Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP C-153
Transradial and Transfemoral Approach in a Case of Brachiocephalic Arteriovenous Fistuloplasty
By Yuen Han Lim, Mohamed Nazrul Mohamed Nazeeb, Yee Sin Tey, Jayakhanthan Kolanthaivelu
Presenter
Yuen Han Lim
Authors
Yuen Han Lim1, Mohamed Nazrul Mohamed Nazeeb1, Yee Sin Tey1, Jayakhanthan Kolanthaivelu2
Affiliation
National Heart Institute, Malaysia1, Cardiovascular Sentral Kuala Lumpur, Malaysia2,
View Study Report
TCTAP C-153
ENDOVASCULAR - Peripheral Vascular Disease and Intervention
Transradial and Transfemoral Approach in a Case of Brachiocephalic Arteriovenous Fistuloplasty
Yuen Han Lim1, Mohamed Nazrul Mohamed Nazeeb1, Yee Sin Tey1, Jayakhanthan Kolanthaivelu2
National Heart Institute, Malaysia1, Cardiovascular Sentral Kuala Lumpur, Malaysia2,
Clinical Information
Patient initials or Identifier Number
ZM
Relevant Clinical History and Physical Exam
Mr. ZM is a 70 years old gentleman with coronary artery disease (Left Main Stem-Left Anterior Descending intervention in September 2022) and end stage renal disease on regular haemodialysis via left brachiocephalic arteriovenous fistula (BCF) since 2017. He underwent fistuloplasty with drug coated balloon to the left cephalic vein in July 2022. Unfortunately, his BCF was blocked again in October 2022. There was swelling with absent thrill. Blood pressure was 125/86 mmHg, heart rate 67 bpm.
Relevant Test Results Prior to Catheterization
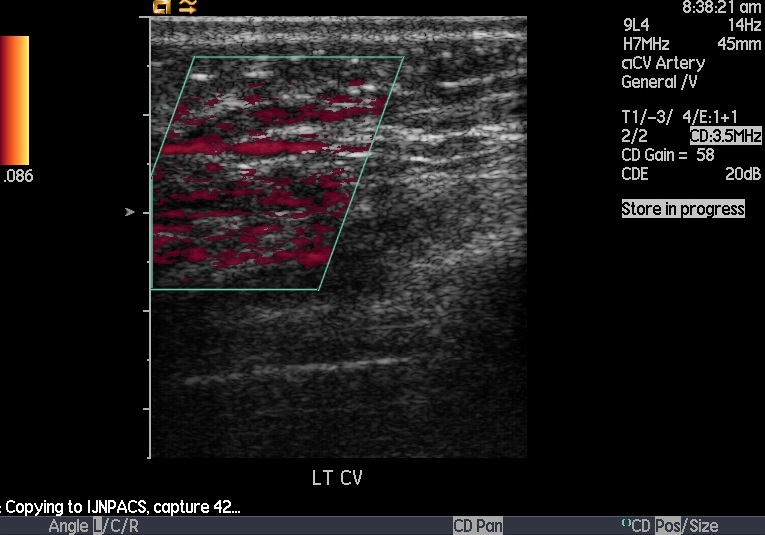
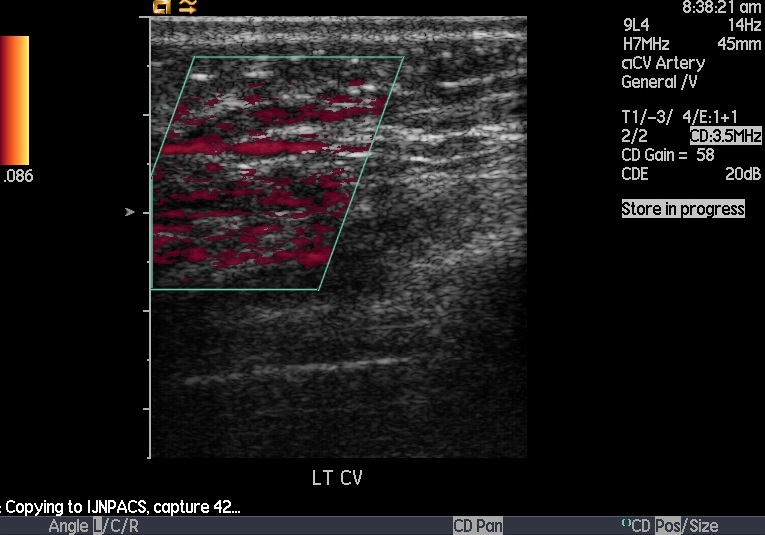
Duplex Doppler ultrasonography of left upper limb showed anastomosis size of 0.6 cm, peak systolic velocity 190 - 209 cm/sec. Thrombus was seen at the first aneurysm sac with minimal flow noted. Peak velocity at the first juxta was 525 - 552 cm/sec. Thrombus seen at the second aneurysm sac with no flow seen. There was total occlusion of cephalic vein. Patent venous flow was seen at the subclavian and axillary veins.




Relevant Catheterization Findings
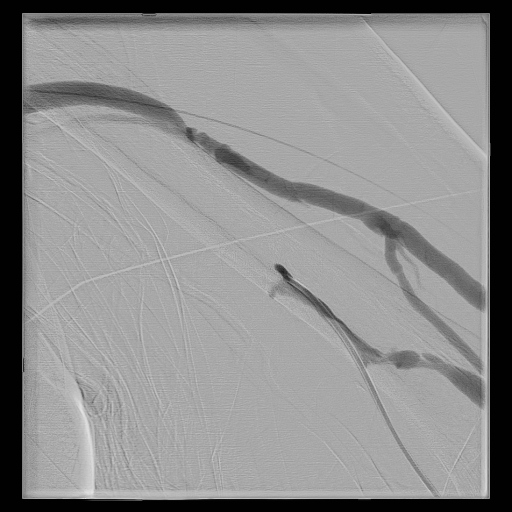
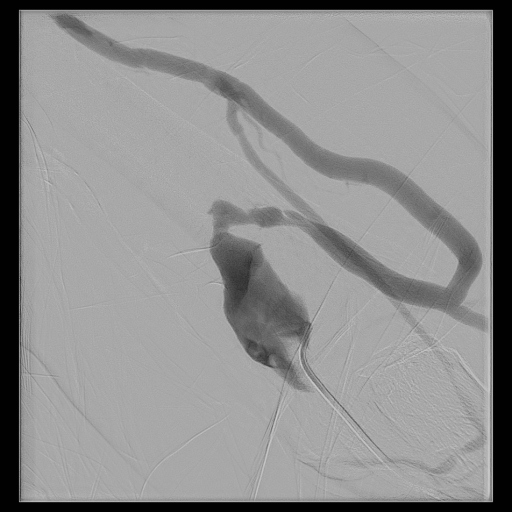
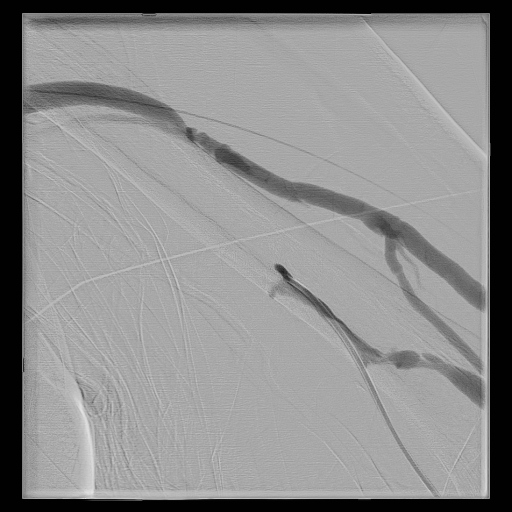
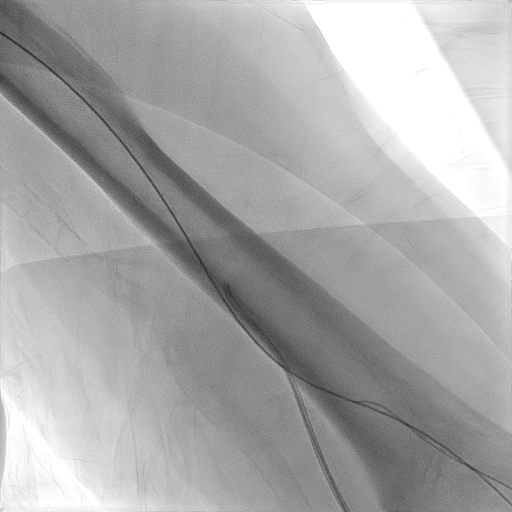
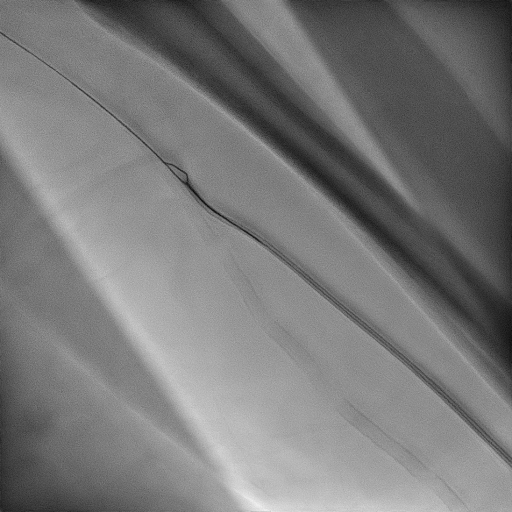
Left brachiocephalic fistulogram and central venogram showed total occlusion of cephalic vein. Thrombus was seen in the aneurysm sac. The arteriovenous anastomotic site, subclavian vein and axillary vein were patent.
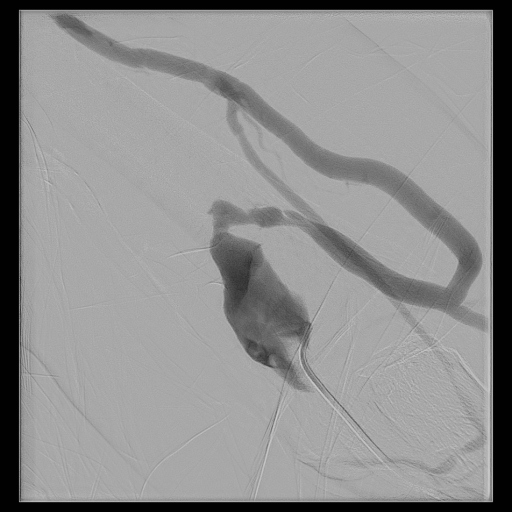
 Video A - Fistulogram.mpg
Video A - Fistulogram.mpg
Interventional Management
Procedural Step
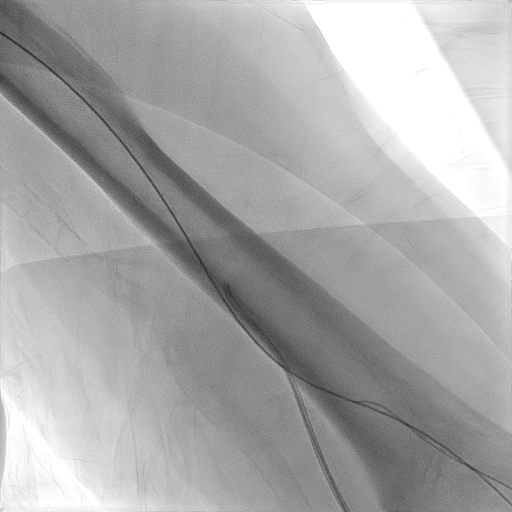
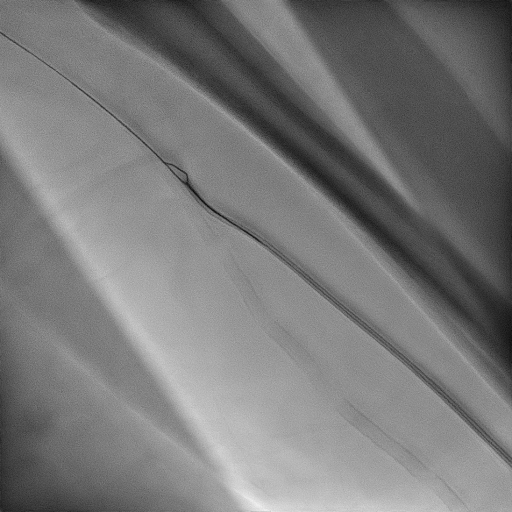
Left radial artery was cannulated with a 4-Fr micropuncture needle followed by insertion of a 5-Fr Glidesheath Slender (Terumo, Tokyo, Japan). 2000 IU heparin and 100 mcg nitroglycerin were administered through the radial sheath to prevent radial artery spasm and thrombus formation. JR3.5/5 Fr catheter and Stiff Glidewire (Terumo, Japan) were advanced past the arteriovenous anastomosis and aneurysm sac but failed to cross the cephalic vein total occlusion antegradely. Following that, left femoral vein was punctured with ultrasound guidance and 6-Fr Terumo Sheath was inserted for retrograde access. Terumo Stiff wire and 6-Fr MPA Catheter 100cm (Medtronic, USA) were advanced from left femoral vein up to the central vein and crossed the left cephalic vein lesion with ease. Terumo stiff wire was then exchanged to V-18 Control Wire 0.018 in x 300 cm (Boston Scientific, MA, USA). In order to proceed with transradial approach, ONE Snare System 4 Fr (Merit Medical, USA) was advanced via the radial sheath then snared the V-18 Wire out of the radial sheath. Over the V-18 wire, the 5-Fr Glidesheath was exchanged to 6-Fr Terumo sheath. Subsequently, sequential plain balloon dilatation of the left cephalic vein was done with Armada 35 4.0 mm x 40 mm x 135 cm (Abbott, USA) up to 16 atm for 10 seconds, Armada 35 LL 5.0 mm x 200mm x 135 cm up to 8 atm for 70 seconds, and finally Armada 35 6.0 mm x 80 mm x 135 cm up to 6 atm for 100 seconds. Post procedure, radial artery was compressed with Nichiban dressing.
Case Summary
Venous antegrade or retrograde puncture of the fistula is a commonly used access for fistuloplasty. However, it has limitation in treating juxta-anastomotic lesions, lesions downstream from the puncture site, and multiple lesions. We prefer antegrade radial approach as it allows assessment and intervention of the entire fistula up to the central vein, including arterial inflow and venous outflow, with a single puncture and sheath. It is also safe and more comfortable for the patients. Femoral approach is another alternative in difficult radial access due to small diameter or spasm. In this case, the femoral approach allowed successful retrograde crossing of the cephalic vein occlusion.


