Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-005
An Evil From the Past
By Kai Soon Liew, Vijayendran Rajalingam, Yuen Hoong Phang, Pirevina Naidu Krishnan Naidu, Tamim Ansari Bin Jahubar Sathik, Izzatul Nadzirah Binti Ismail, Nur Asmalina Binti Azizan, Kantha Rao Narasamuloo, Saravanan Krishinan, Chee Tat Liew, Dharmaraj Karthikesan
Presenter
Authors
Affiliation
An Evil From the Past
Kai Soon Liew1, Vijayendran Rajalingam2, Yuen Hoong Phang1, Pirevina Naidu Krishnan Naidu3, Tamim Ansari Bin Jahubar Sathik3, Izzatul Nadzirah Binti Ismail3, Nur Asmalina Binti Azizan3, Kantha Rao Narasamuloo1, Saravanan Krishinan4, Chee Tat Liew5, Dharmaraj Karthikesan3
Sultanah Bahiyah Hospital, Malaysia1, Sultan Idris Shah Serdang Hospital, Malaysia2, Hospital Sultanah Bahiyah, Malaysia3, Ministry of Health Malaysia, Malaysia4, Pantai Penang Hospital, Malaysia5,
Clinical Information
Patient initials or Identifier Number
Relevant Clinical History and Physical Exam
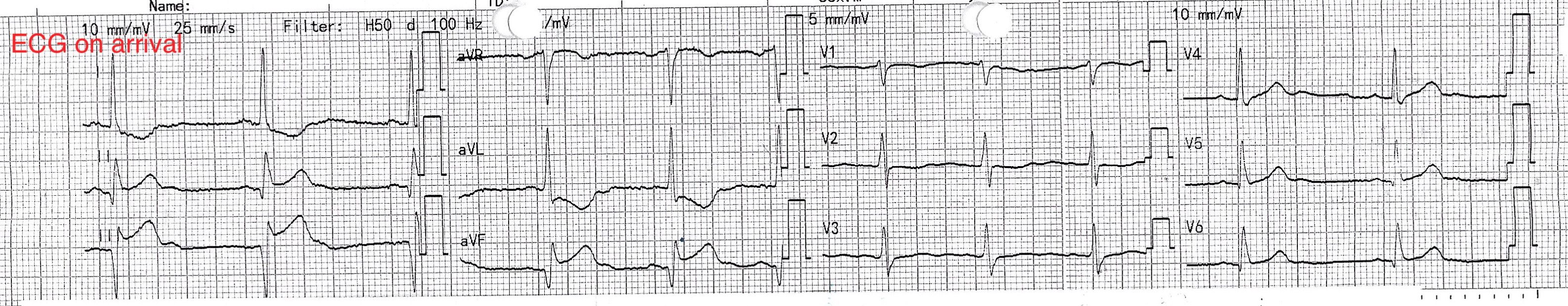
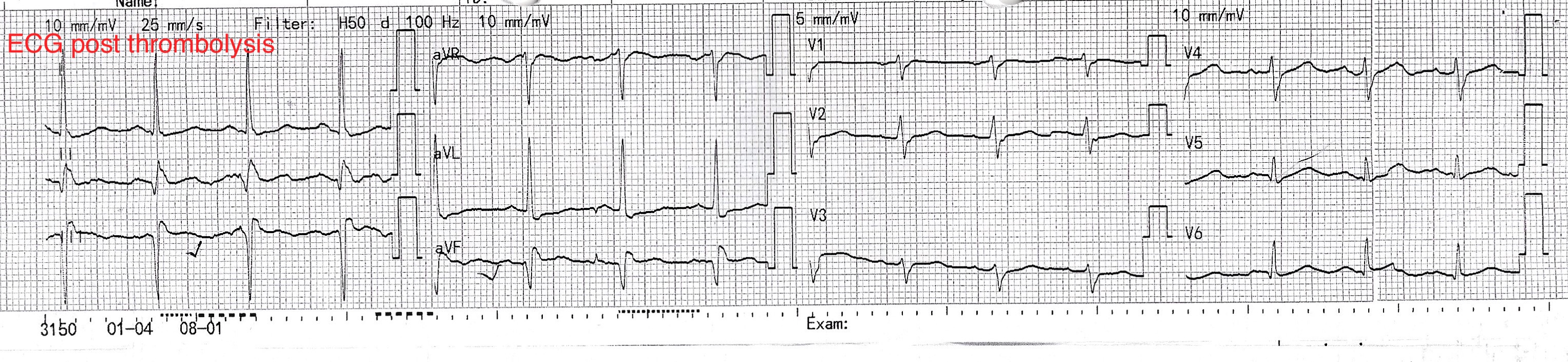
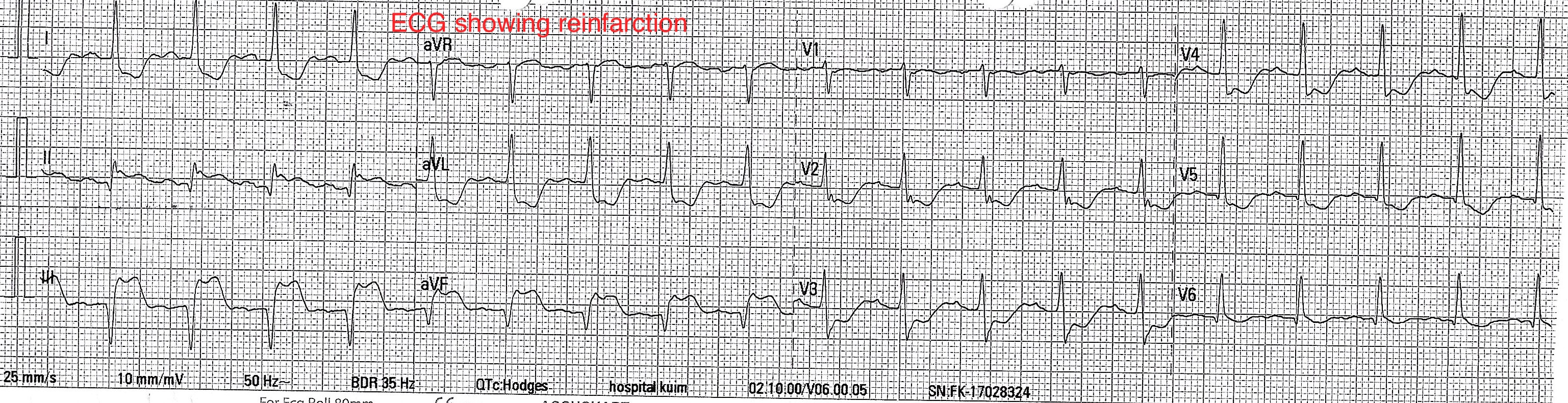
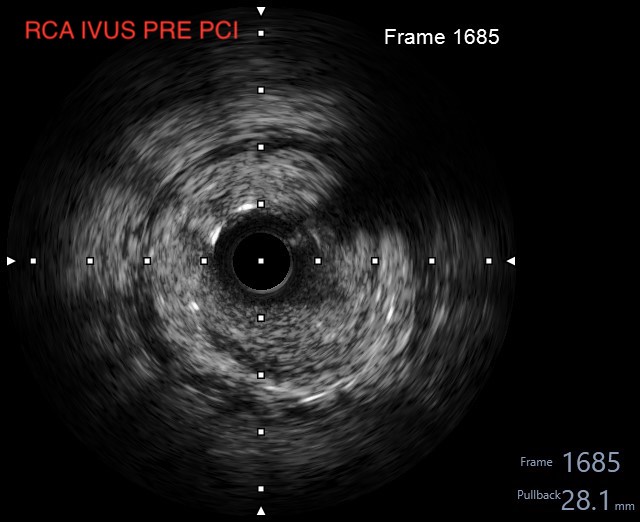
Relevant Test Results Prior to Catheterization
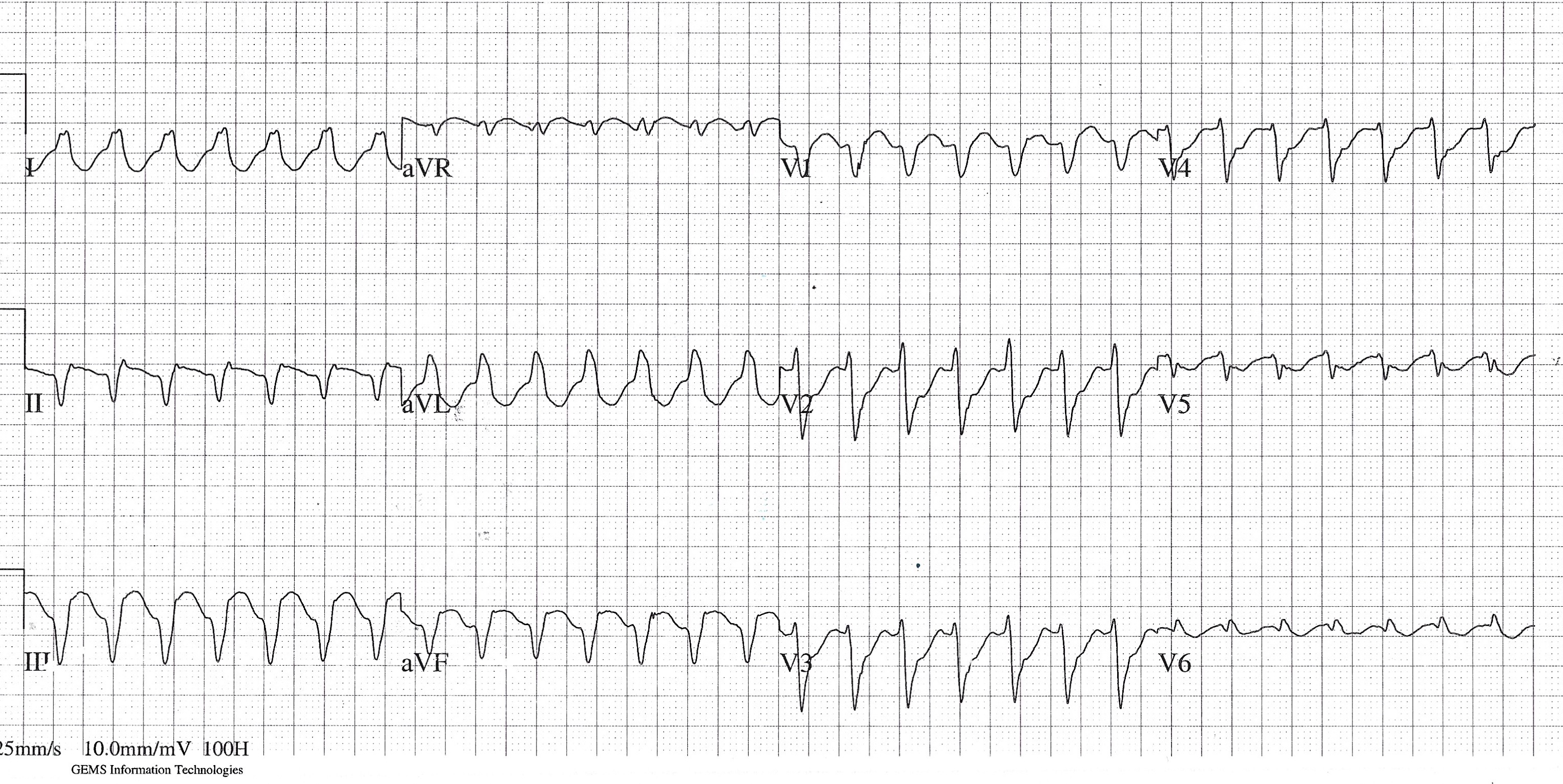
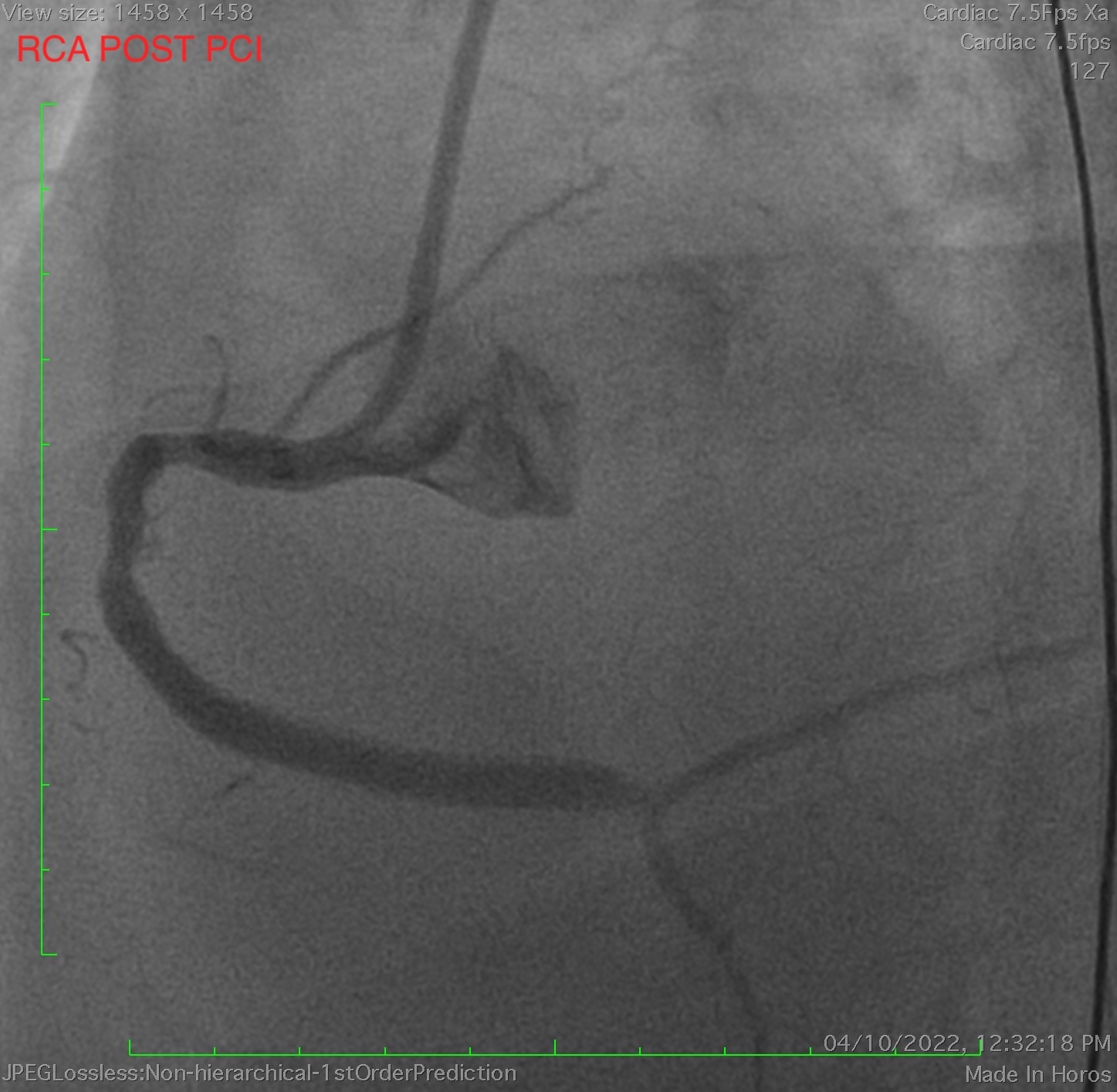
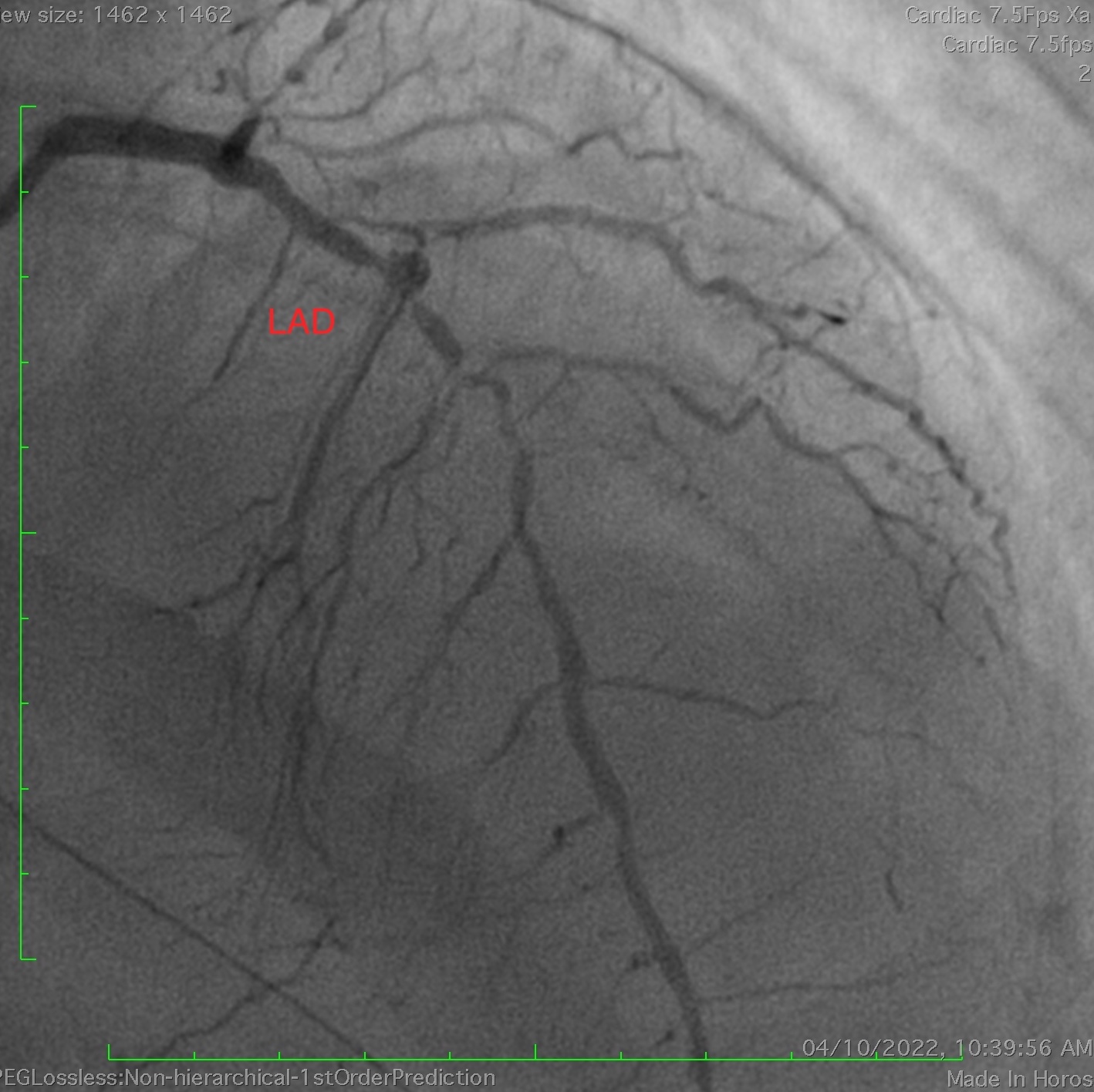
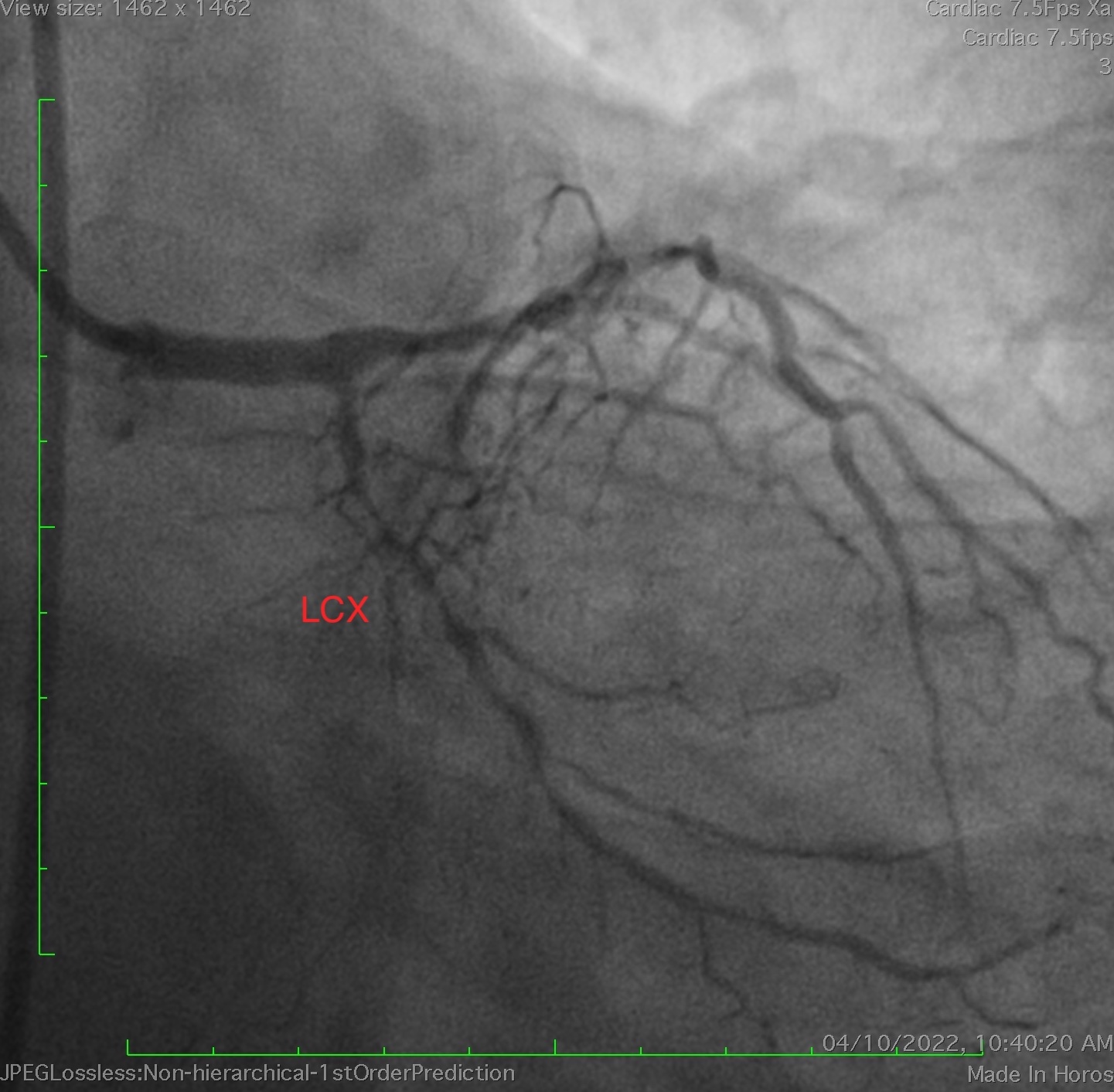
Relevant Catheterization Findings

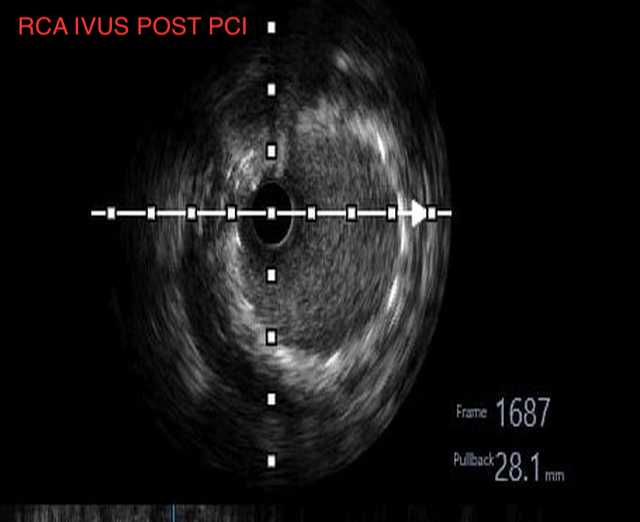
Interventional Management
Procedural Step