Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-090
Investigation of Strategies to Reduce Contrast Media Usage and Risk of Contrast Induced Renal Injury During PCI: A “Low Contrast Volume Protocol” Introduction to a Daily Clinical Practice
By Aiste Zebrauskaite, Greta Ziubryte, Lukas Mackus, Austeja Lieponyte, Evelina Kairyte, Gediminas Jarusevicius
Presenter
Aiste Zebrauskaite
Authors
Aiste Zebrauskaite1, Greta Ziubryte1, Lukas Mackus1, Austeja Lieponyte1, Evelina Kairyte1, Gediminas Jarusevicius2
Affiliation
Lithuanian University of Health Sciences, Lithuania1, Institute of Cardiology, Lithuanian University of Health Sciences, Lithuania2
View Study Report
TCTAP A-090
Renal Insufficiency and Contrast Nephropathy
Investigation of Strategies to Reduce Contrast Media Usage and Risk of Contrast Induced Renal Injury During PCI: A “Low Contrast Volume Protocol” Introduction to a Daily Clinical Practice
Aiste Zebrauskaite1, Greta Ziubryte1, Lukas Mackus1, Austeja Lieponyte1, Evelina Kairyte1, Gediminas Jarusevicius2
Lithuanian University of Health Sciences, Lithuania1, Institute of Cardiology, Lithuanian University of Health Sciences, Lithuania2
Background
Approximately 7% of patients undergoing percutaneous coronary intervention (PCI) experience contrast induced nephropathy (CIN).1 In patients with advanced kidney disease the incidence increases to around 30%1,2. CIN has been strongly associated with adverse clinical outcomes, including death, need for haemodialysis, increased hospital costs and lengths of stay.1-6 The ratio of the contrast media (CM) volume used to the creatinine clearance is one of the strongest predictors of development of CIN following PCI.7,8 Therefore, in order to reduce the incidence of CIN it is important to focus on strategies to reduce the volume of CM used particularly in those with chronic kidney disease (CKD).
Methods
A “Low Contrast Volume Protocol” was established in our catheterisation laboratory. It includes patient’s renal function described as a serum creatinine level in mkmol/l and calculated creatinine clearance (CrCl). CrCl was calculated with the Cockroft-Gault equation9. Based on the most relevant clinical data7-8 two contrast volume targets were calculated: the maximal recommended to use CV and a CV witch should strictly not be exceed. The maximal recommended to use CV was calculated according to the CrCl by the formula – CrCl X3.0 – it shows the amount of maximal recommended to use CV in mls and a CV witch should strictly not be exceed during the procedure is calculated by the formula CrCl X3.5 – it indicated the amount of the CV in mls witch is maximally allowed to use.
Results
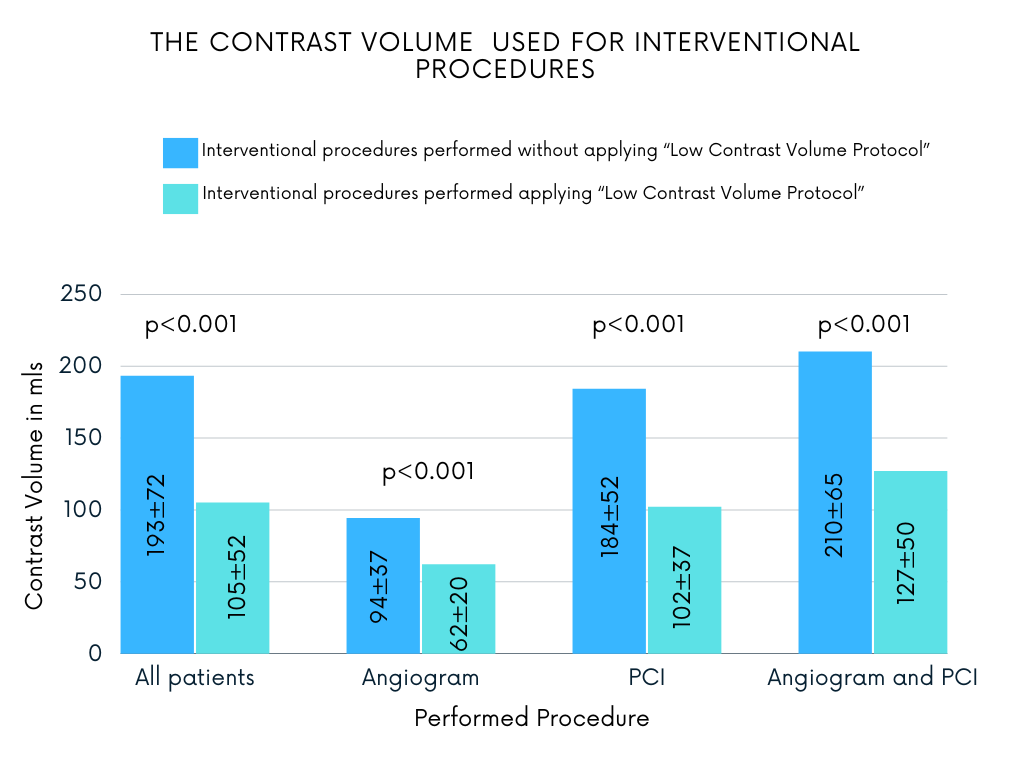
A total of 519 patients undergoing angiogram or PCI or angiogram followed by PCI on the same procedure were involved into the study.
For 312 patients interventional procedures were performed without applying “Low Contrast Volume Protocol”. The mean age was 71.0 ± 12.1 years. There were 67.3% male and 32.7% female patients. Comorbidities included as followed: AH (93.3%), Dyslipidaemia (91.7%) and CAD (97.1%). Nearly one fifth (18.3%) had DM and 21.8% had diagnosed CKD. For 12.8% of patients diagnostic angiogram was performed, 10.0% underwent scheduled PCI, the majority of patients 77.2%.For 207 patients the “Love Contrast Volume Protocol” was applied, maximal recommended CV amounts were personally calculated based on their kidney function, contrast dosing was actively monitored during the procedure. The mean patient age was 68.2 ± 11.0 years. There were 58.5% male and 41.5% female patients. Comorbidities included: AH (96.1%), Dyslipidaemia (88.9%) and CAD (99.5%). Nearly one fifth (19.8%) had DM and 19.3% had diagnosed CKD. For 29.0% of patients diagnostic angiogram was performed, 14.5% underwent scheduled PCI, 56.5% underwent angiogram and PCI.
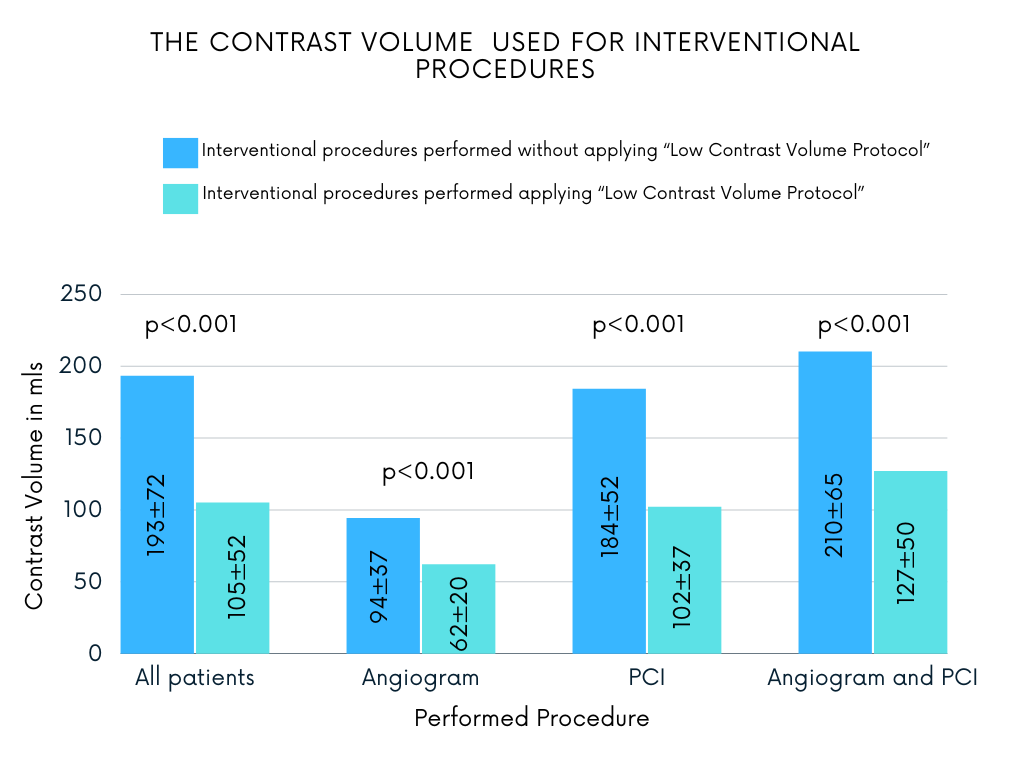
For 312 patients interventional procedures were performed without applying “Low Contrast Volume Protocol”. The mean age was 71.0 ± 12.1 years. There were 67.3% male and 32.7% female patients. Comorbidities included as followed: AH (93.3%), Dyslipidaemia (91.7%) and CAD (97.1%). Nearly one fifth (18.3%) had DM and 21.8% had diagnosed CKD. For 12.8% of patients diagnostic angiogram was performed, 10.0% underwent scheduled PCI, the majority of patients 77.2%.For 207 patients the “Love Contrast Volume Protocol” was applied, maximal recommended CV amounts were personally calculated based on their kidney function, contrast dosing was actively monitored during the procedure. The mean patient age was 68.2 ± 11.0 years. There were 58.5% male and 41.5% female patients. Comorbidities included: AH (96.1%), Dyslipidaemia (88.9%) and CAD (99.5%). Nearly one fifth (19.8%) had DM and 19.3% had diagnosed CKD. For 29.0% of patients diagnostic angiogram was performed, 14.5% underwent scheduled PCI, 56.5% underwent angiogram and PCI.
Conclusion
Our applied personalised maximal recommended to use CM volume calculation leads to significant reduction in contrast volume usage and risk reduction of contrast induced kidney injury development.


