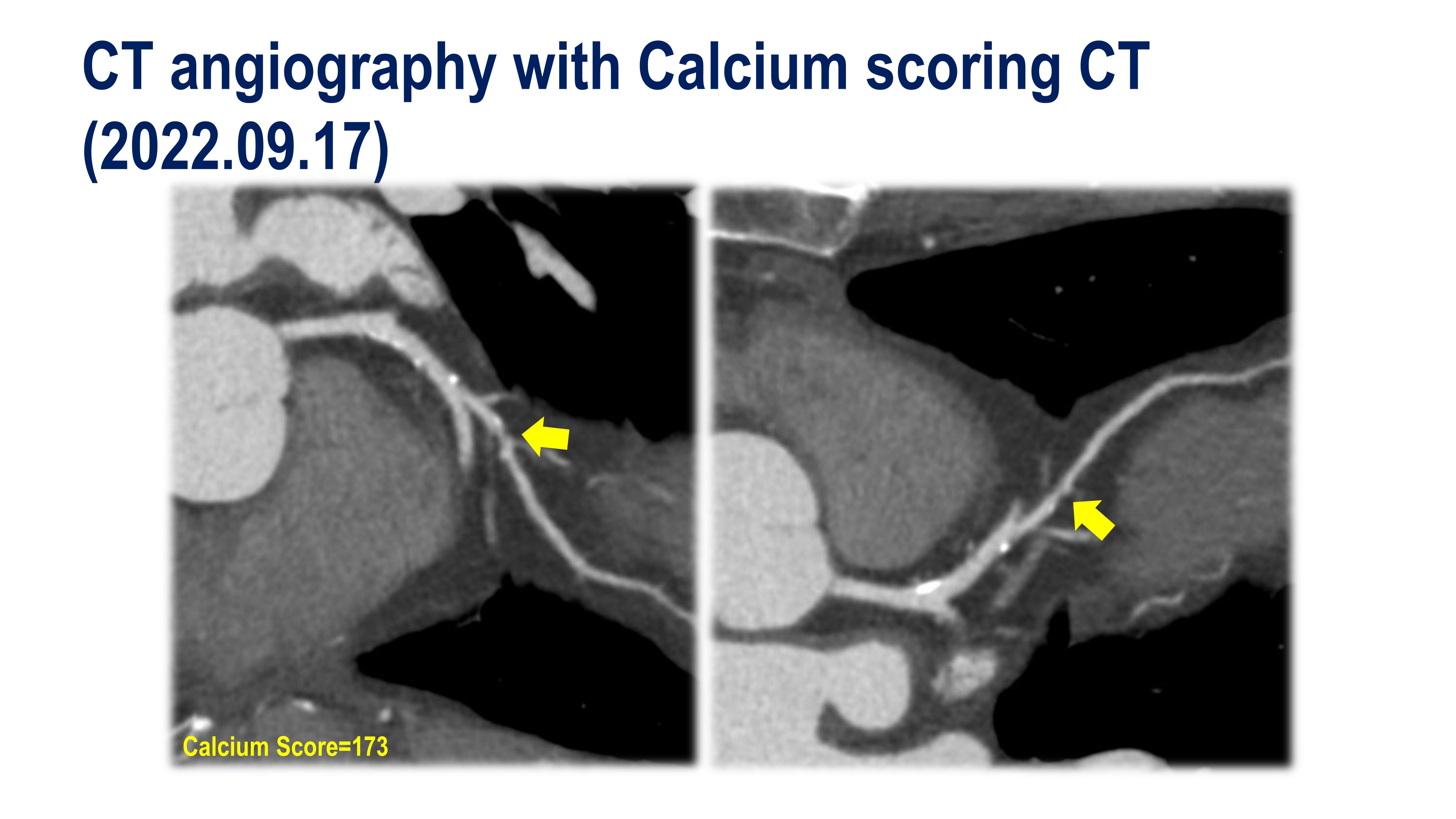
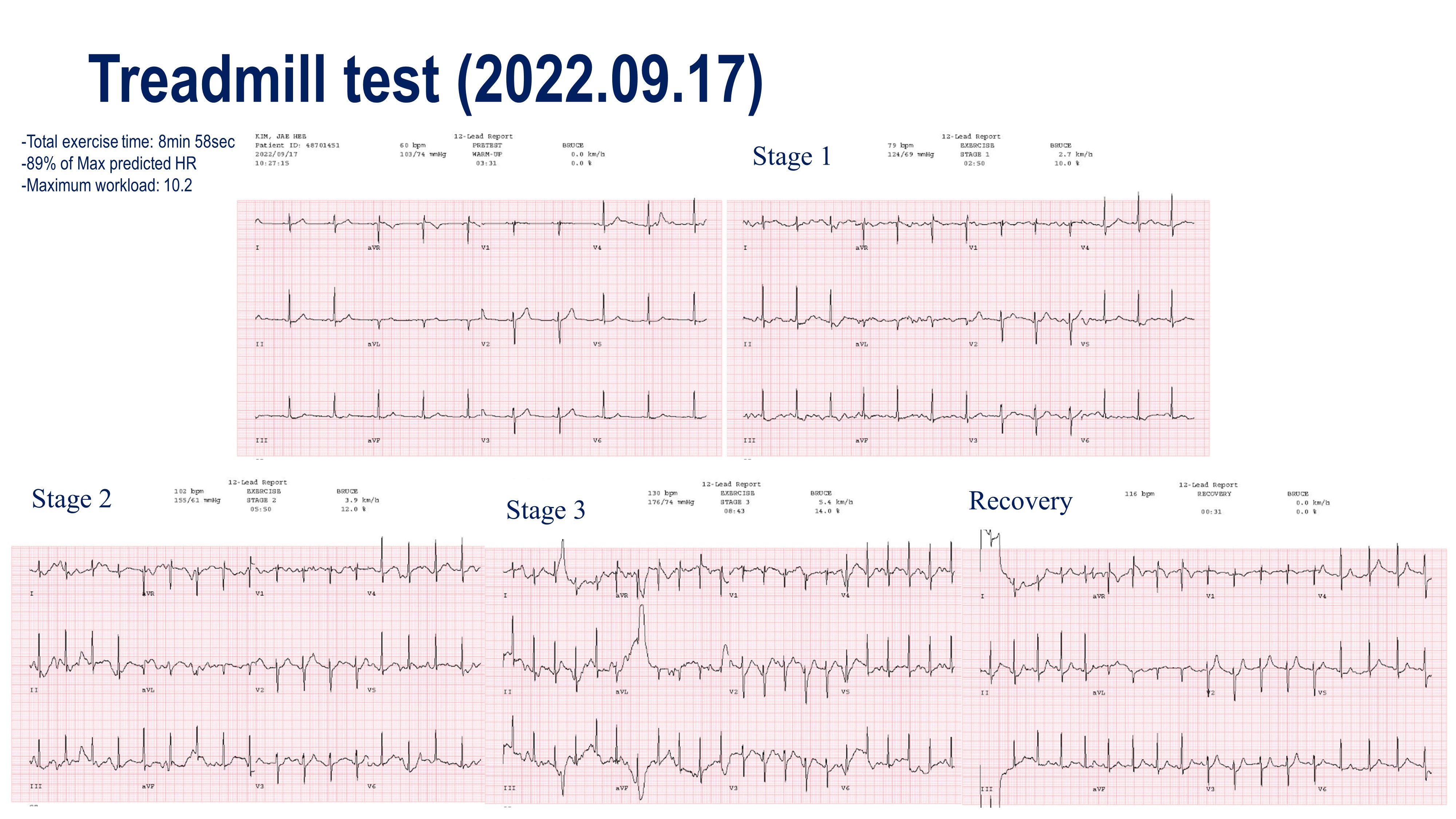
Relevant Test Results Prior to Catheterization
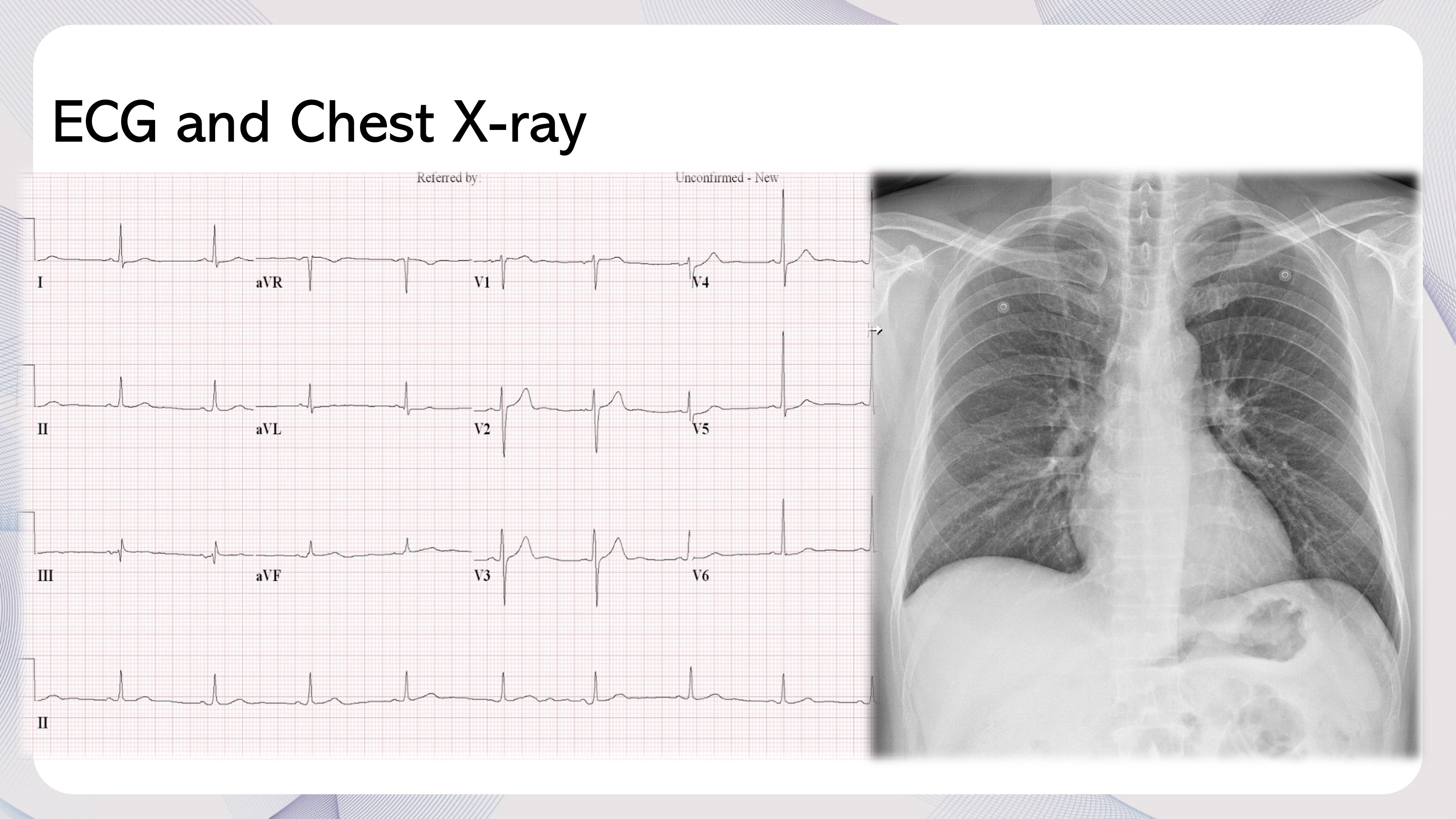
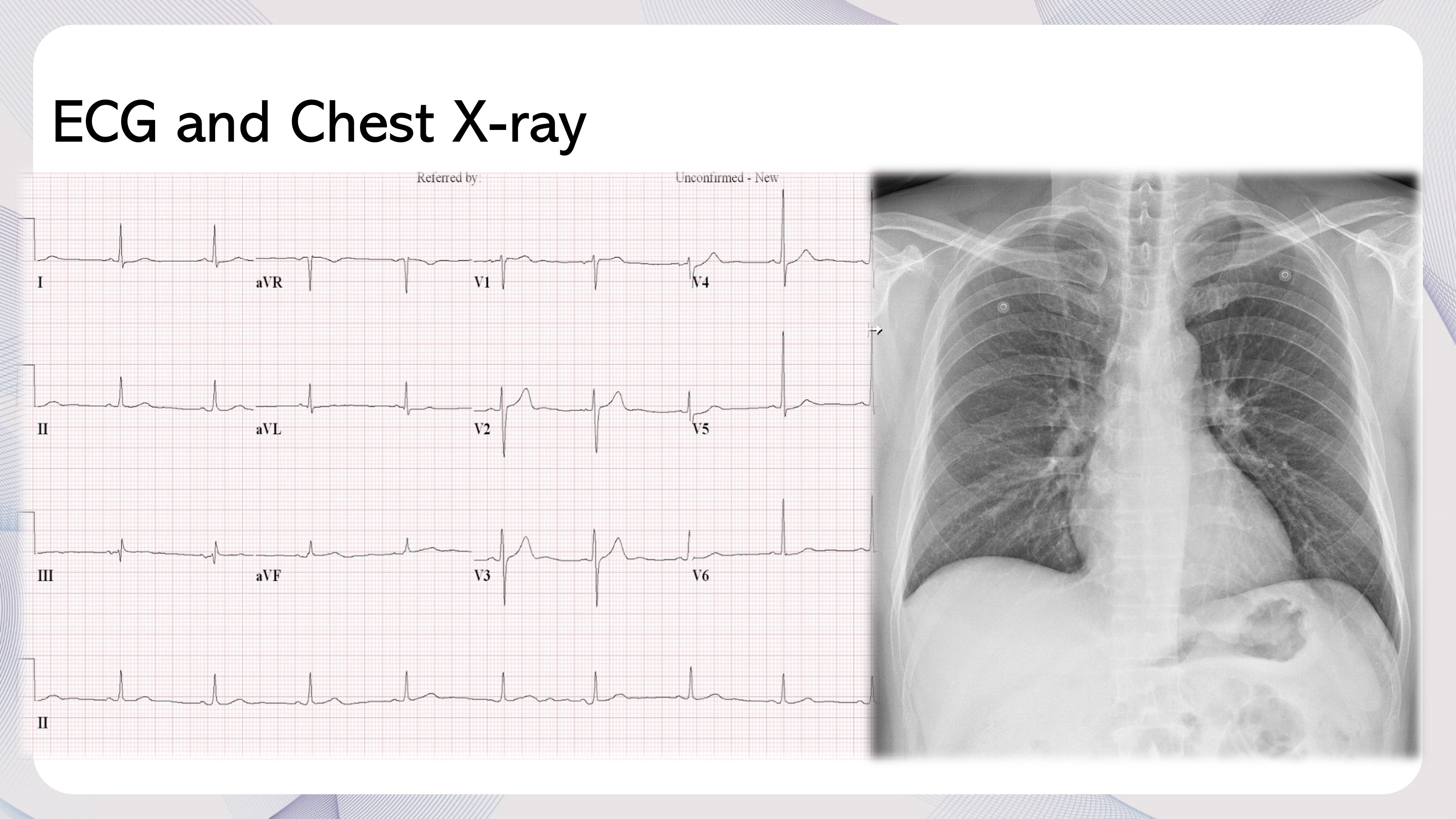
On admission, his vital sign was stable and ECG showed normal sinus rhythm without an ischemic sign. On the Chest x-ray, There was no abnormal finding in the lung parenchyma, and bony thorax. Also, cardiomegaly was not observed. Furthermore, overall the results of laboratory tests including were normal range. Echocardiography showed a normal LV function and there was no regional wall motion abnormality.
Relevant Catheterization Findings
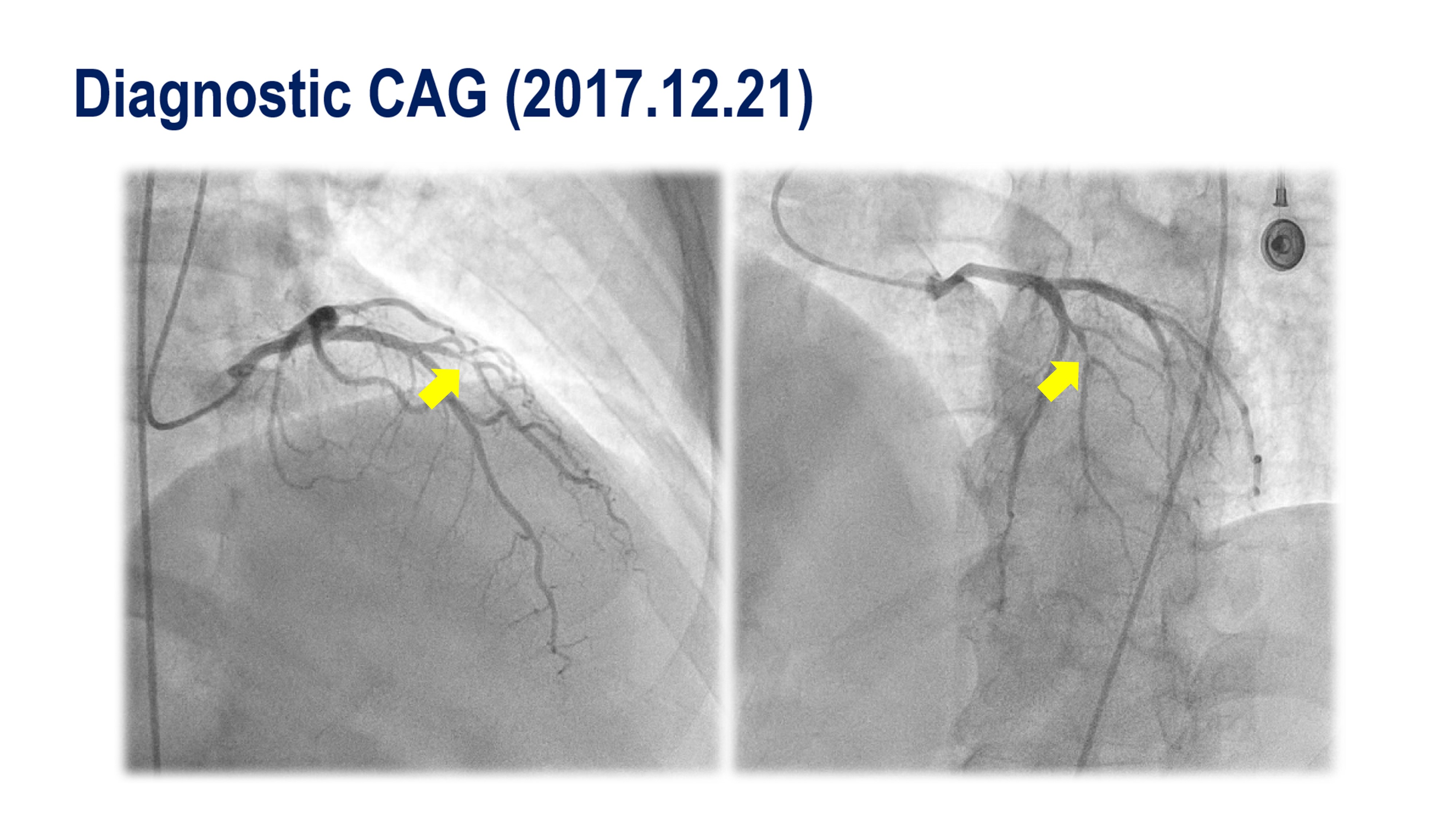
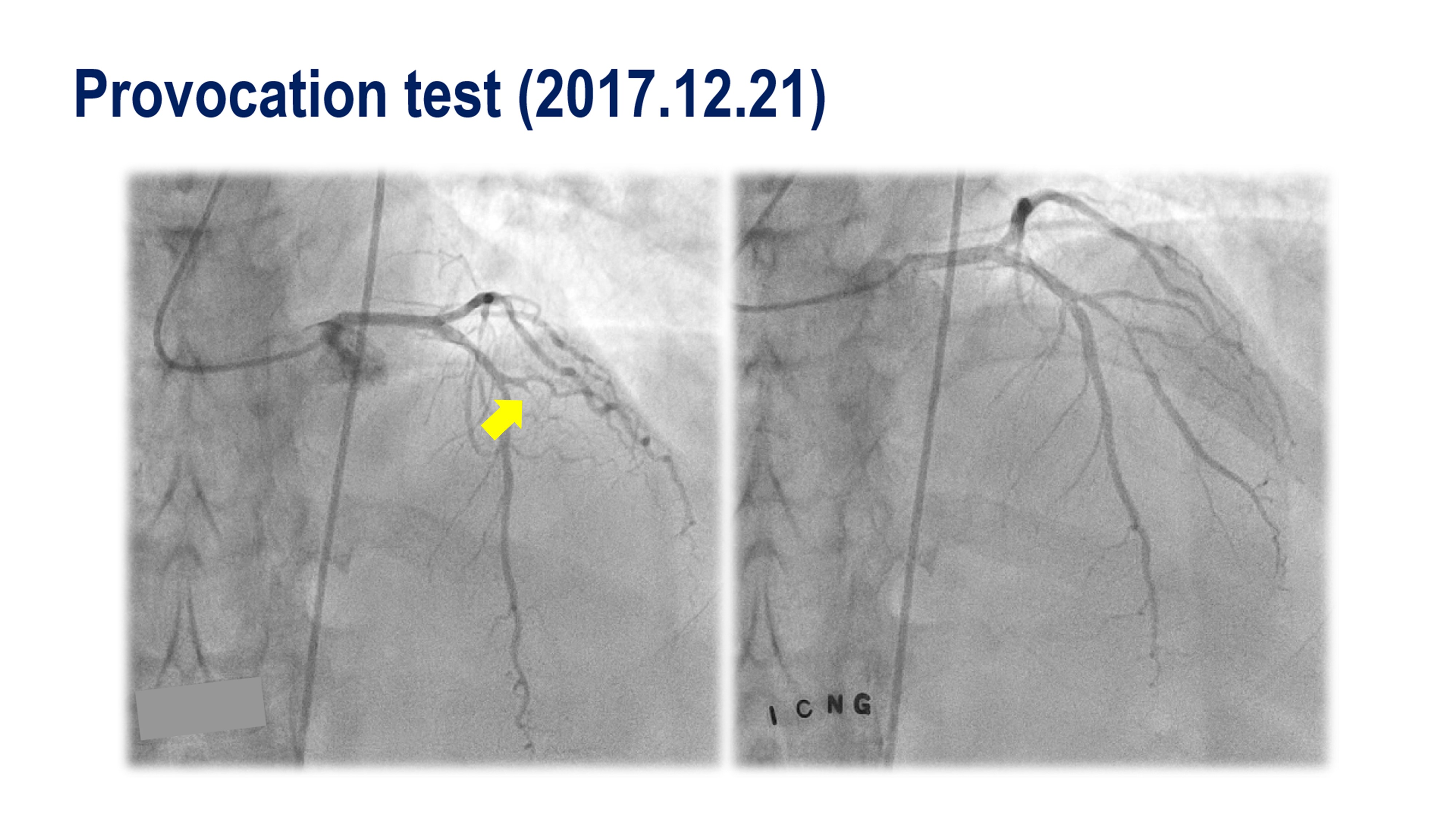
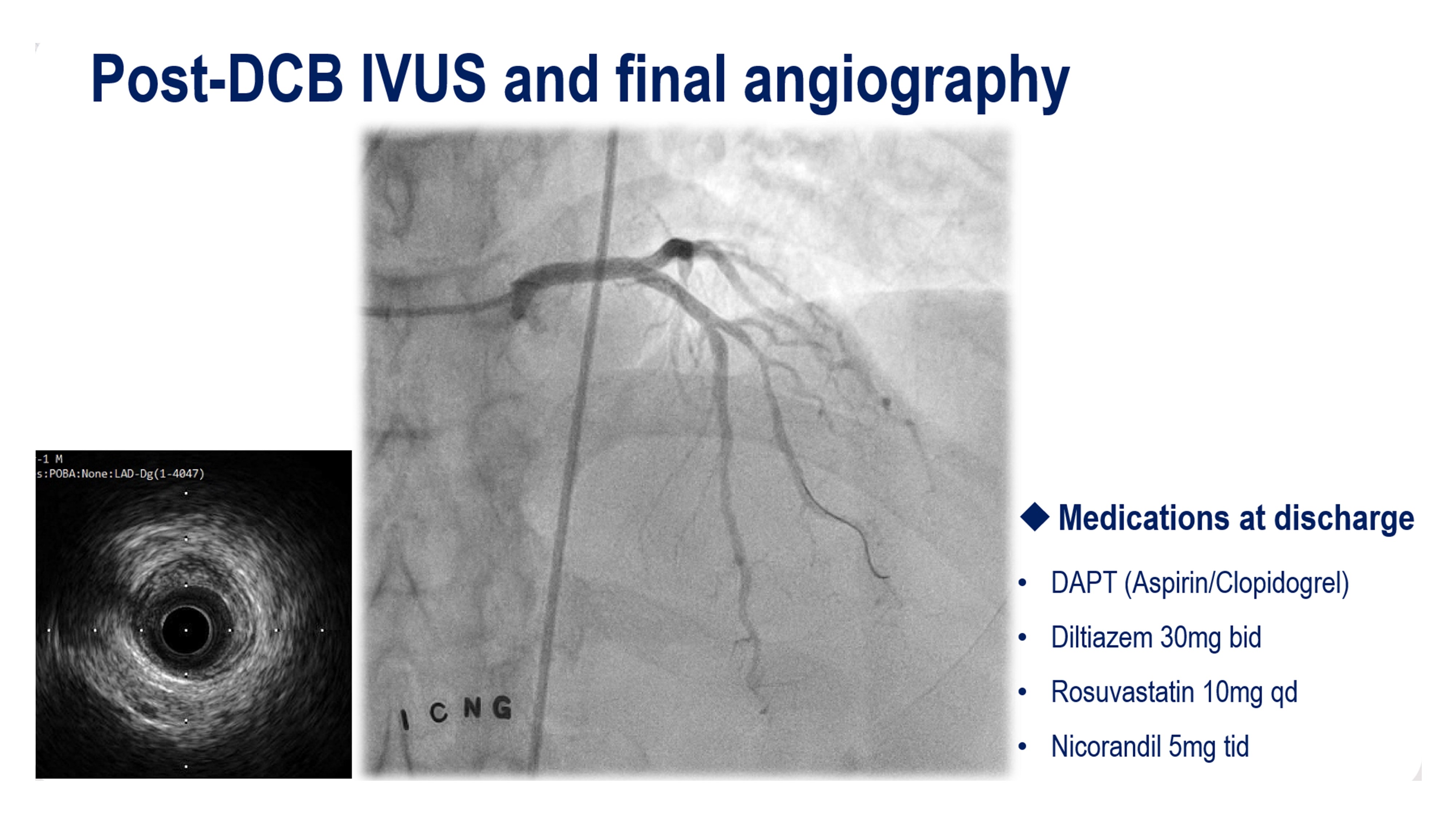
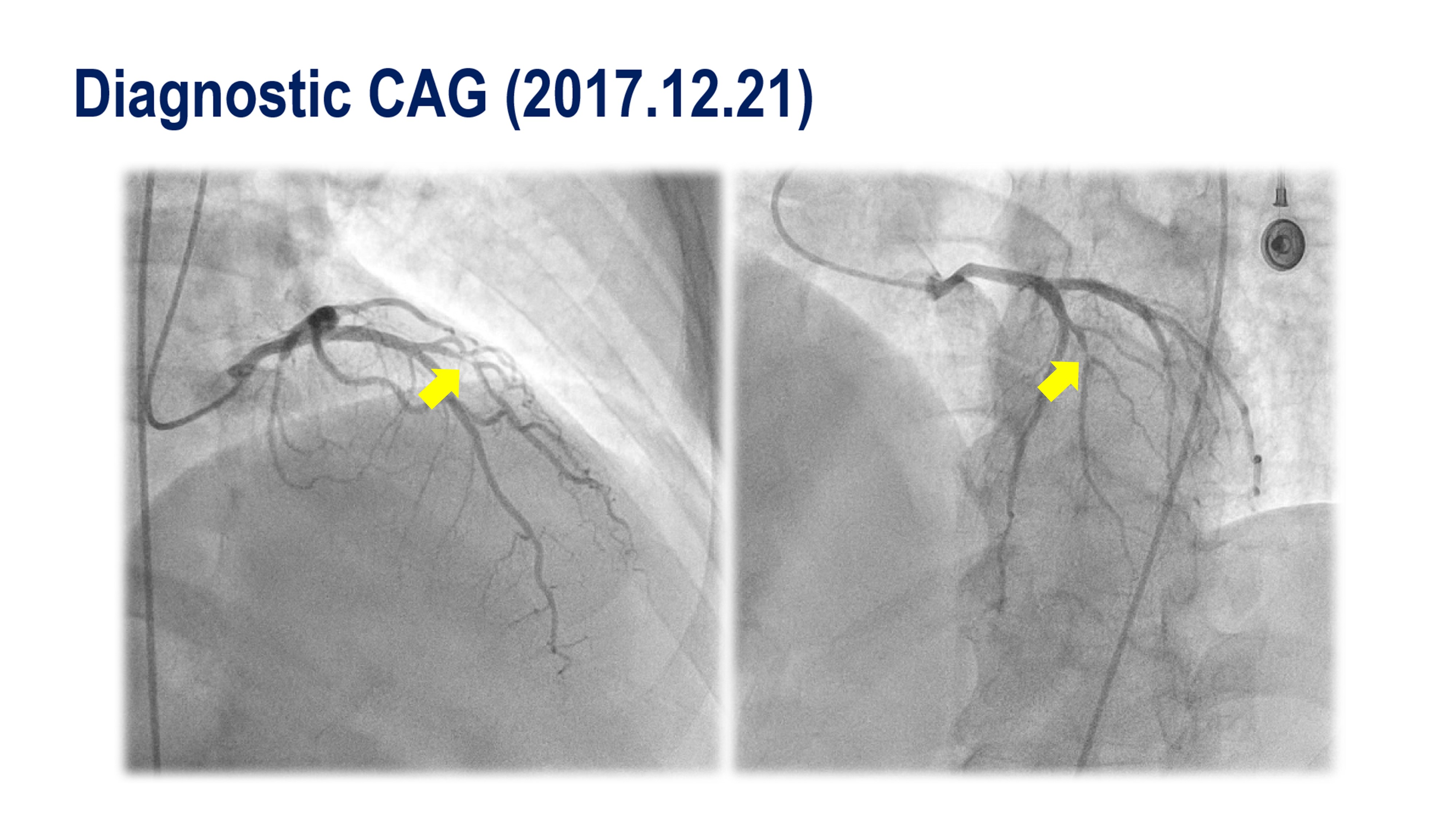
The diagnostic coronary angiography revealed a focal 90% stenosis of a 1st Dg branch and a diffuse 60% stenosis of the distal circumflex artery. Next, we performed an ergonovine provocation test to rule out the possibility of variant angina because he complained of chest pain at midnight and the pain was well relieved by NG. After IV administration of ergonovine 200mg 2 times at intervals of 2mins, total occlusion was observed at 1st Dg and he complained of chest pain.
Interventional Management
Procedural Step
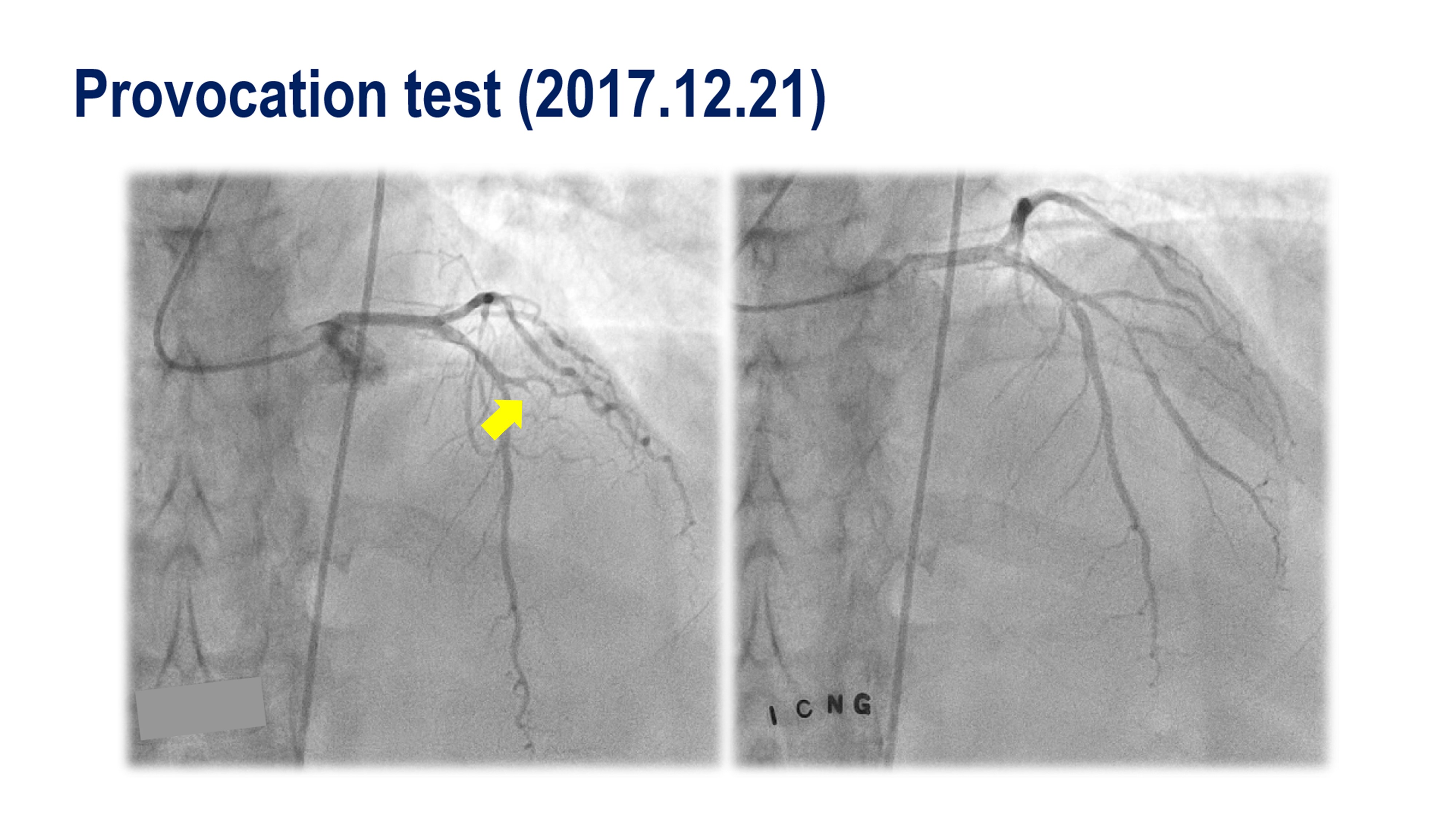
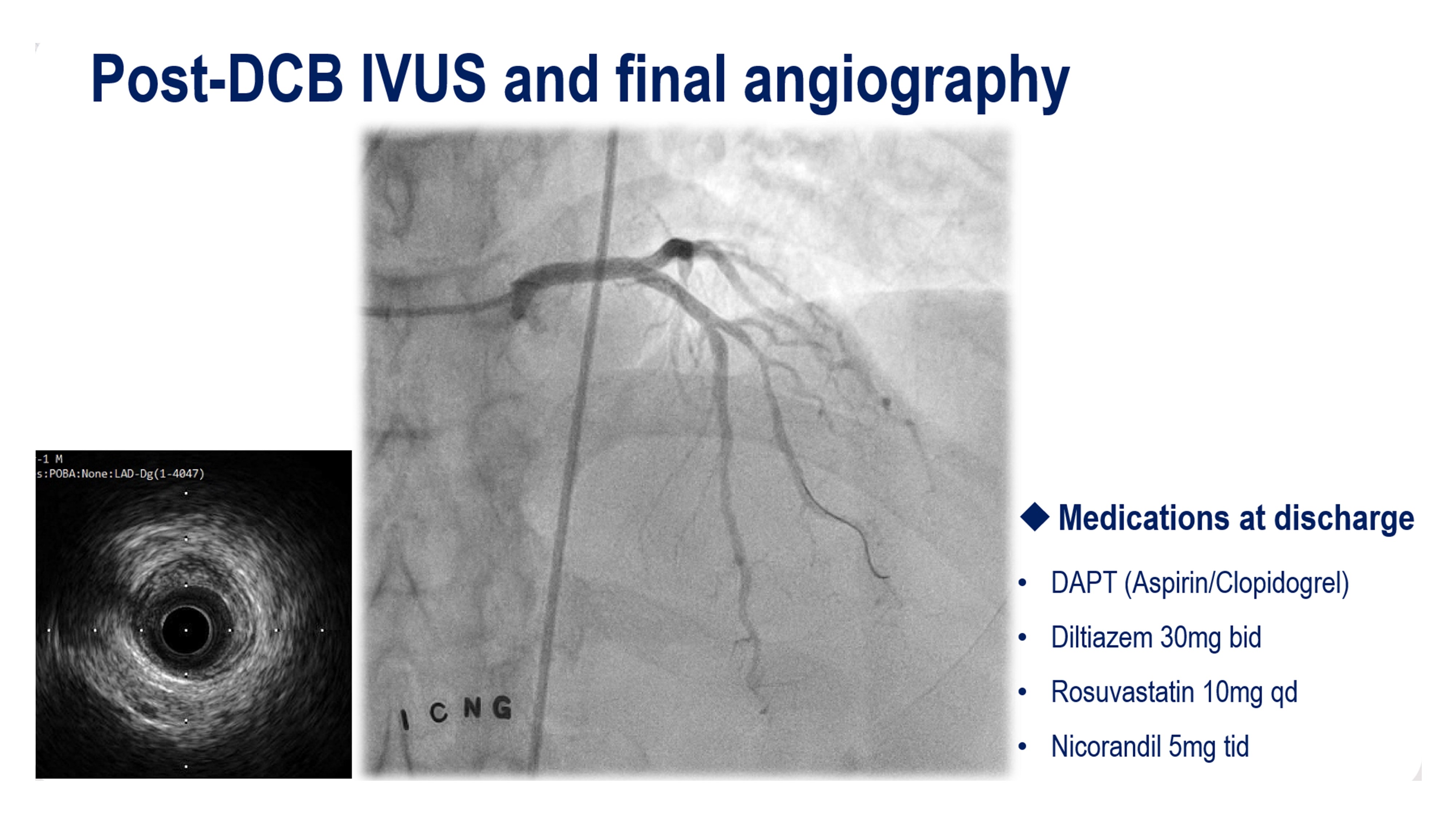
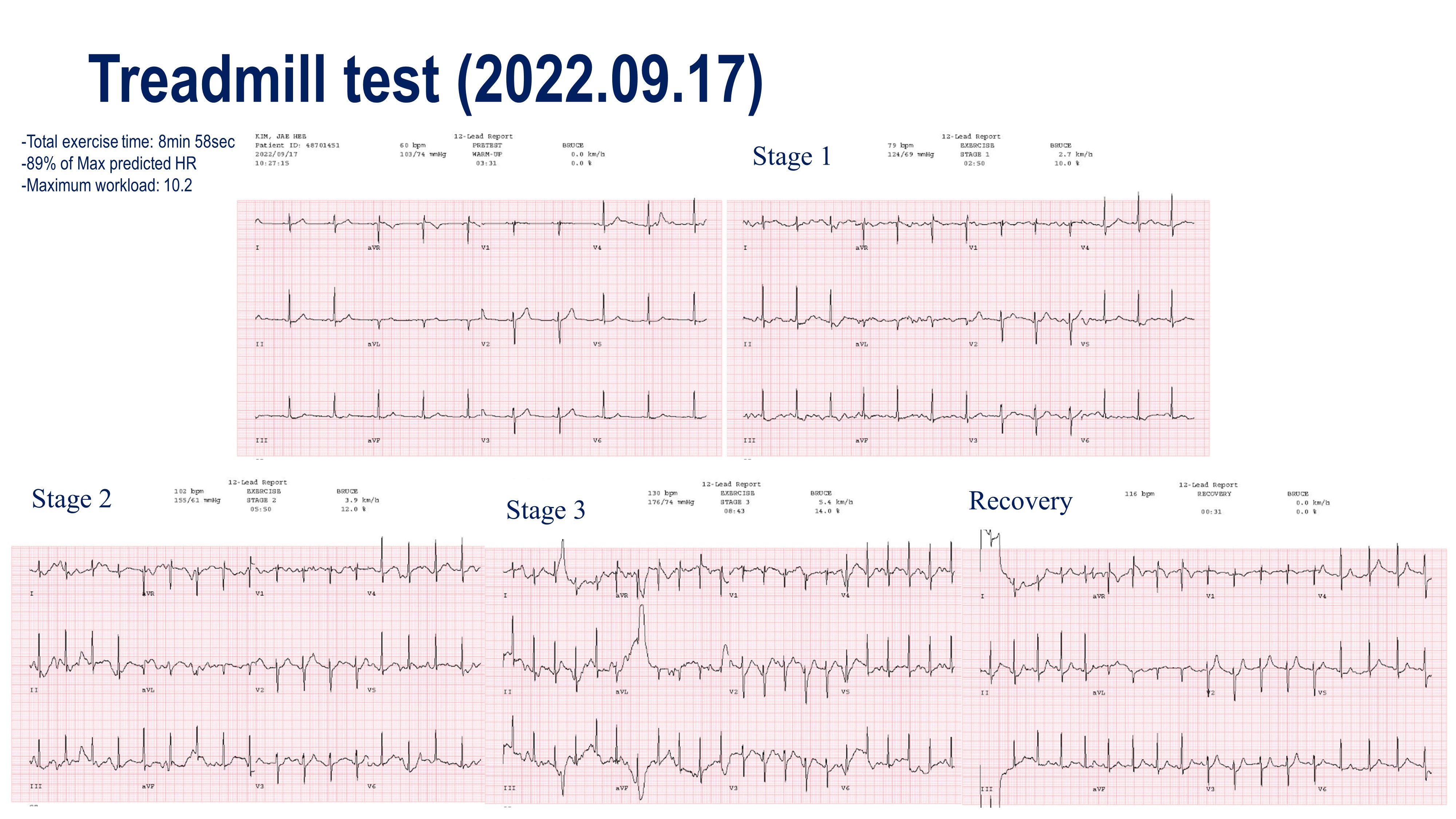
During hospital admission, 1. Diagnostic coronary angiography and ergonovine provocation test was performed because he suspected unstable angina or variant angina.we confirmed the severe stenotic lesion in 1st diagonal branch, and have seen a vasospastic change from the provocation test. 2. FFR was performed and the FFR was 0.73 in the diagonal branch.3. POBA to the diagonal branch was performed and confirmed that the distal reference diameter was 3.0mm, more than 60% calcified plaque, and negative remodeling in the diagonal lesion. The minimal lesion diameter was 2.4x2.6mm4. Post-POBA FFR and IVUS5. DCB was performed at the diagonal branch6. Post-DCB FFR and IVUS were performed. the FFR was o.96After successful DCB angioplasty, symptoms disappeared and there was no significant stenosis or myocardial ischemia evidence in follow-up N-13 Ammonia PET/CT and coronary CT angiography.
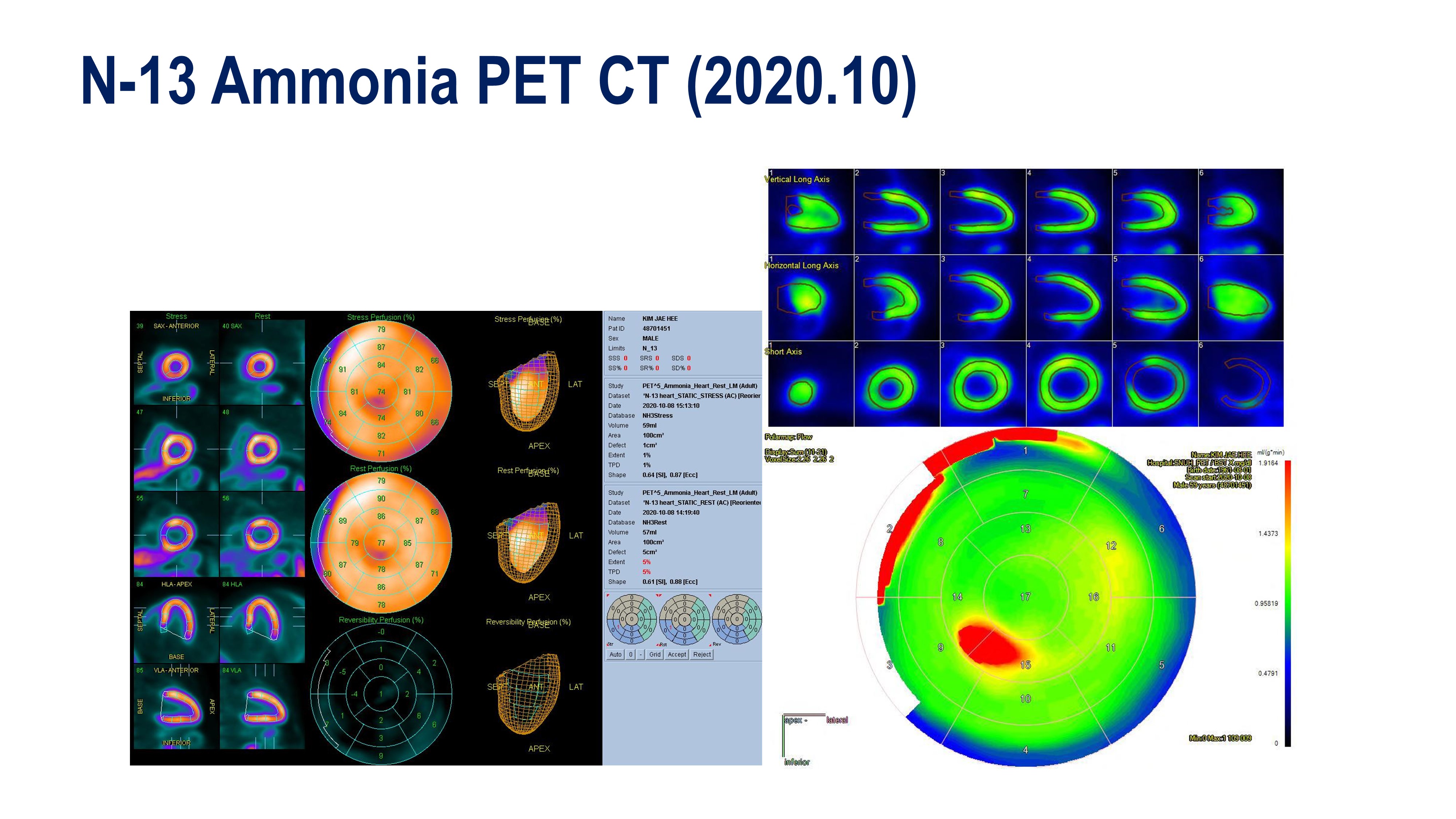
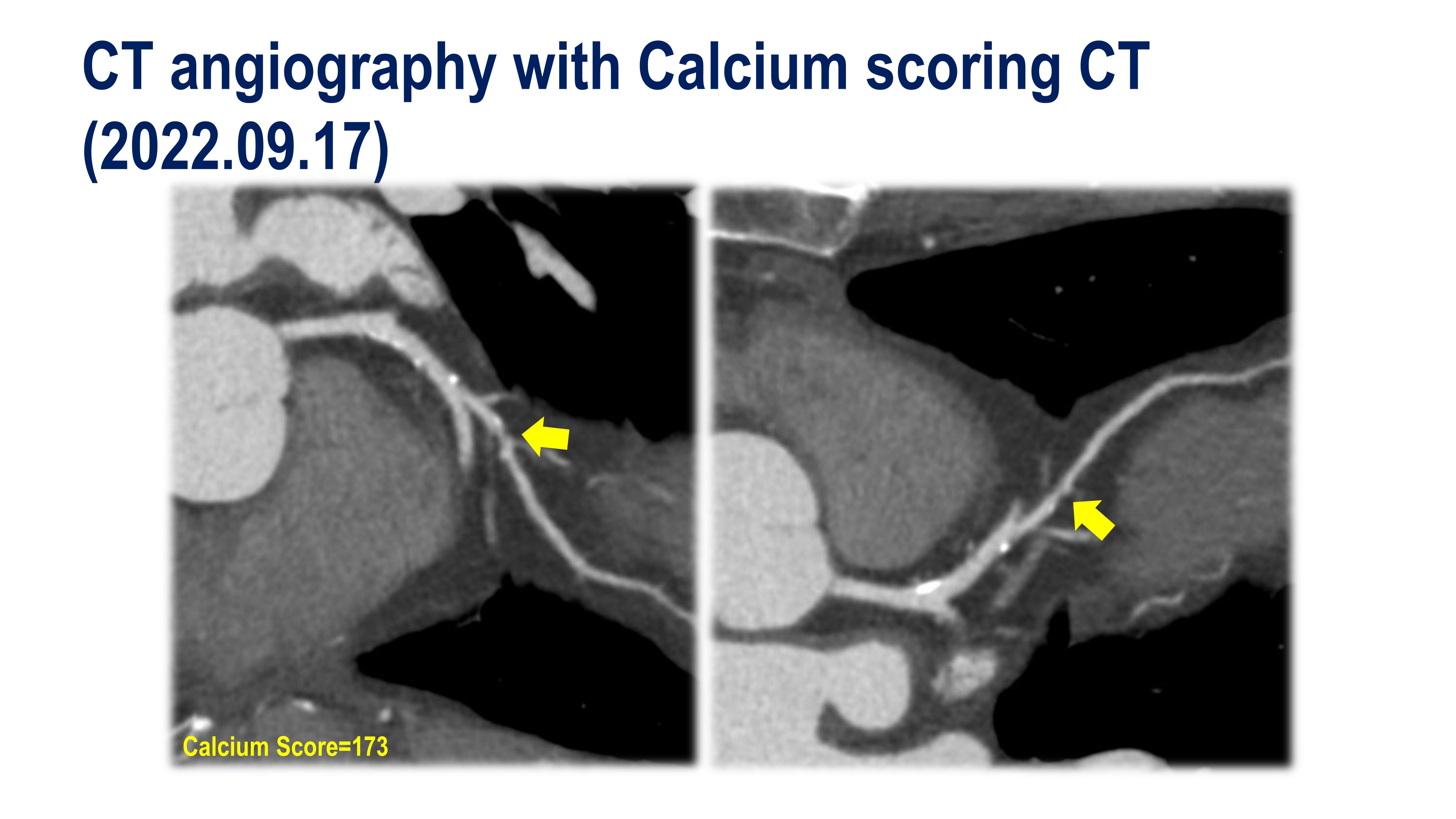
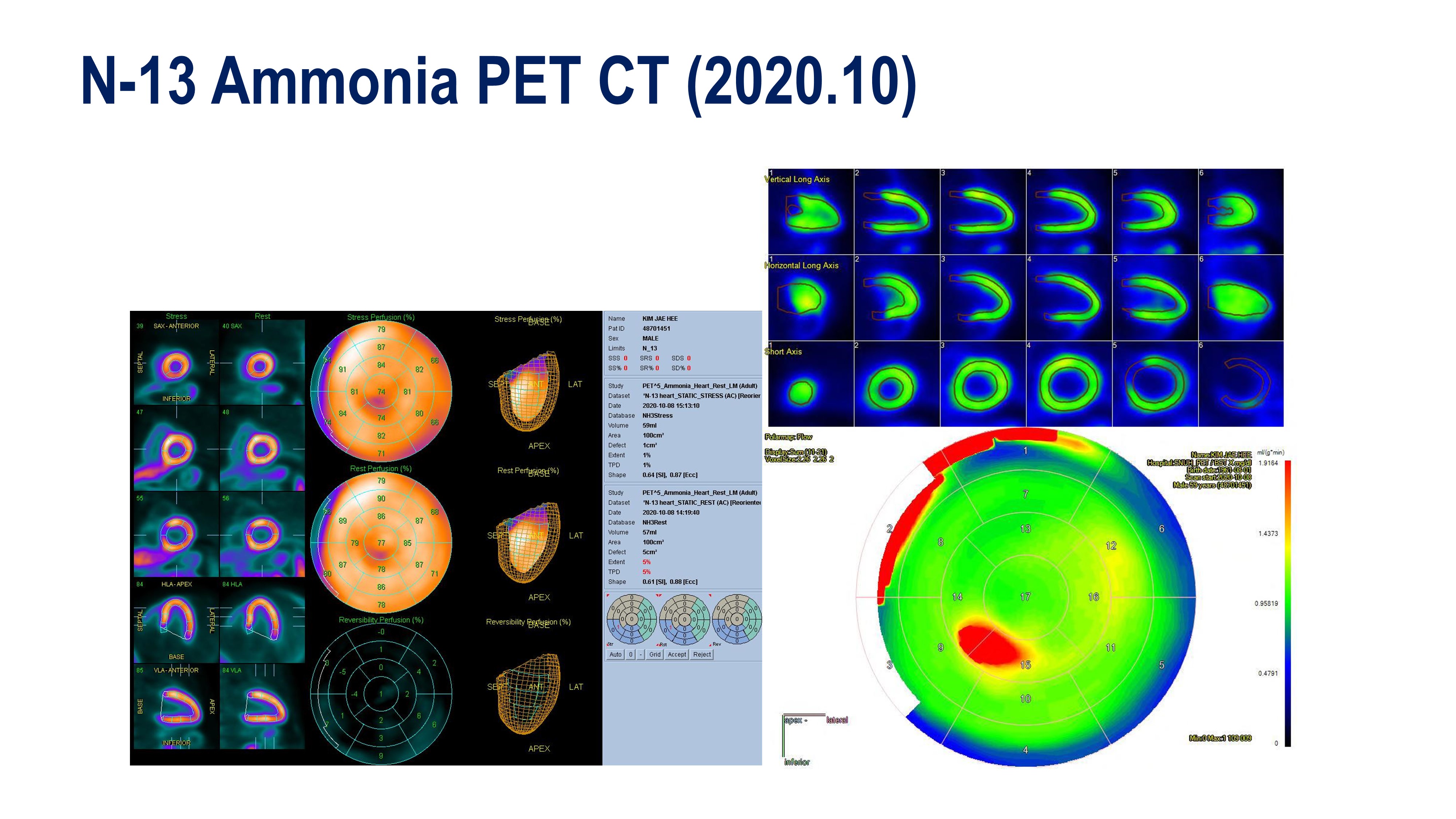
Case Summary
This case was the development of a fixed obstructive coronary lesion in a patient with variant angina. The point of this case is whether to treat this 1st Dg branch or not and if treated, how to treat this SB, de-novo lesion in the small vessel? In this case, we decided to apply the " leave nothing behind" strategy with drug-coating balloon angioplasty at the 1st Dg branch. After successful DCB angioplasty, the patient did not complain of chest pain and has been prescribed clopidogrel and statin. Currently, the patient has only been prescribed statin without an antiplatelet agent.


