Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-077
Antegrade Approach Strategy for Left Main CTO Lesion
By Susila Surya Darma, Doni Firman, Amir Aziz Alkatiri, Arwin Saleh Mangkuanom, Nanda Iryuza
Presenter
Susila Surya Darma
Authors
Susila Surya Darma1, Doni Firman2, Amir Aziz Alkatiri2, Arwin Saleh Mangkuanom2, Nanda Iryuza2
Affiliation
Prof. Dr. I.G.N.G Ngoerah Hospital, Indonesia1, National Cardiovascular Center Harapan Kita, Indonesia2,
View Study Report
TCTAP C-077
CORONARY - Chronic Total Occlusion
Antegrade Approach Strategy for Left Main CTO Lesion
Susila Surya Darma1, Doni Firman2, Amir Aziz Alkatiri2, Arwin Saleh Mangkuanom2, Nanda Iryuza2
Prof. Dr. I.G.N.G Ngoerah Hospital, Indonesia1, National Cardiovascular Center Harapan Kita, Indonesia2,
Clinical Information
Patient initials or Identifier Number
GM
Relevant Clinical History and Physical Exam
Male, 51 years old, with chief complaint chest pain during activity. No documented history of acute coronary syndrome in this patient. Risk factor for coronary artery disease was smoking. His blood pressure was 131/71 mmHg, heart rate 62 bpm, respiratory rate 22 x/minute, oxygen saturation 99% room air.
Relevant Test Results Prior to Catheterization
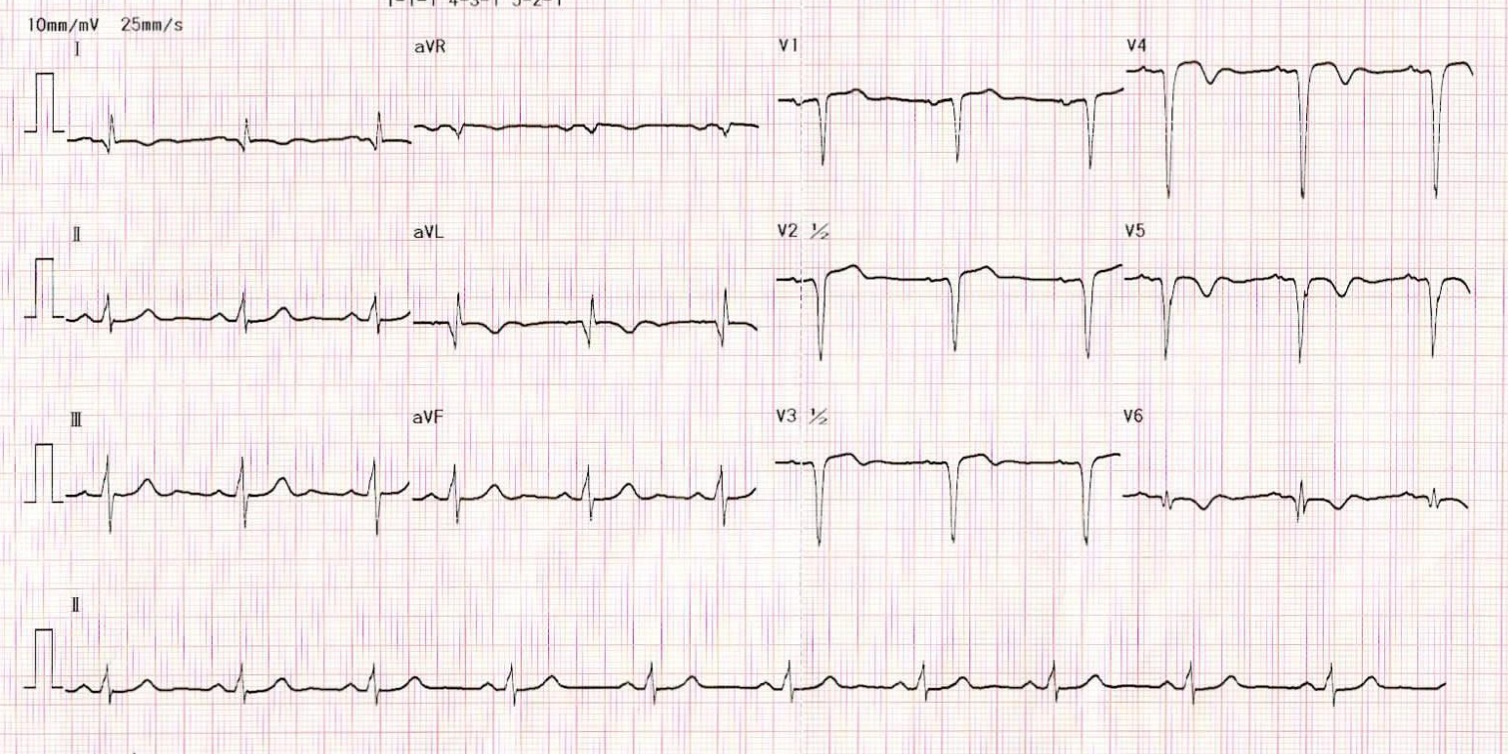
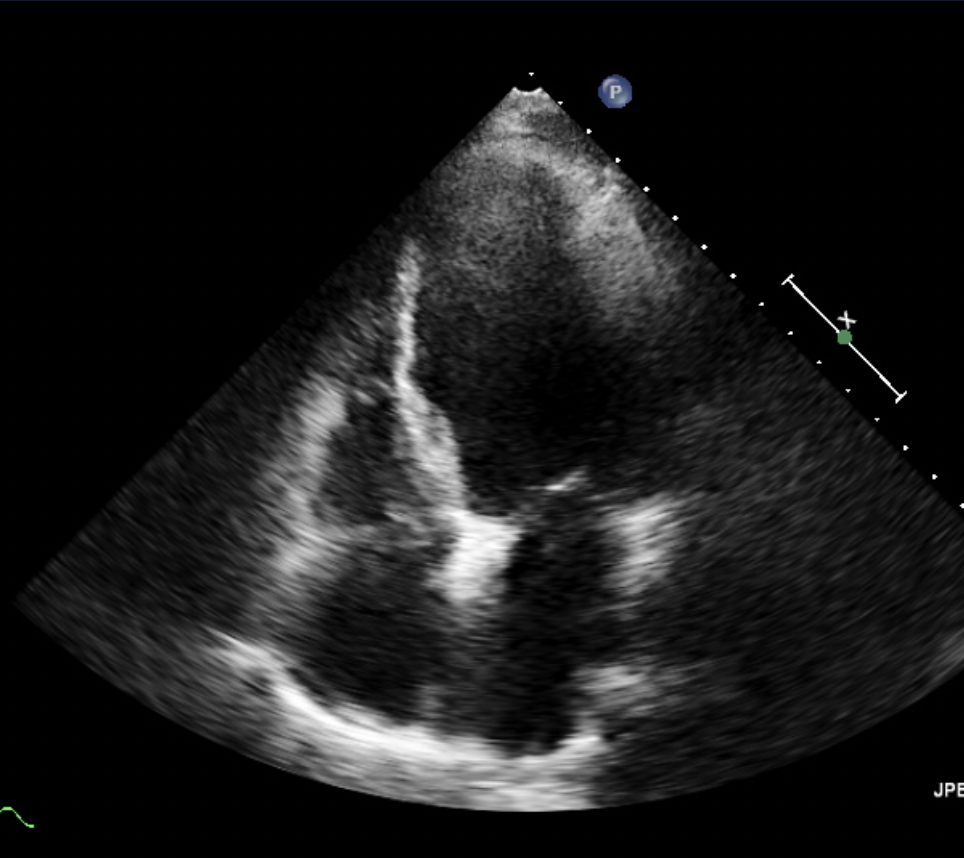
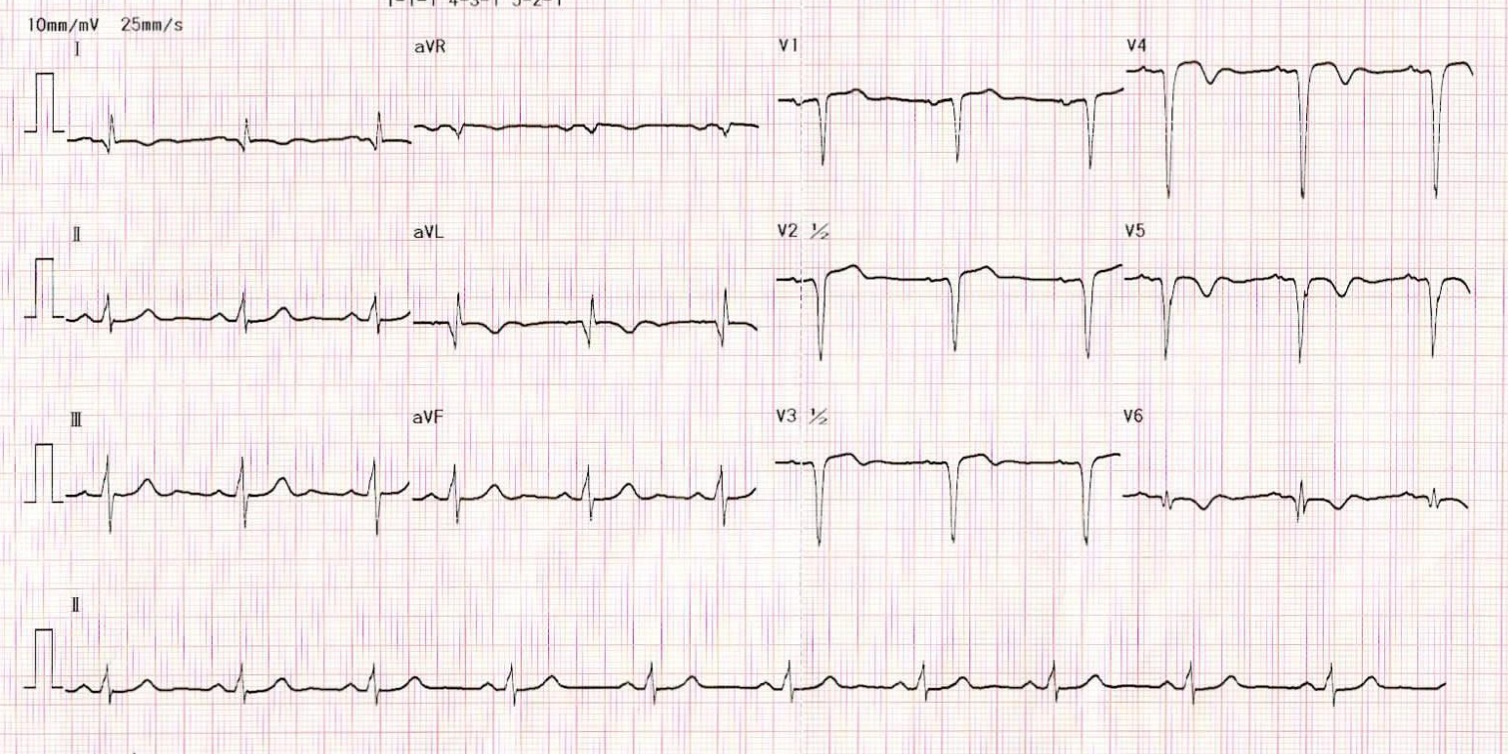
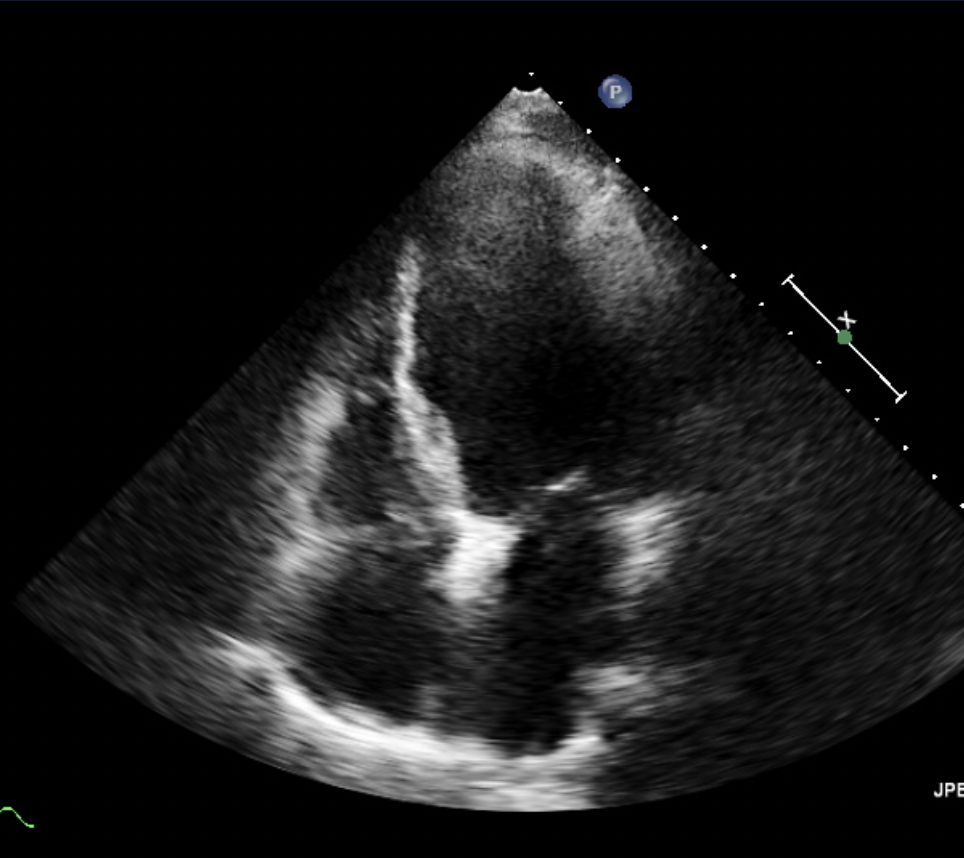
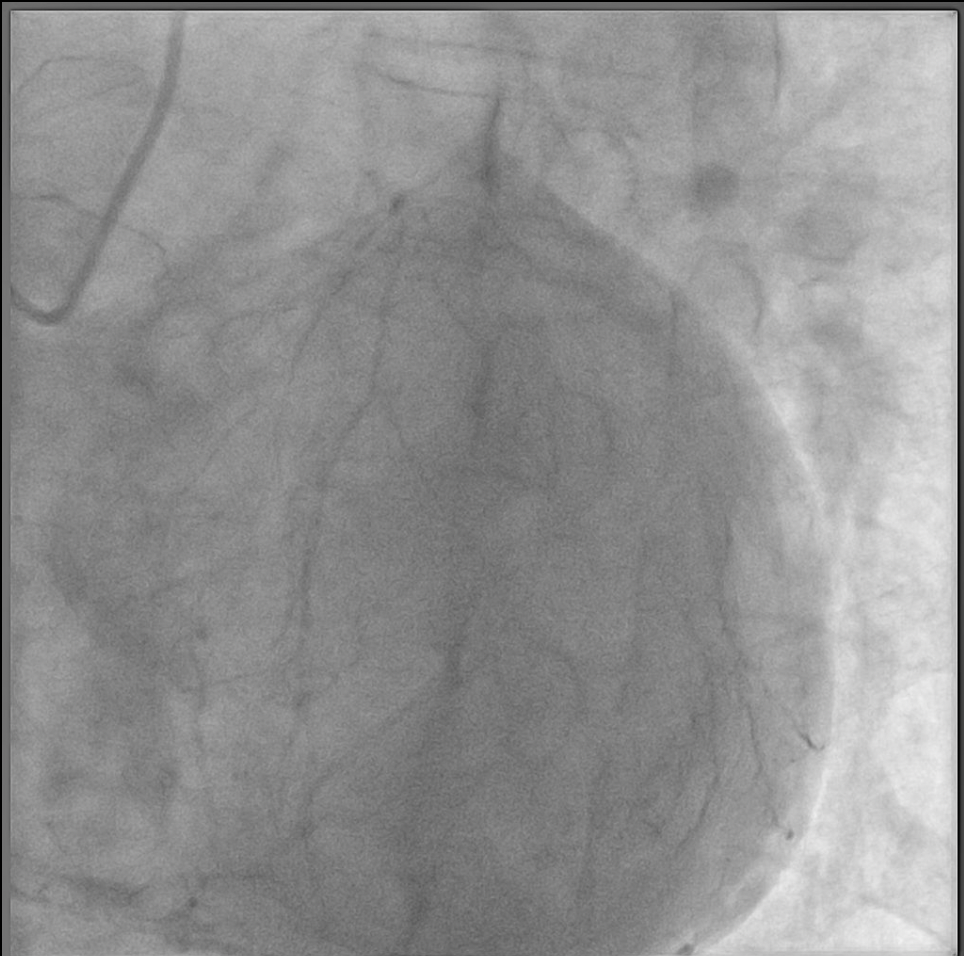
ECG showed anterior extensive Q waves (I, AVL, V1-V6) with inverted T waves at anterolateral (I, AVL, V3-V6). Echocardiography showed LVEF 28%, normal RV systolic function with TAPSE 22 mm, hypokinetic at apical anterior, anteroseptal, and anterolateral, diastolic dysfunction grade II, and mild MR.
Relevant Catheterization Findings
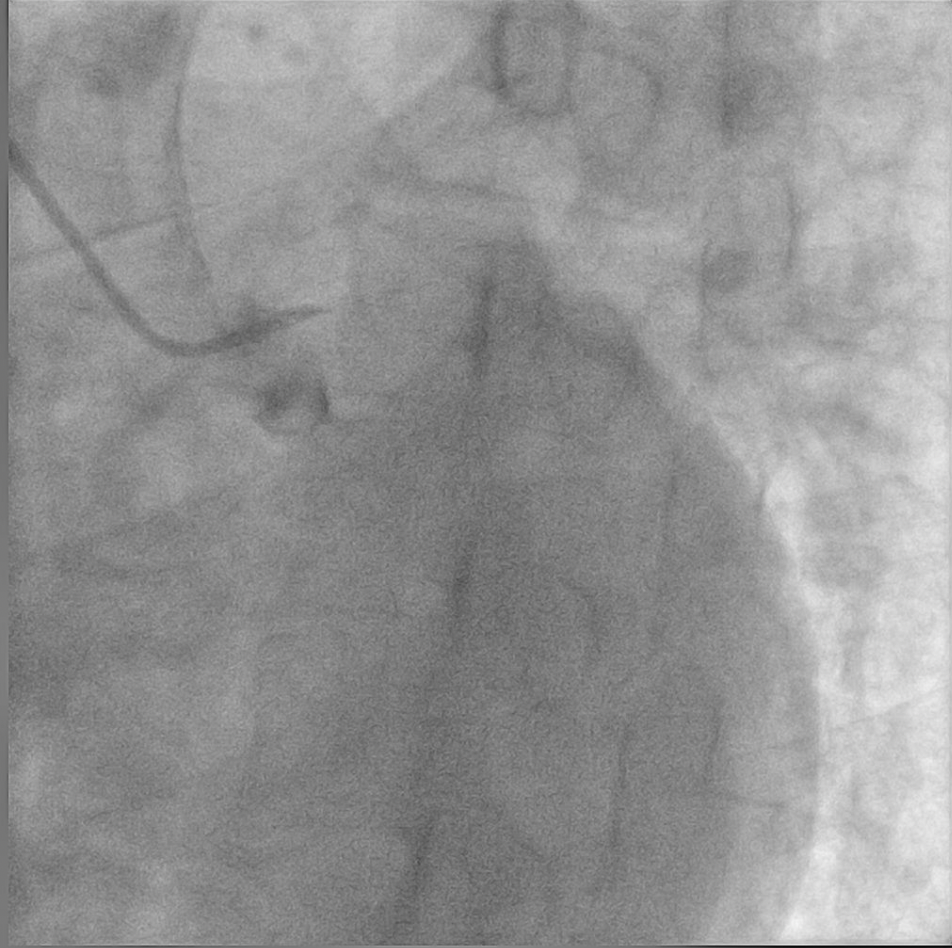
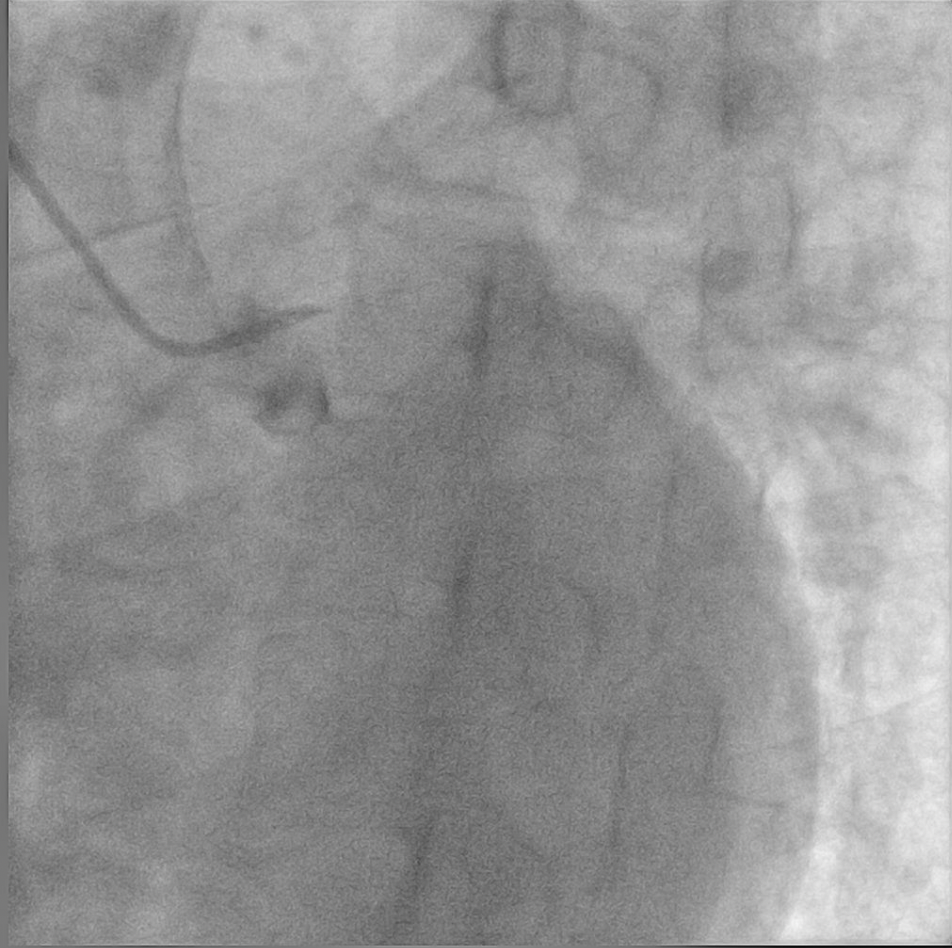
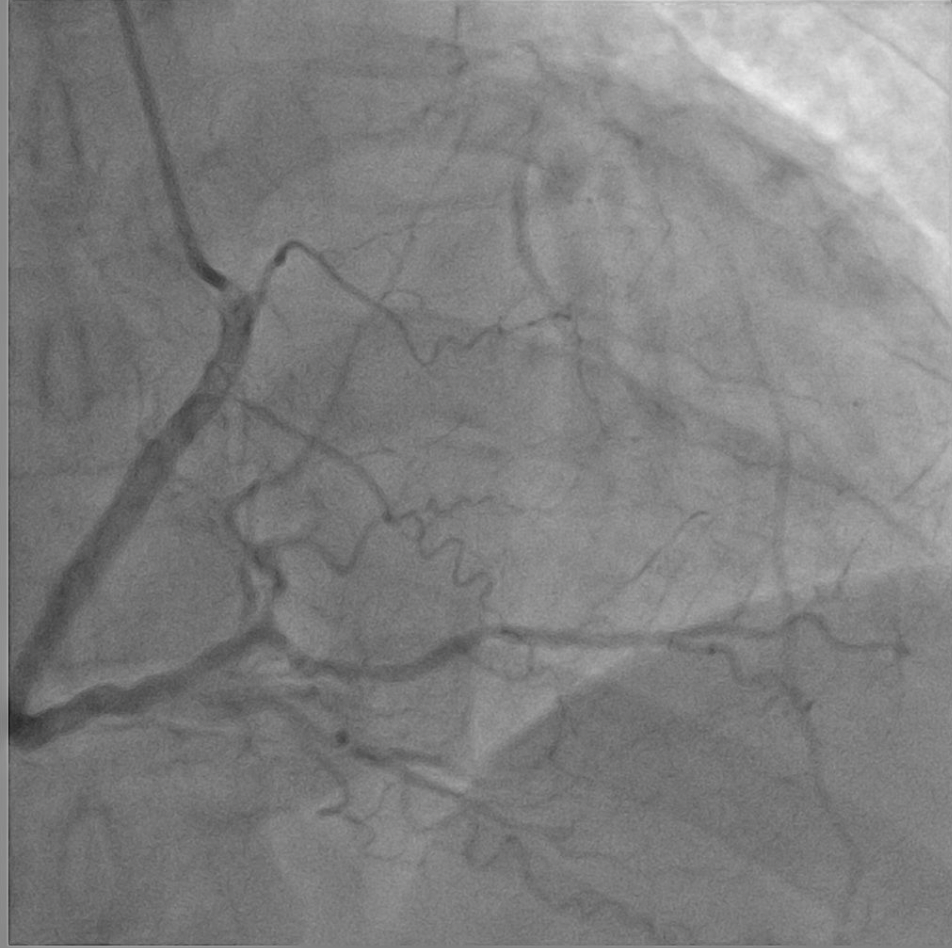
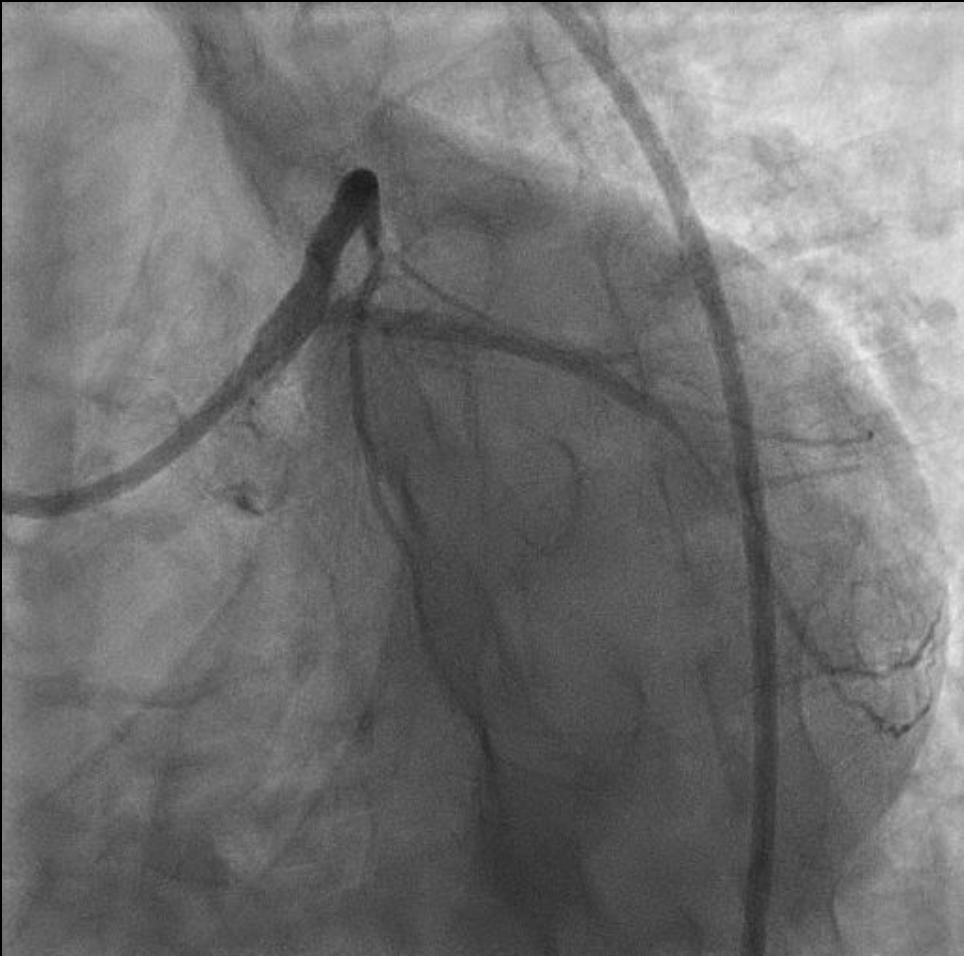
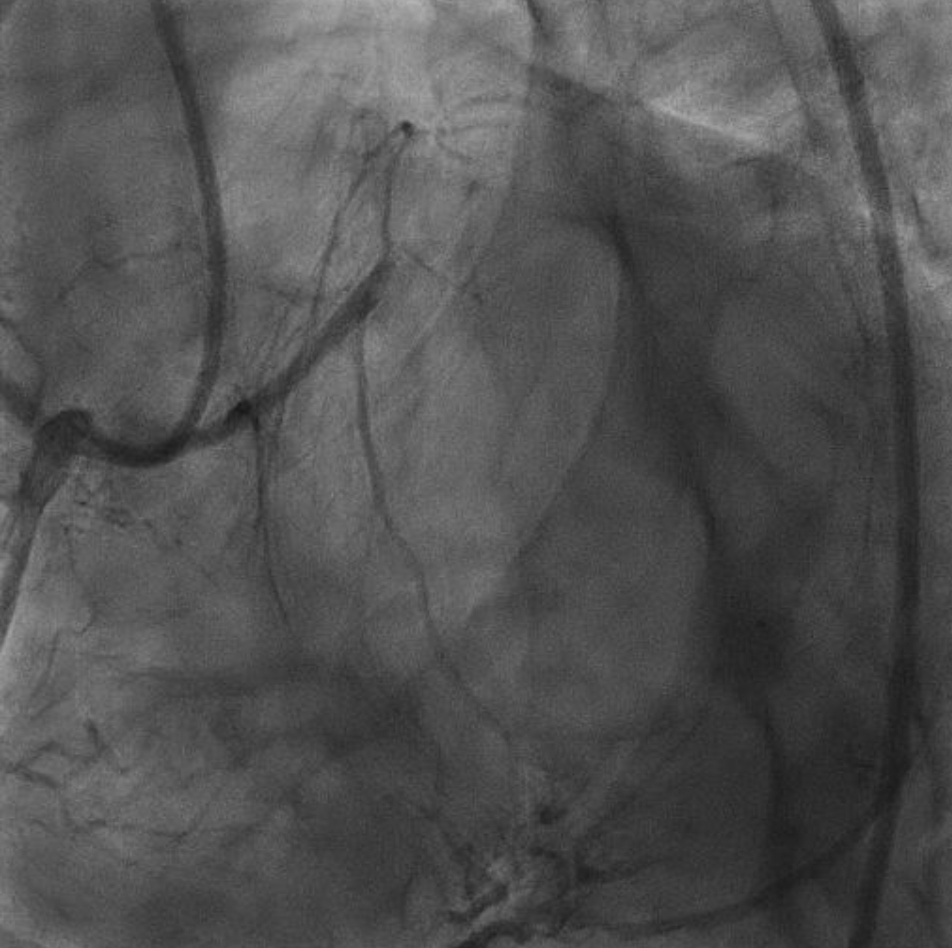
Angiography data showed CTO at proximal LM, subsequently LAD and LCx received collateral from contralateral rentrop III, RCA dominant normal. CTO assessment: tapered lesion, calcified, lesion with length more then 20 mm (JCTO score: 3). PCI strategy: dual angiography injection, antegrade CTO approach, and two stent bifurcation strategy with intravascular imaging.
Interventional Management
Procedural Step
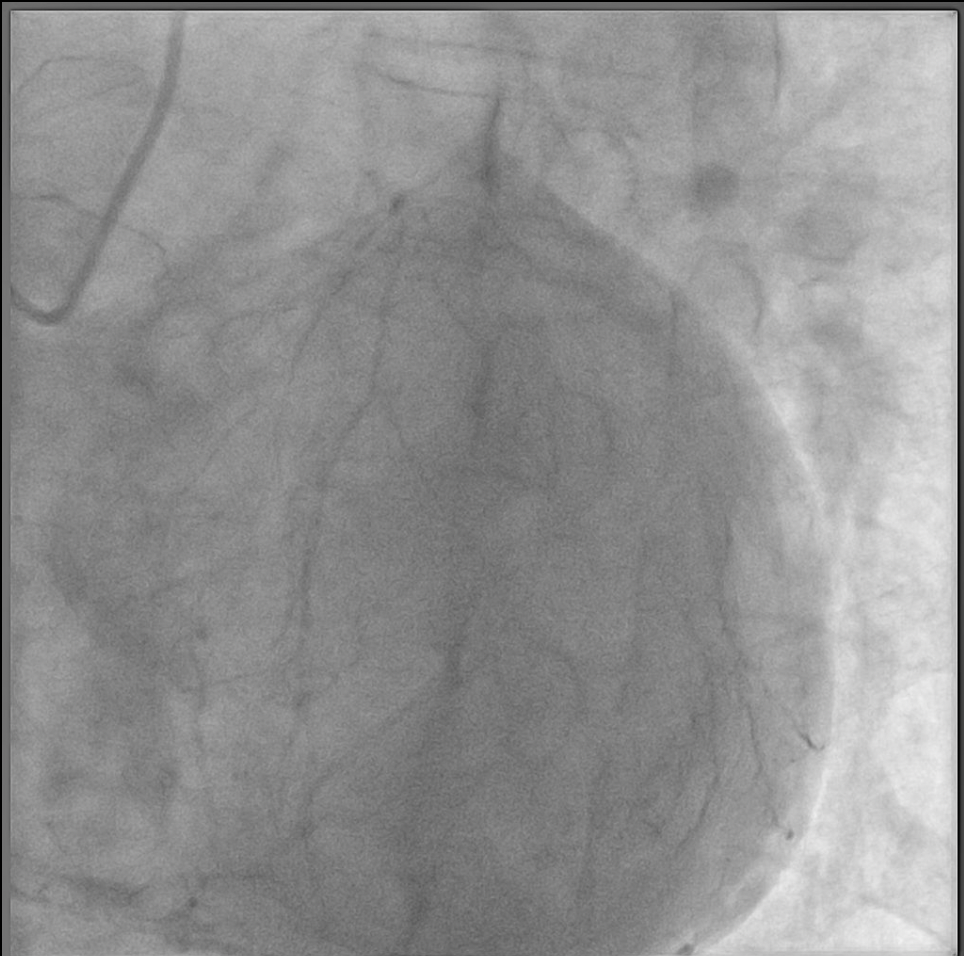
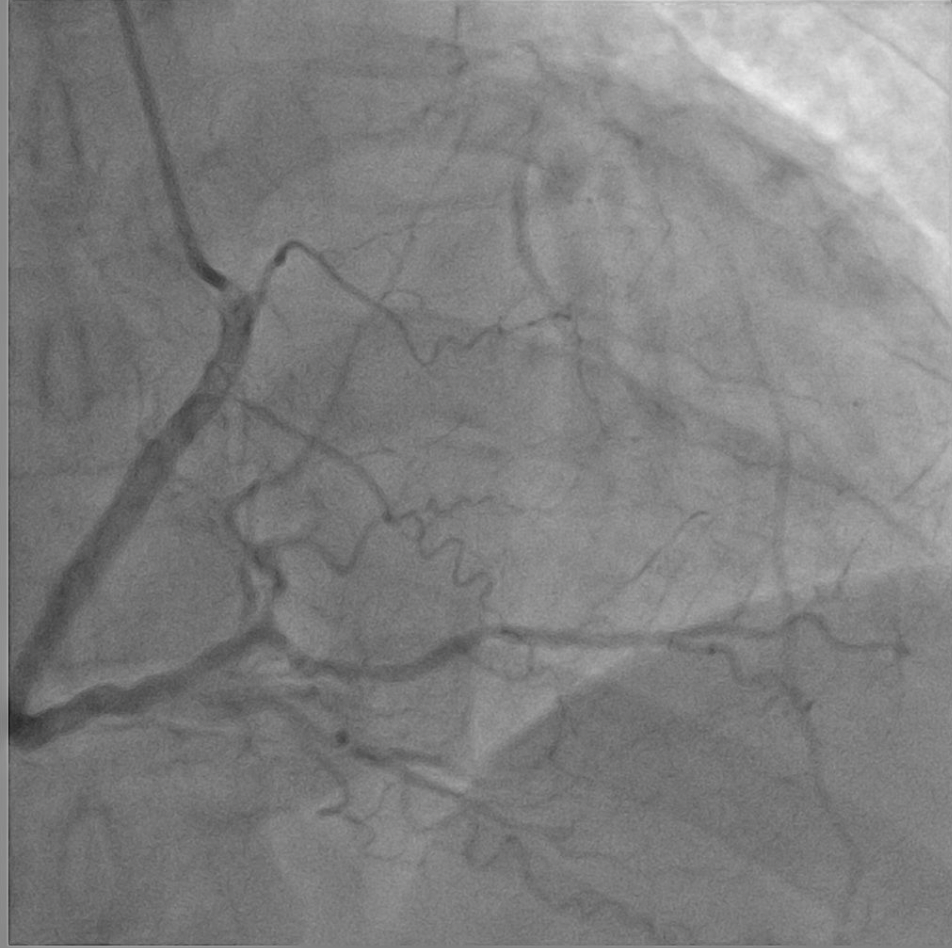
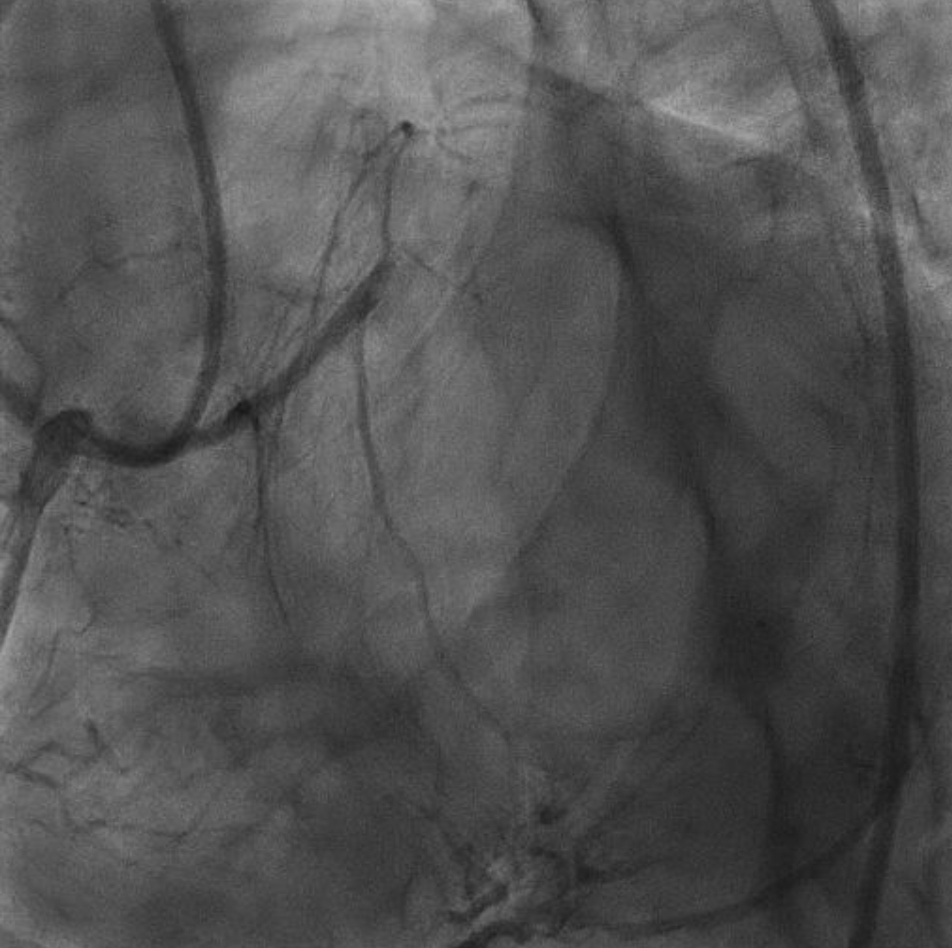
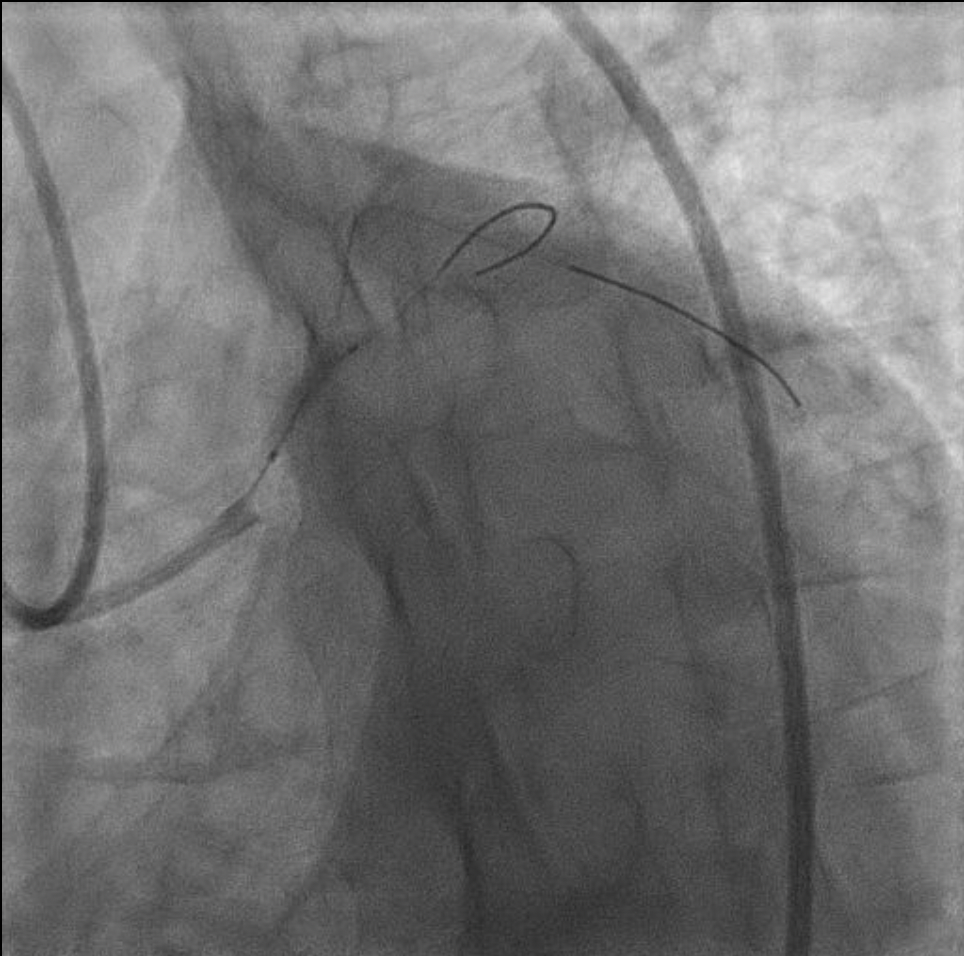
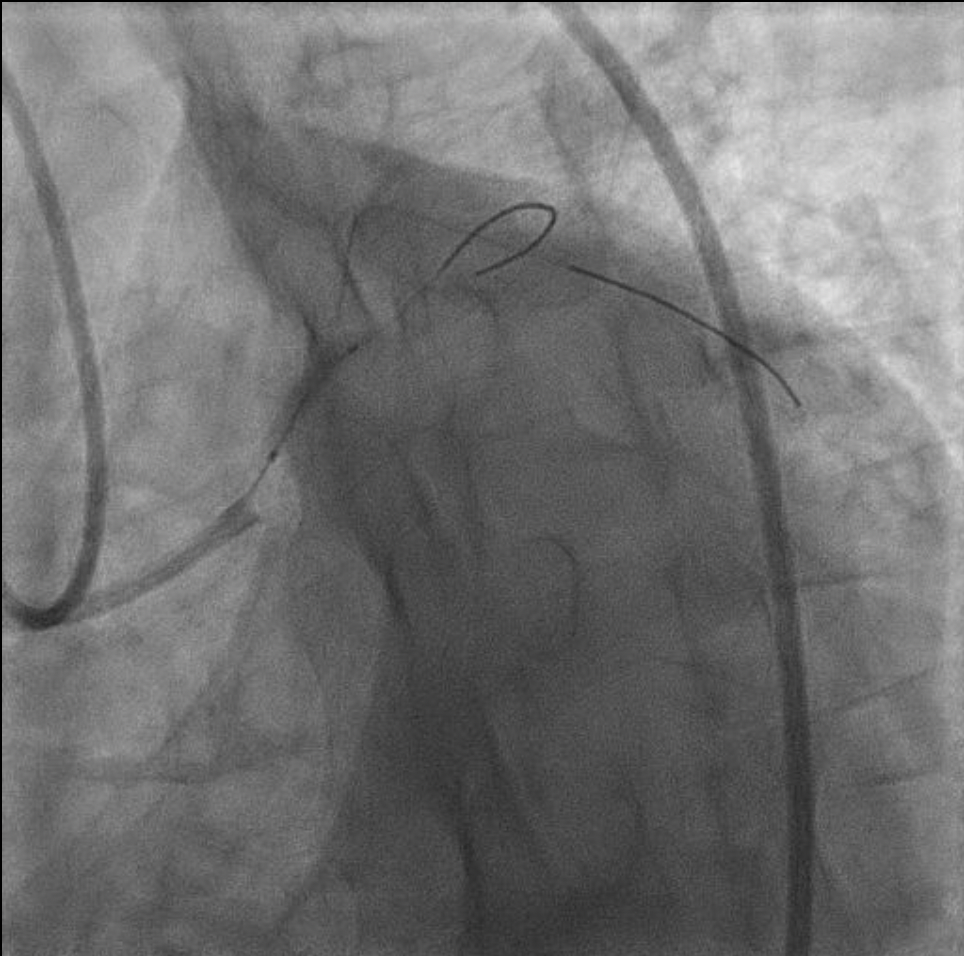
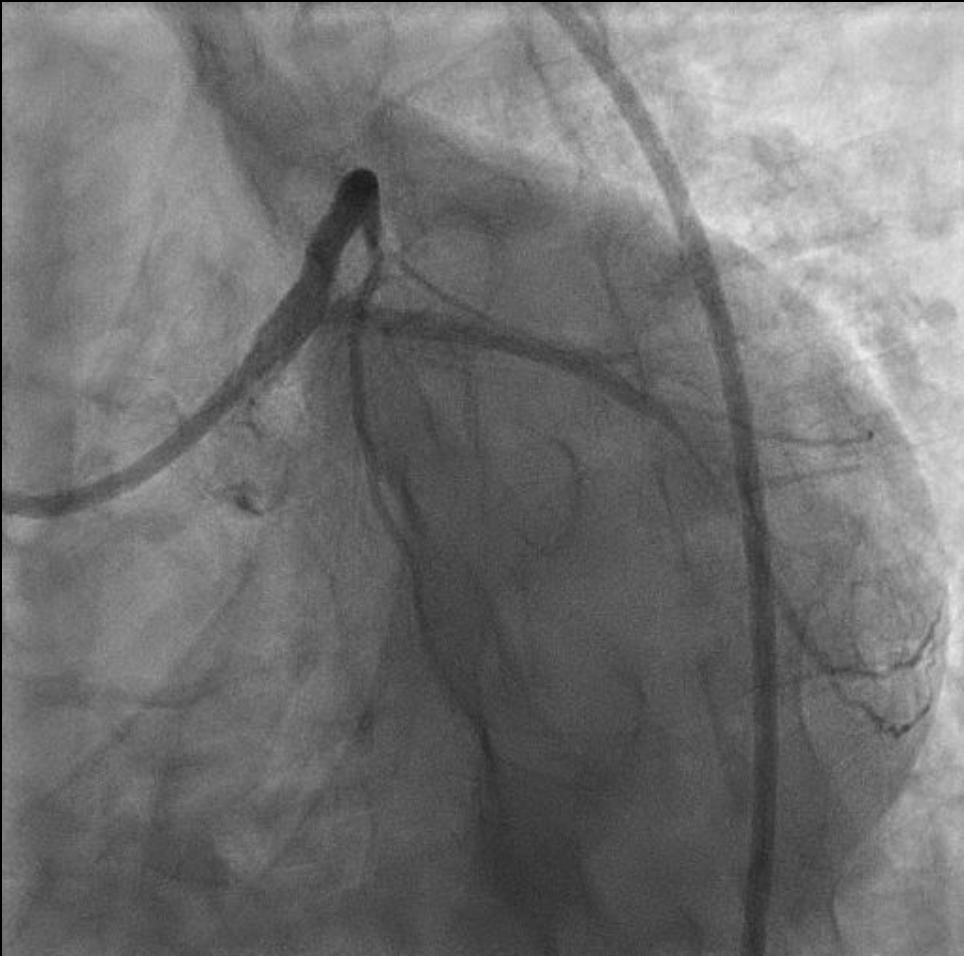
We performed PCI at LM CTO with dual injection strategy, right femoral access using guiding catheter XB 3.5/7F and diagnostic catheter JR 3.5/6F on the right radial. LM CTO was successfully crossed using wire Ashahi Fielder XT-A with microcatheter backup through to D1. Subsequently we exchanged wire at D1 with Runthrough Floppy, tried further to pass dLAD using wire Ashahi Fielder XT-A, and succeeded. Predilatation of LM-proximal LAD was performed using SC balloon 2.5/15 mm. Our next step was wiring to distal LCx using wire Ashahi Fielder XT-A with microcatheter backup, and predilated LM-proximal LCx using SC balloon 2.5/15 mm. Pre-PCI IVUS to LM-LAD and LM-LCx found fibrous-calcified plaque. Proximal-mid LAD was stented with DES 3.0/38 mm inflated to 14 atm, and stenting LM-proximal LAD using DES 3.5/38 mm inflated to 18 atm. LM optimized using NC balloon 4.0/12 mm inflated up to 20 atm. Osteal-proximal LCx predilated with SC balloon 2.5/15 mm and stented using DES 2.75/38 mm inflated to 14 atm. Then we performed kissing balloon technique using NC balloon 4.0/12 mm and ex-stent balloon 2.75/38 mm. We optimized LM again with NC balloon 4.0/12 mm inflated to 20 atm. Post PCI IVUS showed mild medial stent edge dissection at distal LAD without flow limitation, stents were well apposed with good expansion. Final angiography showed TIMI 3 flow, no residual stenosis nor thrombus. Patient was stable hemodynamically without any complain.
Case Summary
Based on the evidence, PCI in CTO LM is infrequently performed and mainly used in patients prior to CABG. PCI in LM CTO associated with favorable procedural outcome. Good lesion assessment and strategies before procedure is mandatory.


