Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-203
An Inoperable Non-calcified Severe Aortic Regurgitation Case Treated by Balloon Expandable Transcatheter Aortic Valve Replacement
By Thinnakrit Sasiprapha, Mann Chandavimol, Pavit Pienvichit, Tawai Ngernsritrakul
Presenter
Thinnakrit Sasiprapha
Authors
Thinnakrit Sasiprapha1, Mann Chandavimol1, Pavit Pienvichit1, Tawai Ngernsritrakul1
Affiliation
Ramathibodi Hospital, Thailand1,
View Study Report
TCTAP C-203
STRUCTURAL HEART DISEASE - Valvular Intervention: Aortic
An Inoperable Non-calcified Severe Aortic Regurgitation Case Treated by Balloon Expandable Transcatheter Aortic Valve Replacement
Thinnakrit Sasiprapha1, Mann Chandavimol1, Pavit Pienvichit1, Tawai Ngernsritrakul1
Ramathibodi Hospital, Thailand1,
Clinical Information
Patient initials or Identifier Number
KS
Relevant Clinical History and Physical Exam
A 78-year-old man had presented with progressive dyspnea for 3 months. He was diagnosed with acute de novo heart failure at another hospital. An echocardiogram reported severely impaired LV function and moderate AR. Diuretics and heart failure medications were given. After a month of admission, he was referred to our hospital for further evaluation and treatment. He was in a cachexic and bedridden state. Cardiac auscultation showed a diastolic blowing murmur at the right lower parasternal border.


Relevant Test Results Prior to Catheterization
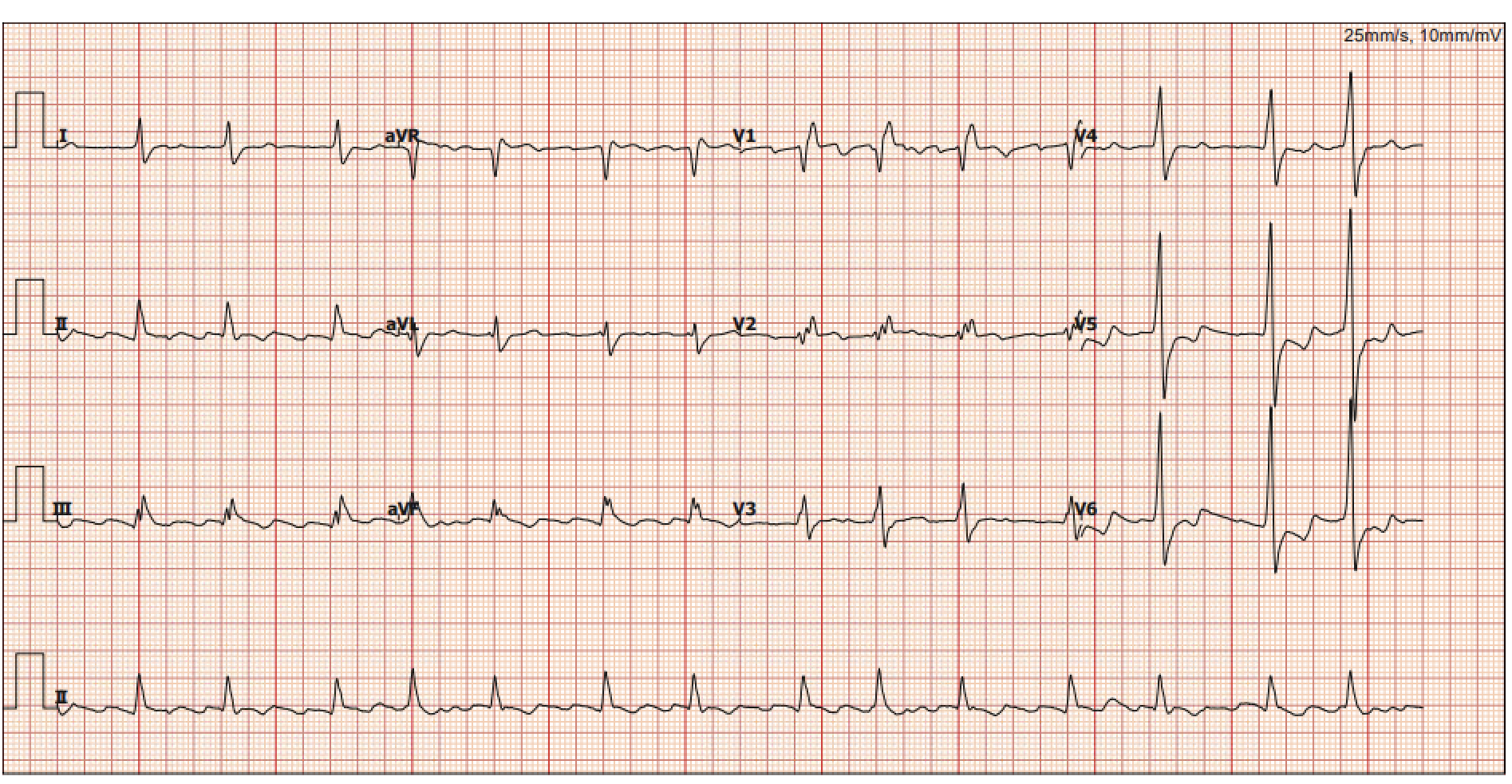
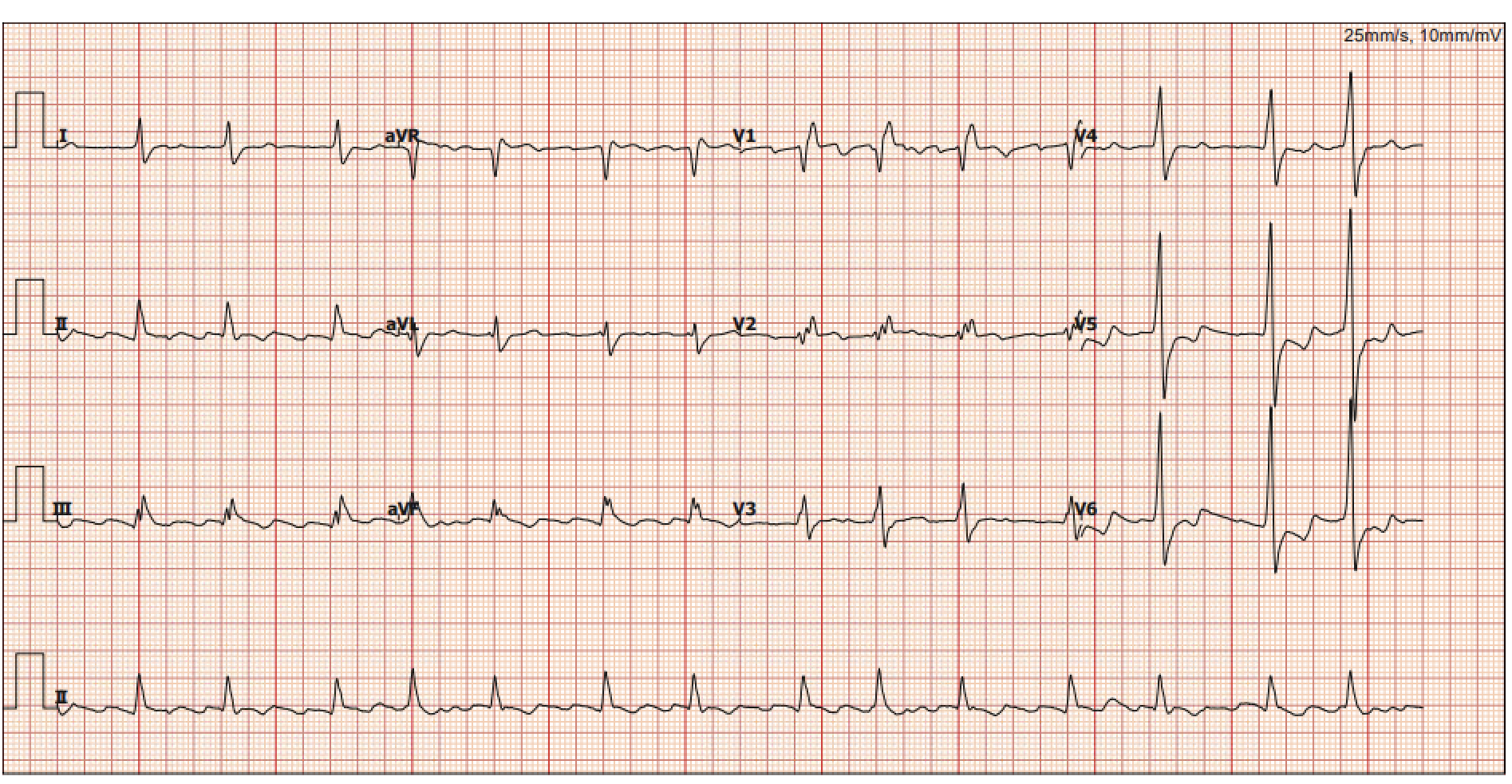
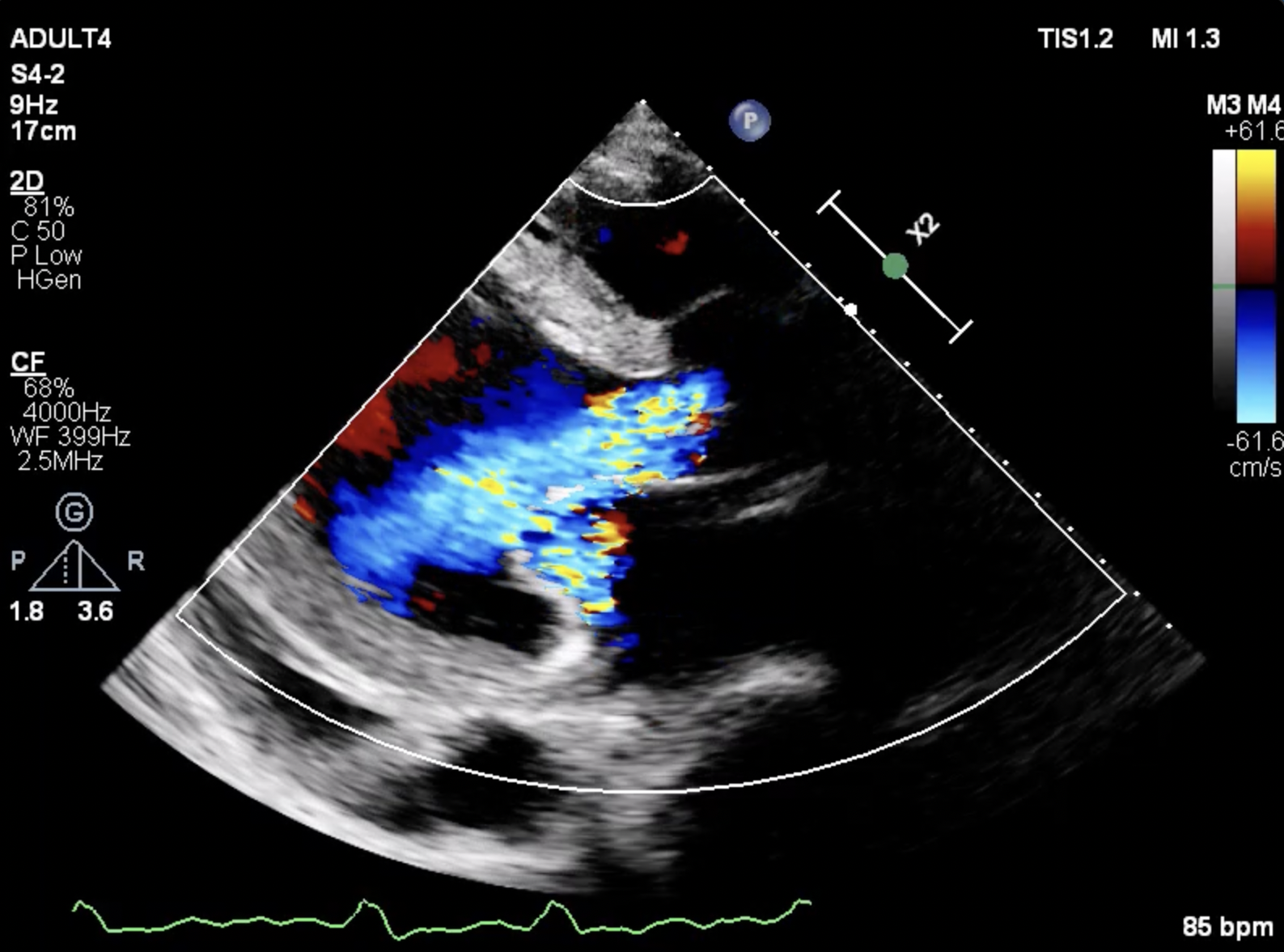
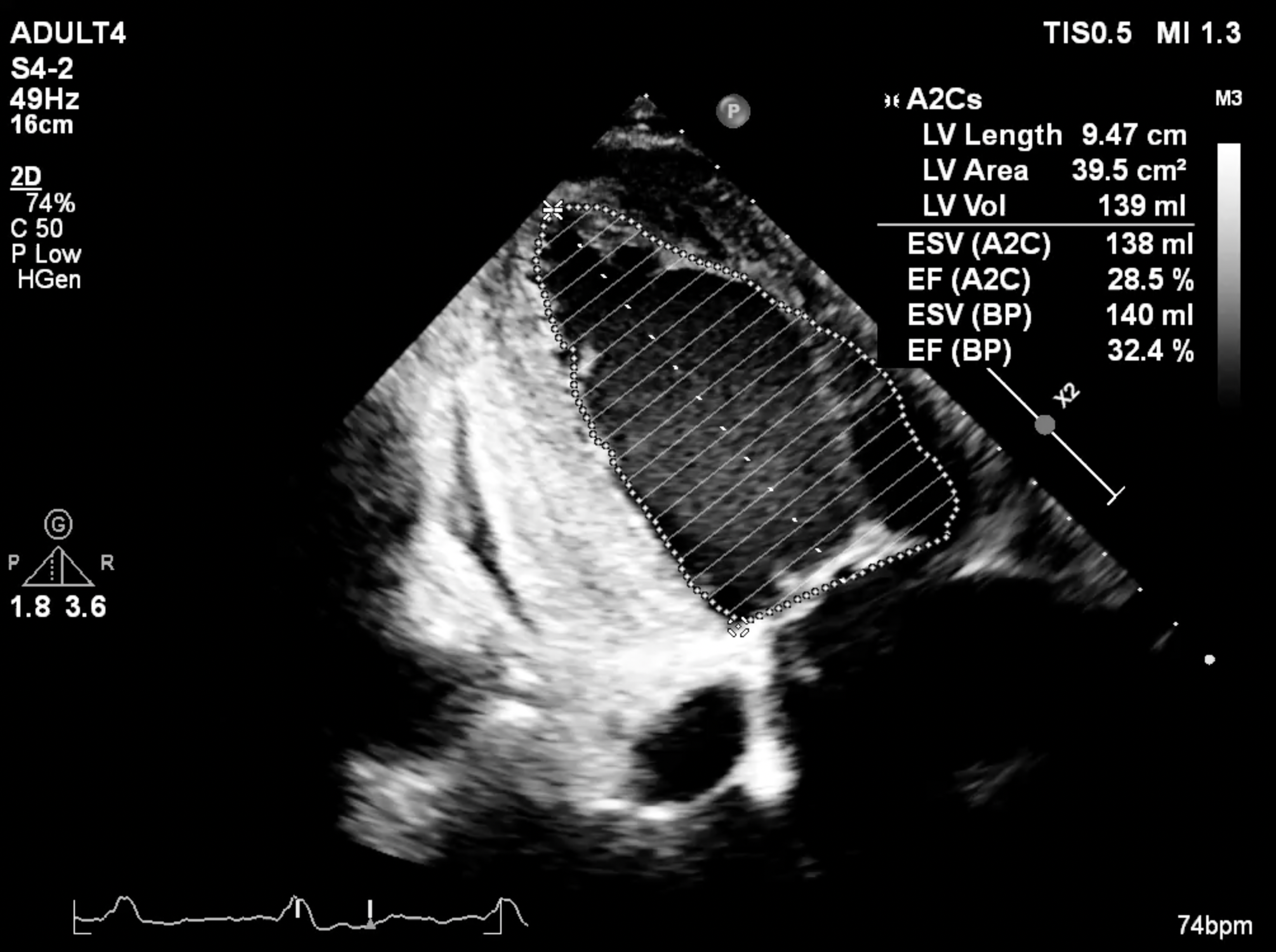
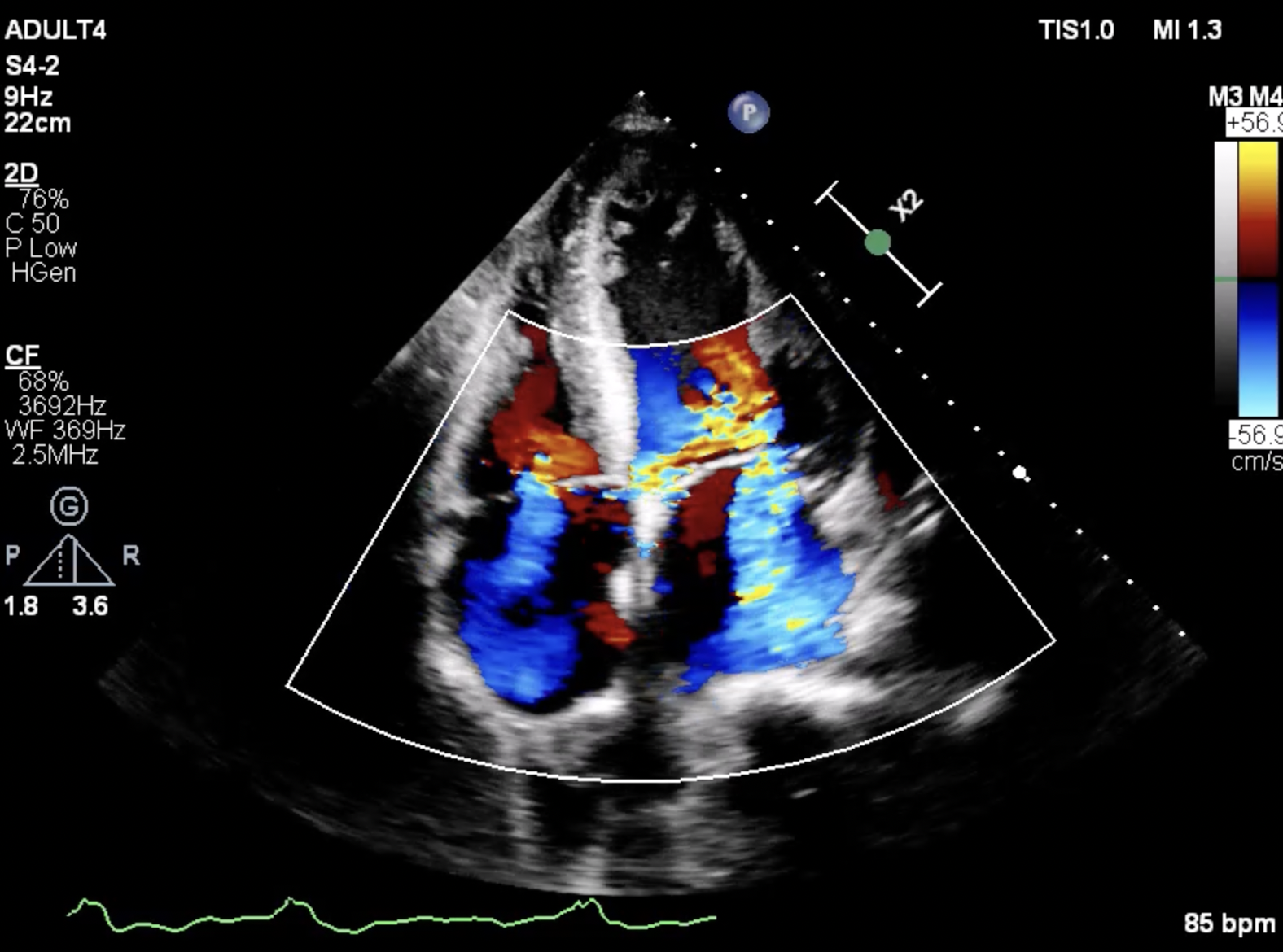
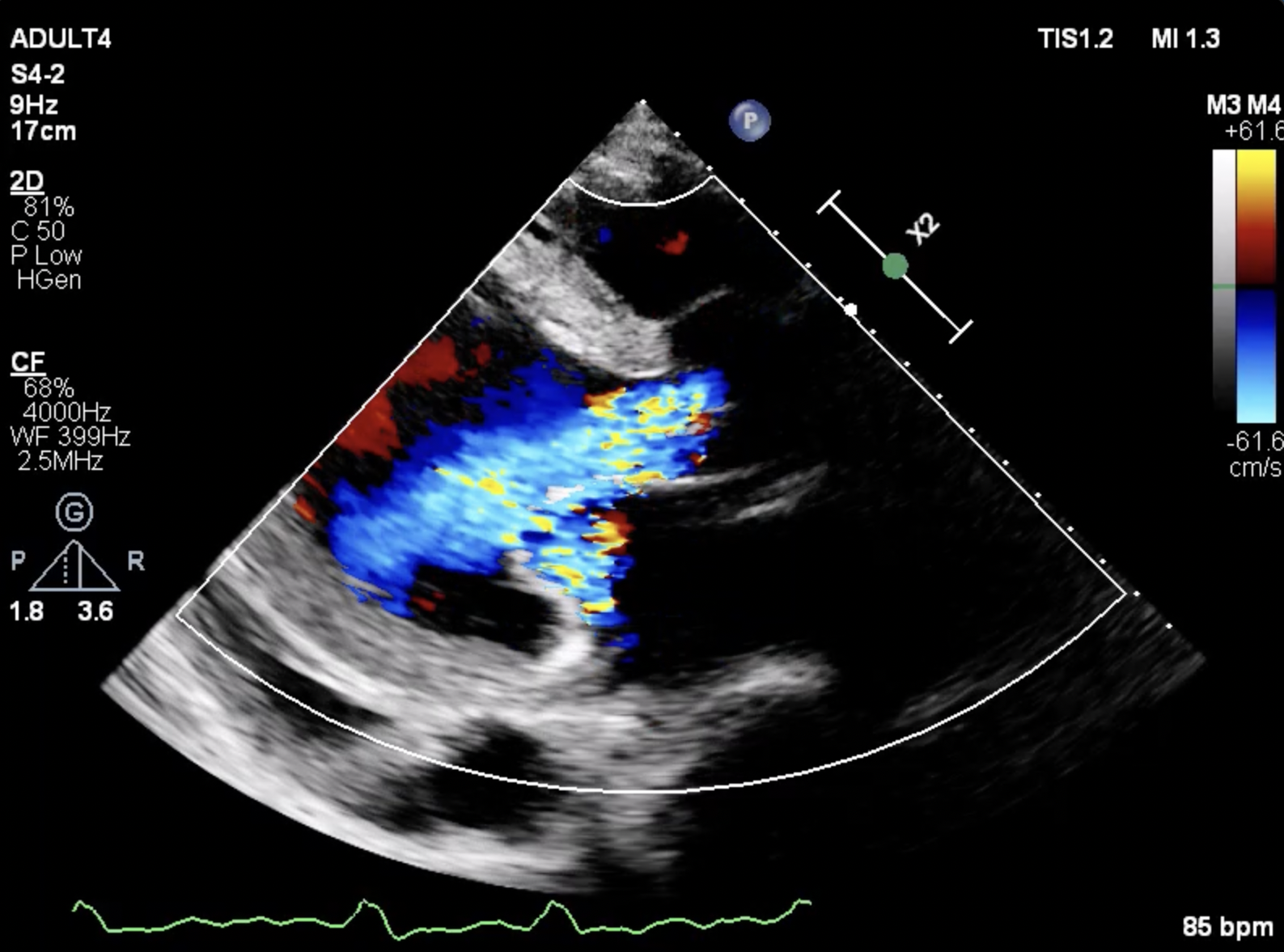
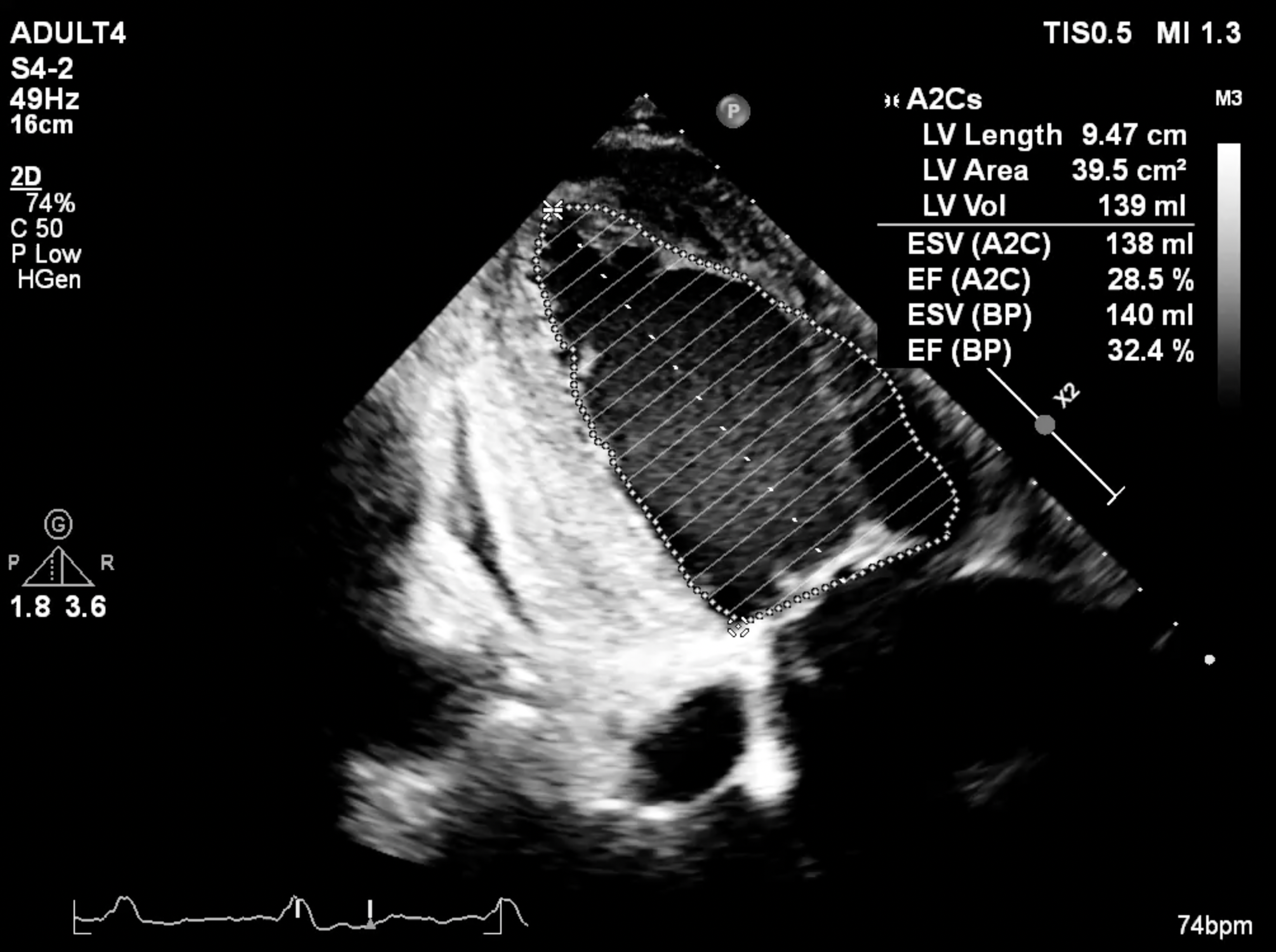
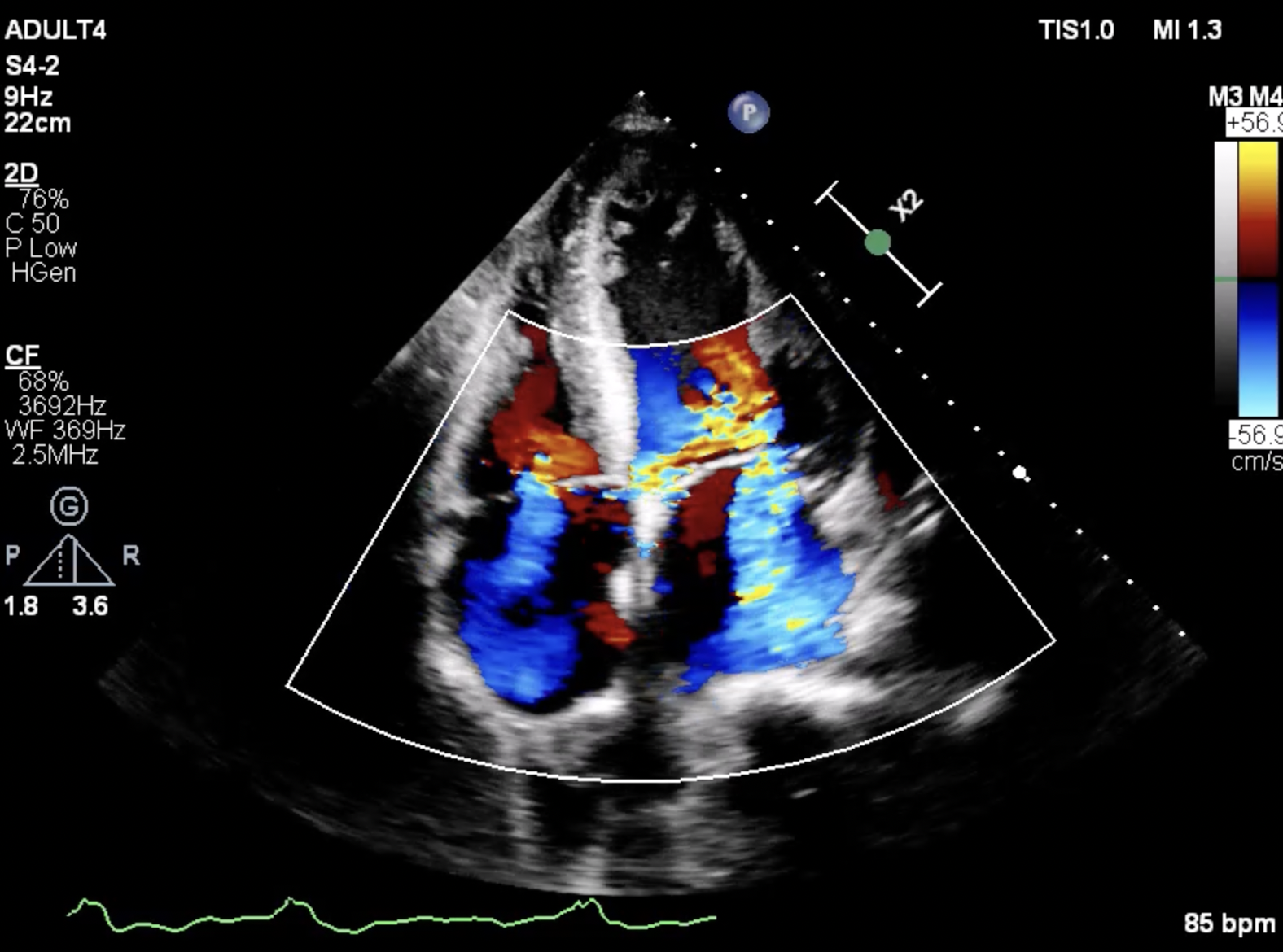
EKG showed atrial fibrillation rhythm with a moderate ventricular response and right bundle branch block morphology. Chest X-ray revealed markedly cardiomegaly with bilateral congestion and pleural effusion. An echocardiogram demonstrated a non-calcified aortic valve with aortic cusp prolapse causing severe aortic regurgitation. Severely dilated and impaired LV systolic function, moderate to severe functional mitral regurgitation, and trace pericardial effusion was also noted.
Relevant Catheterization Findings
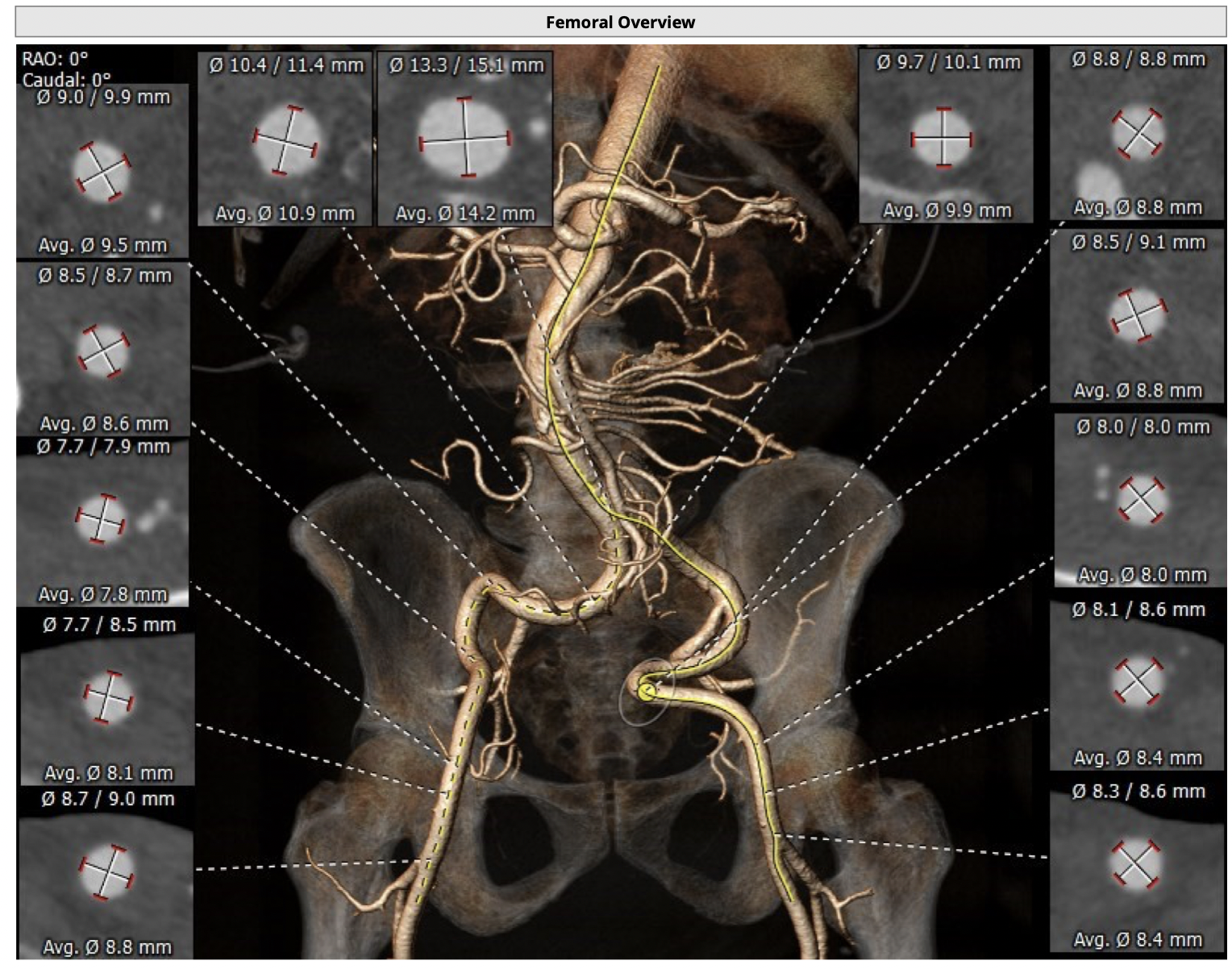
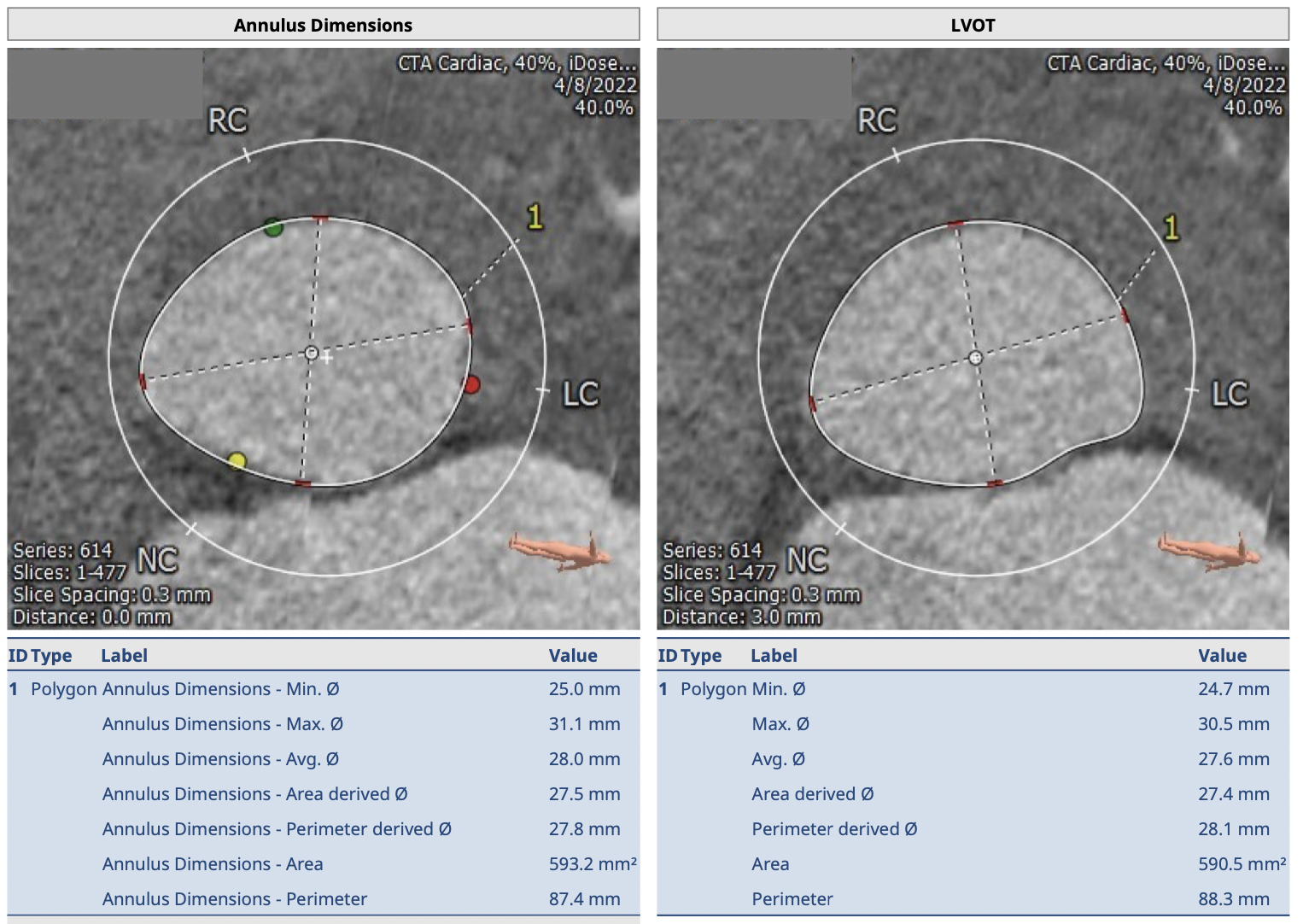
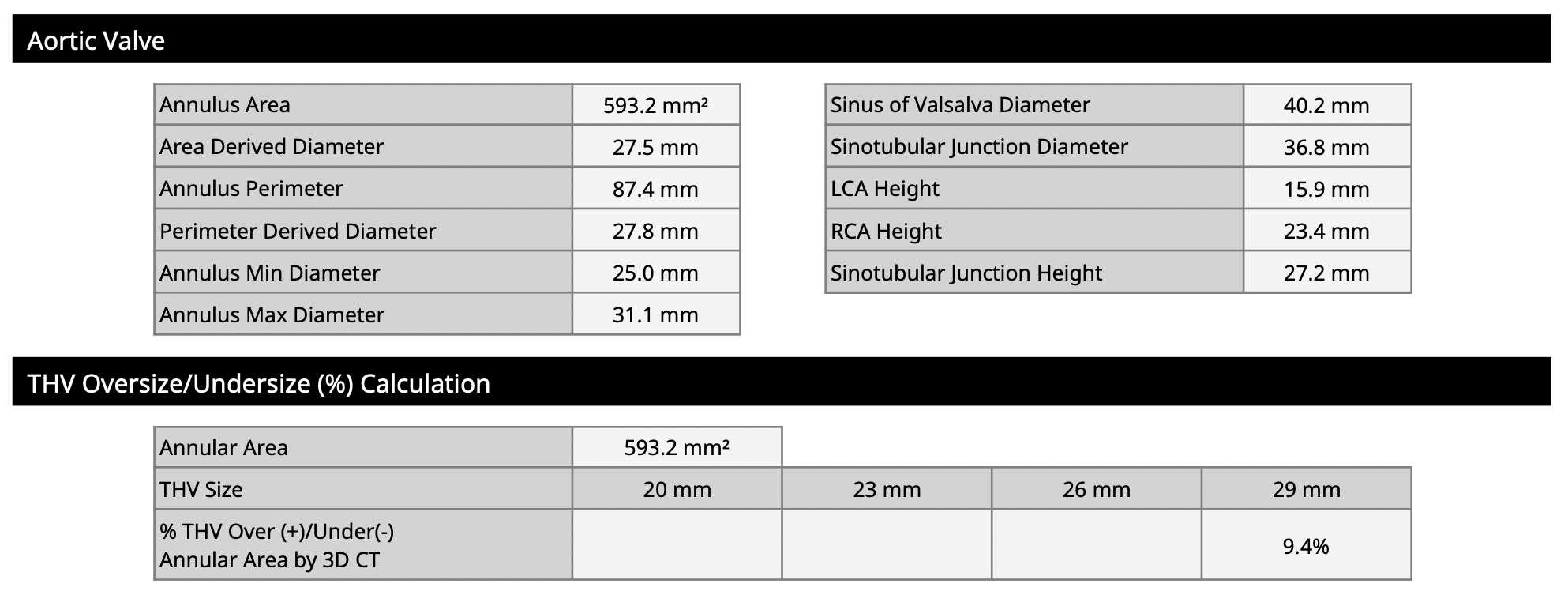
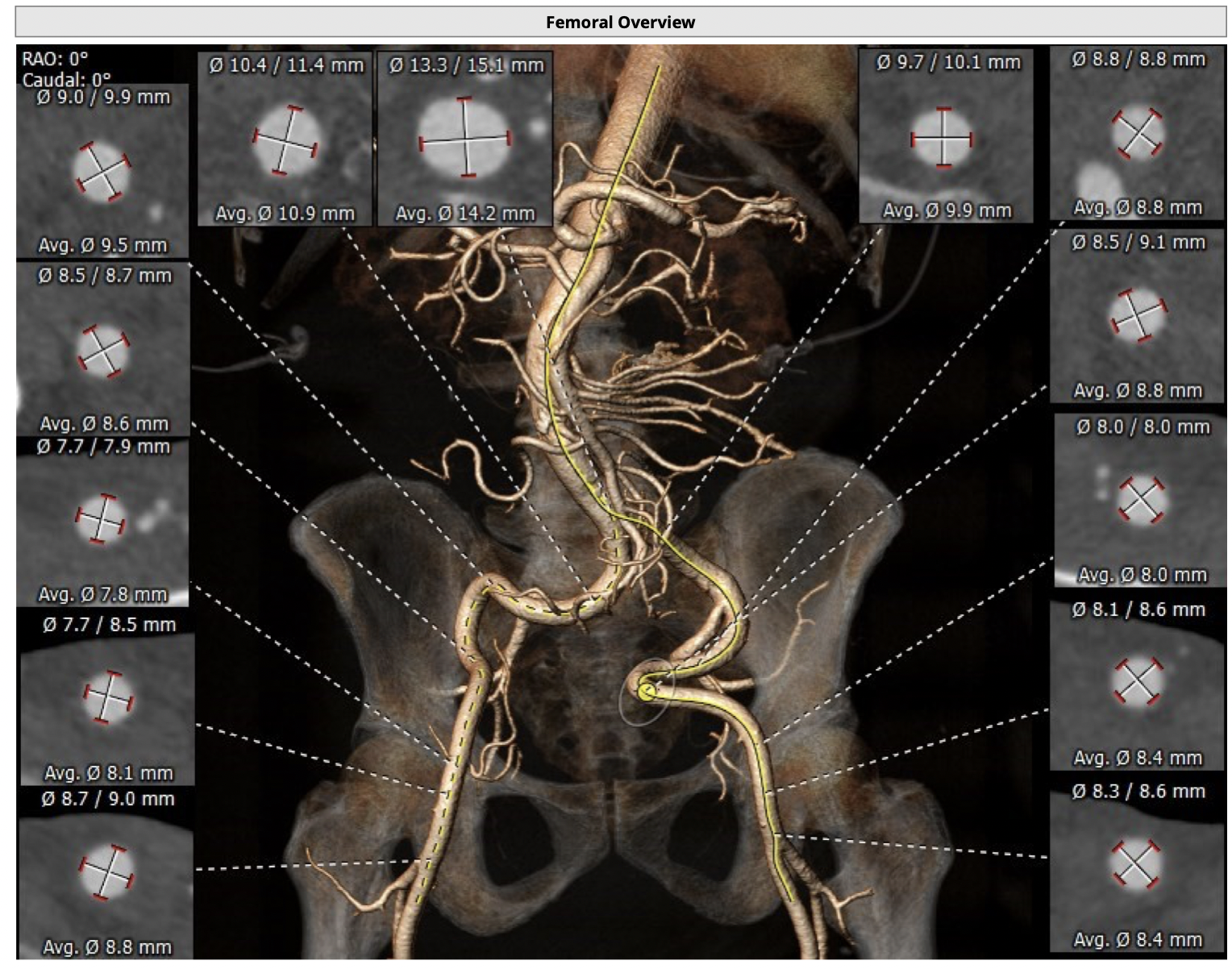
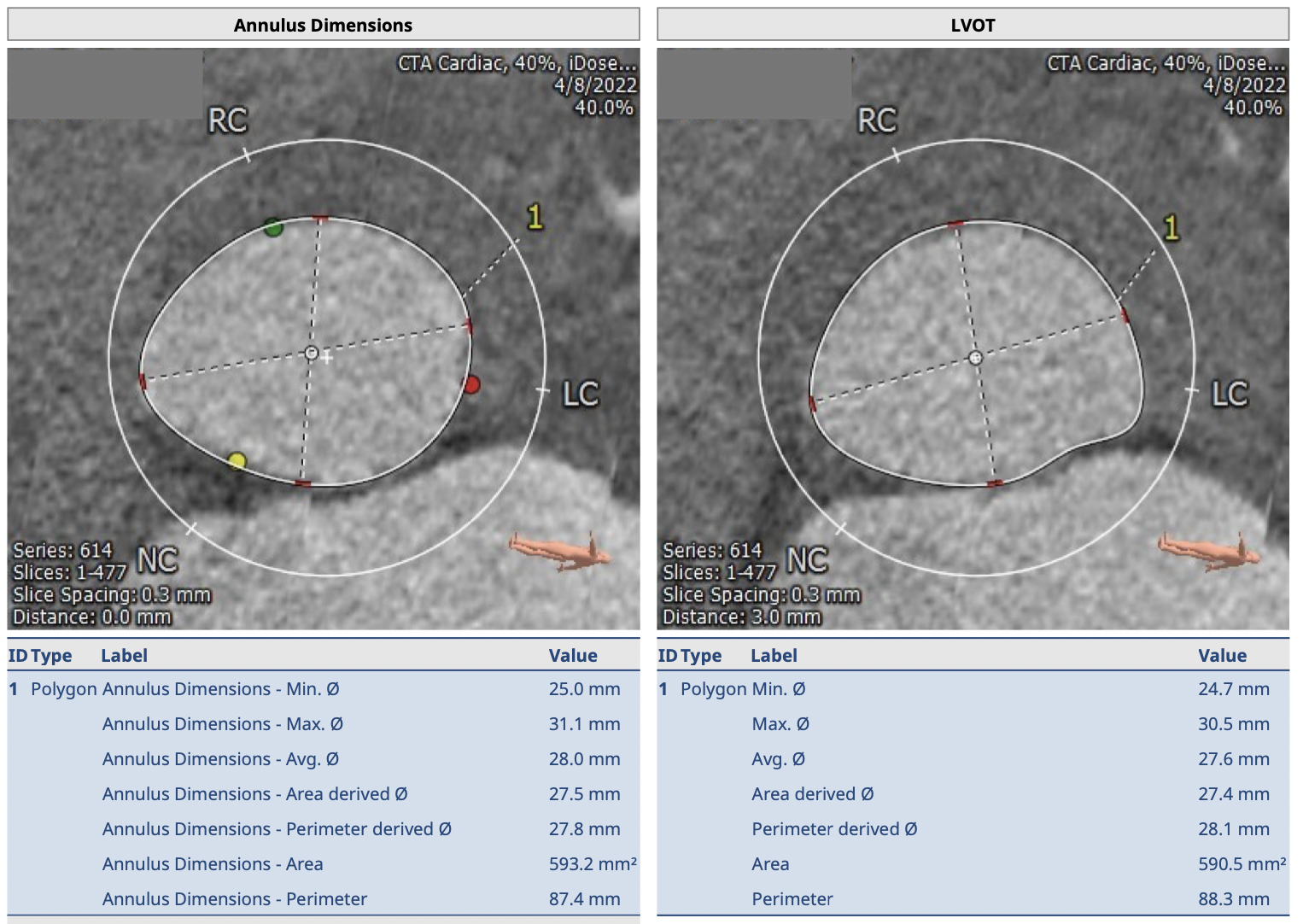
The pre-procedural CT scan confirmed a non-calcified aortic valve. At phase 40 %, the annulus area is 593.2 mm2, mean diameter is 28 mm. The LVOT area is 590.5 mm2, mean diameter is 27.6 mm. SOV diameters are 40.7 mm(RCC) x 40.2 mm(LCC) x 42.2 mm (NCC) . STJ diameters are 36.8 x 38.3 mm and the height is 27.2 mm. The co-planar view is LAO 17 and caudal 31 degree. The left and right coronary heights are 15.9 mm and 23.4 mm. The aorta and its branches are large enough for accommodation with 16F.
Interventional Management
Procedural Step
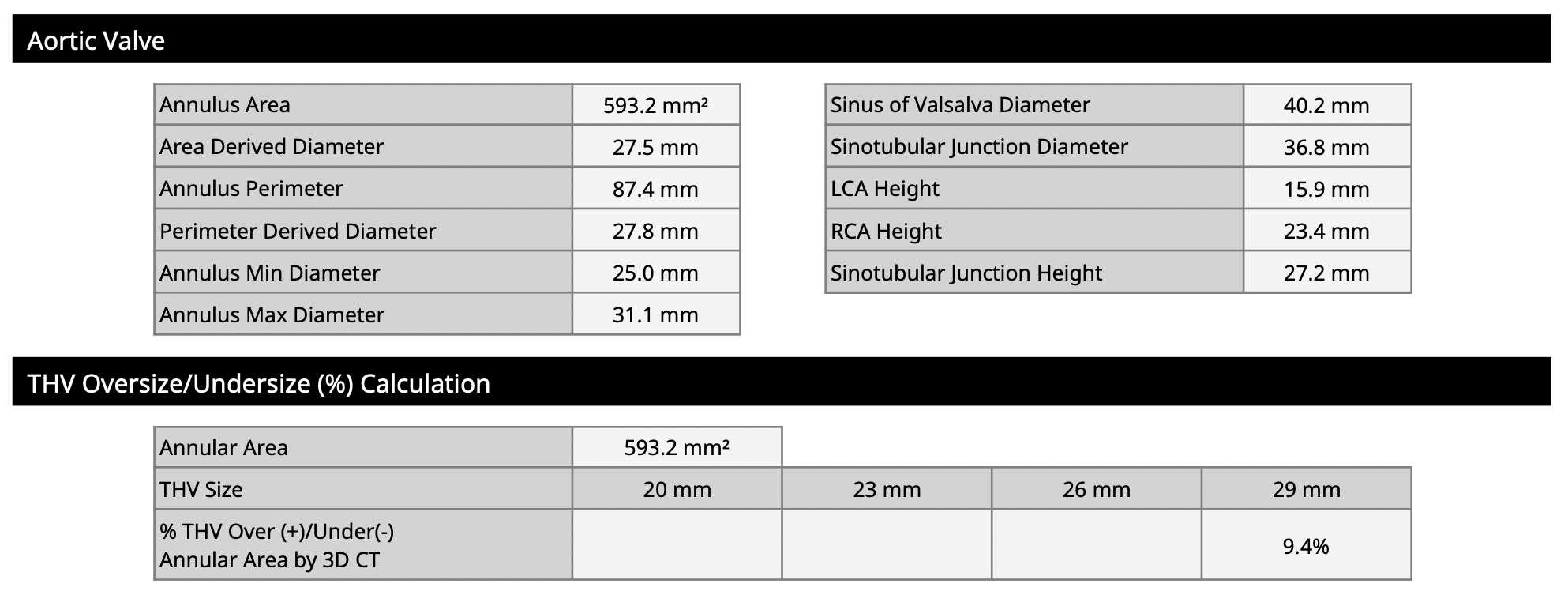
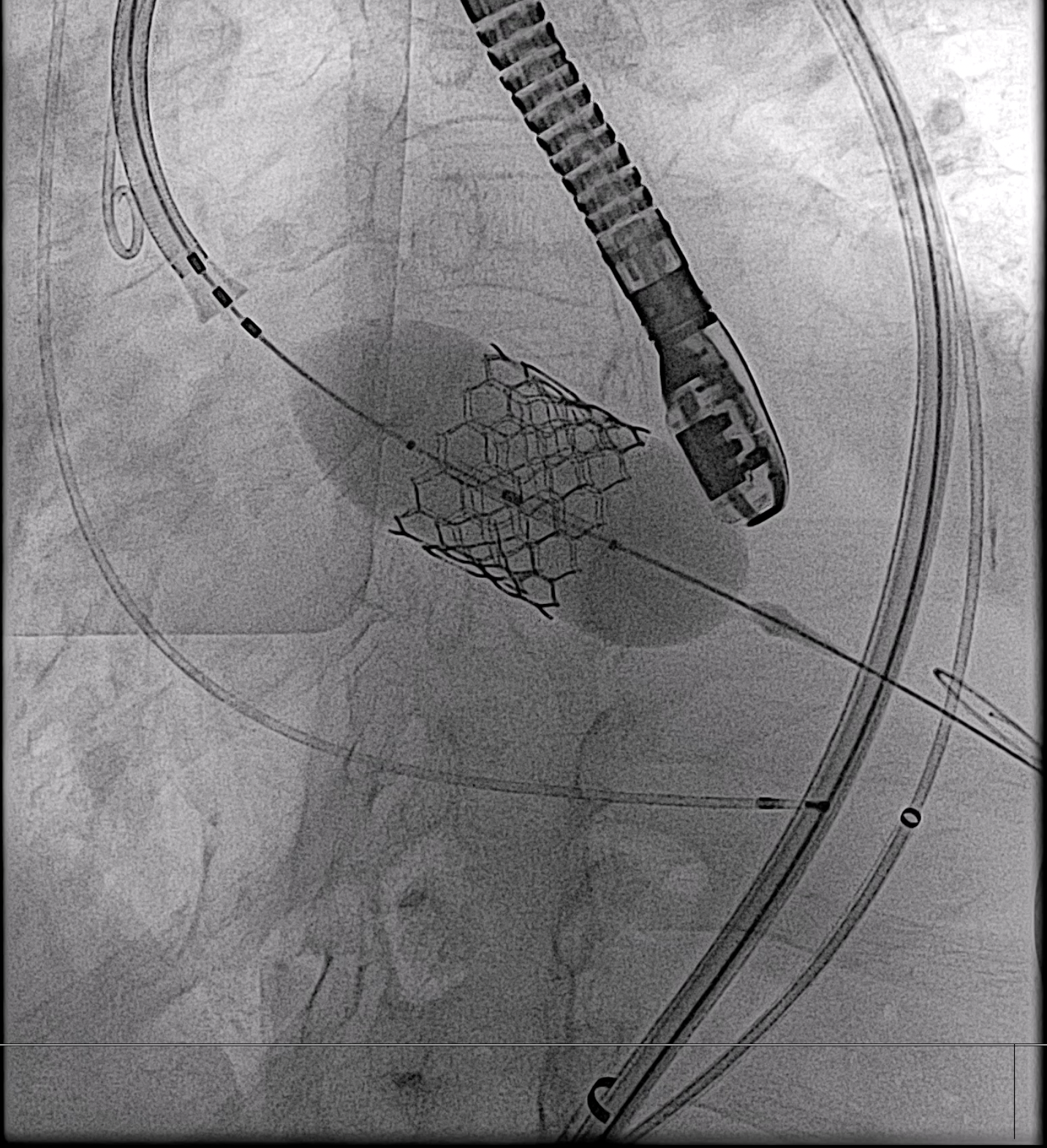
Right femoral access was obtained and pre-closure with two Progilde vascular closure devices was done, and 16F Edward E sheath was placed in the aorta. Left femoral access with a 6F long sheath due to vessel tortuosity was done. Two 5F pigtails were placed as markers at the right and non-coronary cusps, after that aortogram was done at the deployment angle. A pigtail was used to cross the aortic valve to LV and extra-small Safari wire was placed in LV in standard fashion. An Edwards commander delivery system was passed along the Safari wire and prepared as a standard technique before crossing the aortic arch and aortic valve subsequently. The ECG showed a complete heart block after the Sapien S3 size 29 mm passed into LVOT, then the temporary pacemaker was inserted via the right jugular vein to the right ventricle. The final position was aimed during rapid percutaneous pacing and aortogram, S3 was then deployed at +3 ml for 19.7 % oversizing. Initially, the immediate aortogram and TEE showed only mild paravalvular leak(PVL), however, there was a progression of PVL 15 minutes later. The valve embolization was suspected and the valve was unstable, therefore we decided to deploy the second S3 29 mm at +4 ml above the first valve. The final aortogram and TEE showed a reduction of PVL and no new pericardial effusion. The mean pressure gradient across the aortic valve was 5 mmHg.

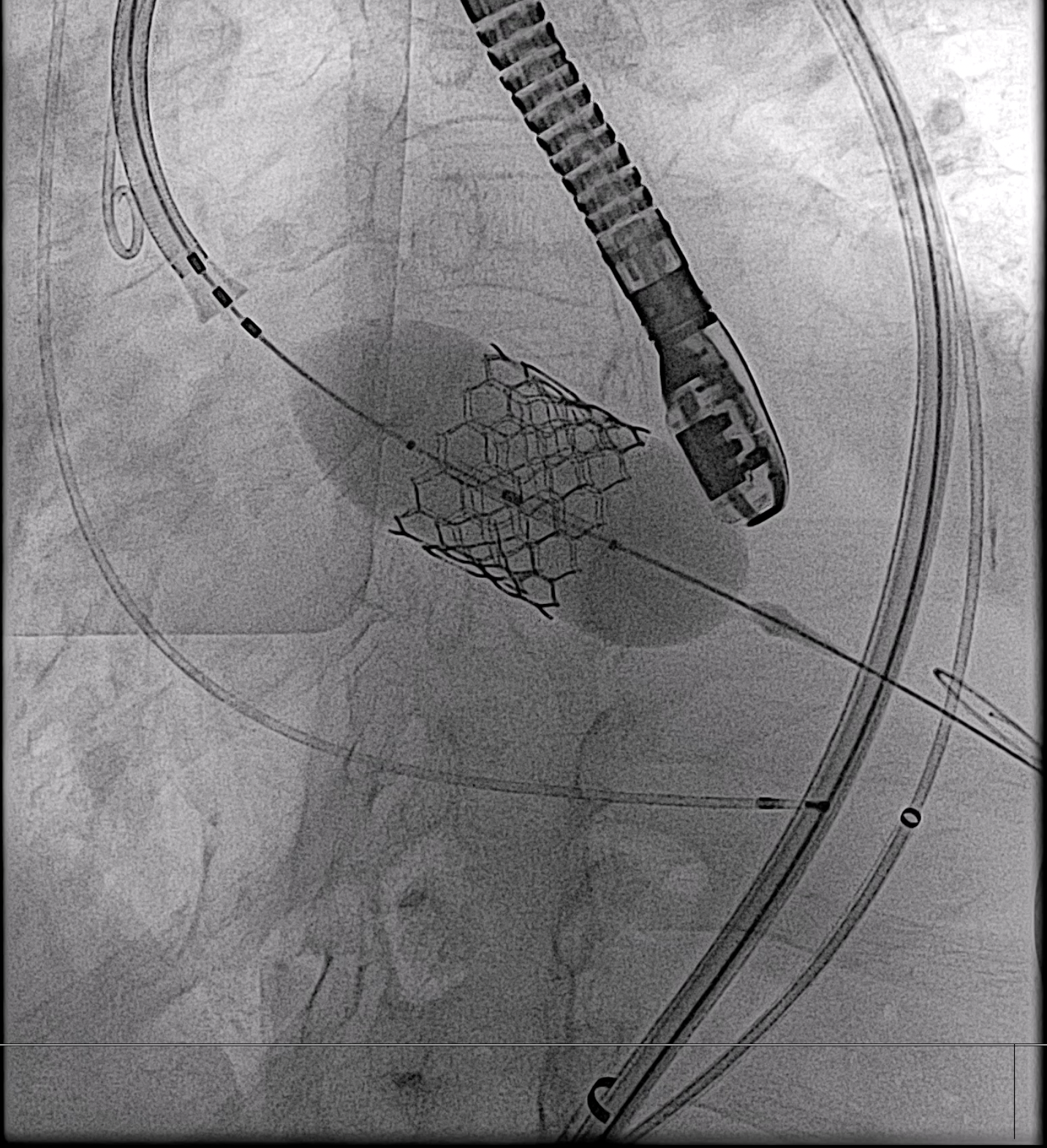

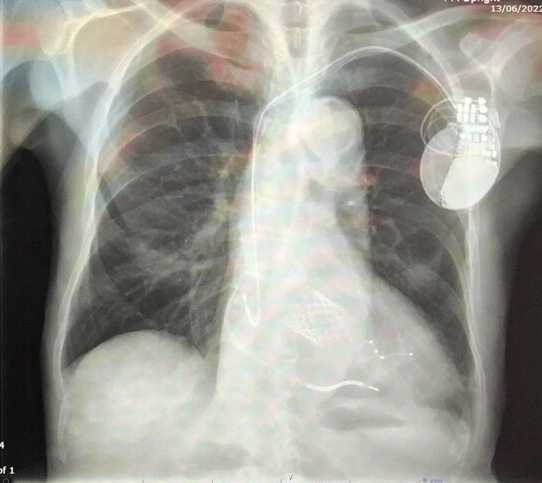
Case Summary
He developed a complete heart block one day after an intervention and was implanted with a CRT-D. He was discharged home after 5 days, with their symptoms dramatically subsiding and a return to normal daily life within a month. Follow-up echocardiography revealed transient deterioration of LV function in the first two weeks, but gradual improvement to normal systolic function within 3 months. The TAVI valves were well-seated with a mean pressure gradient across TAVI of 6 mmHg and functional MR had disappeared completely. This case suggests that the precise diagnosis of the cause of heart failure is crucial and that TAVI is a feasible treatment option with caution.


