Lots of interesting abstracts and cases were submitted for TCTAP 2023. Below are the accepted ones after a thorough review by our official reviewers. Don’t miss the opportunity to expand your knowledge and interact with authors as well as virtual participants by sharing your opinion in the comment section!
TCTAP A-093
Pre-Procedural Ultrasound in Palpation Versus Ultrasound Guided Radial Access for Cardiac Catheterization
By Bryan Rene Toledano, Kristy Garganera, Jose Paolo Alto Prado, Michelangelo L. Sabas
Presenter
Bryan Rene Toledano
Authors
Bryan Rene Toledano1, Kristy Garganera1, Jose Paolo Alto Prado1, Michelangelo L. Sabas1
Affiliation
The Medical City, Philippines1
View Study Report
TCTAP A-093
Vascular Access (Transradial)
Pre-Procedural Ultrasound in Palpation Versus Ultrasound Guided Radial Access for Cardiac Catheterization
Bryan Rene Toledano1, Kristy Garganera1, Jose Paolo Alto Prado1, Michelangelo L. Sabas1
The Medical City, Philippines1
Background
In most laboratories, the radial first approach has become the preferred vascular access for cardiac catheterization procedures. It is associated with better patient comfort, early ambulation, and overall clinical benefit. The challenges encountered during cannulation include a small, deep, calcified, and mobile radial artery (RA). The valuable information provided by an ultrasonographic study, done before and during the procedure, can be used to increase the chance of success. Currently, there are no clear recommendations, and the utility of routine pre-procedural and procedural ultrasound (US) of the RA remains underused, understudied, and controversial. This study aims to employ a routine pre-procedural US and to evaluate the utility of procedural US over palpation guidance.
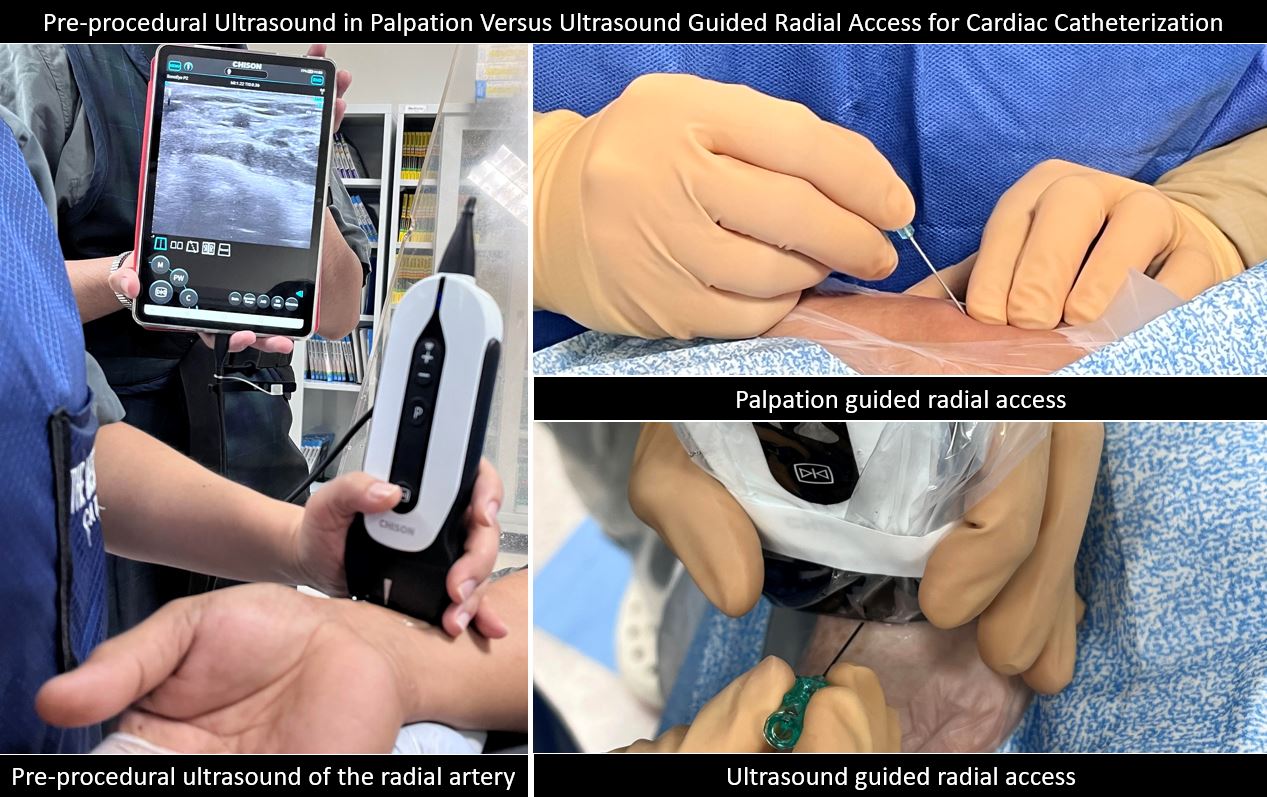
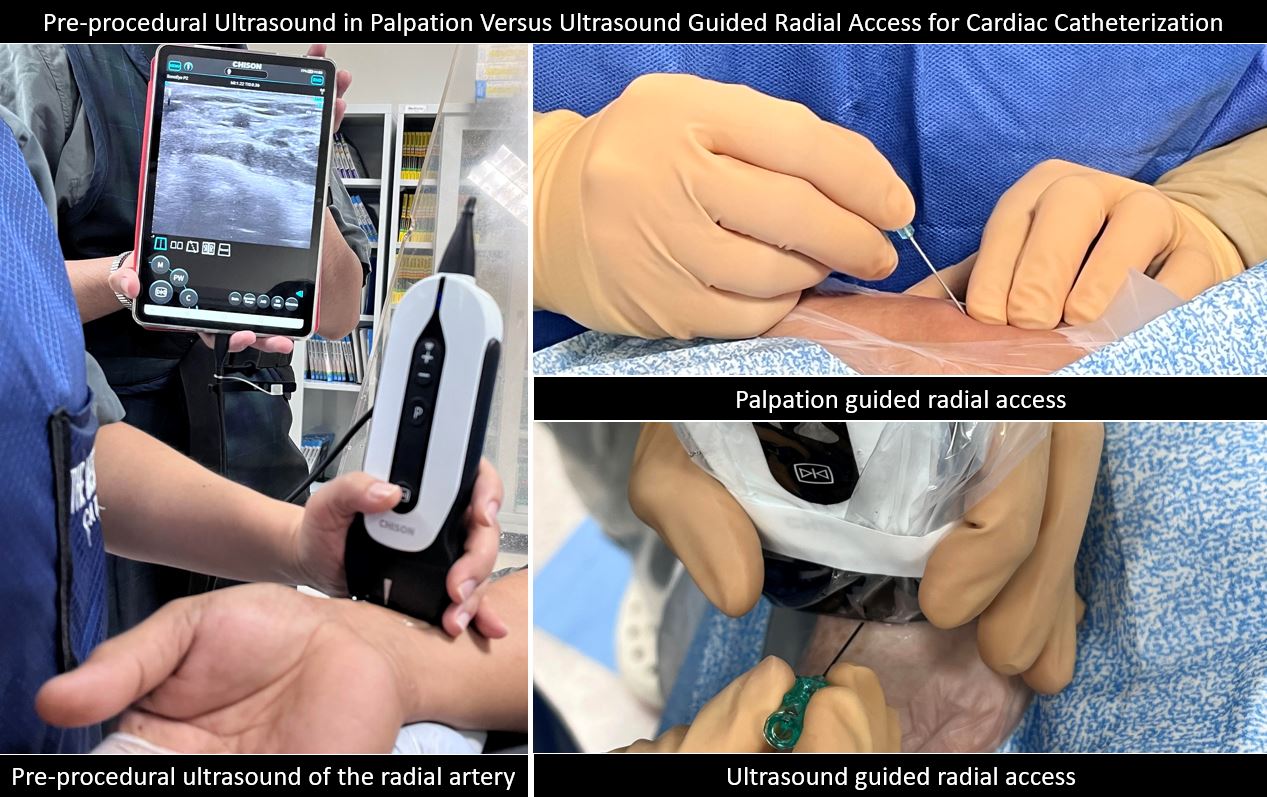
Methods
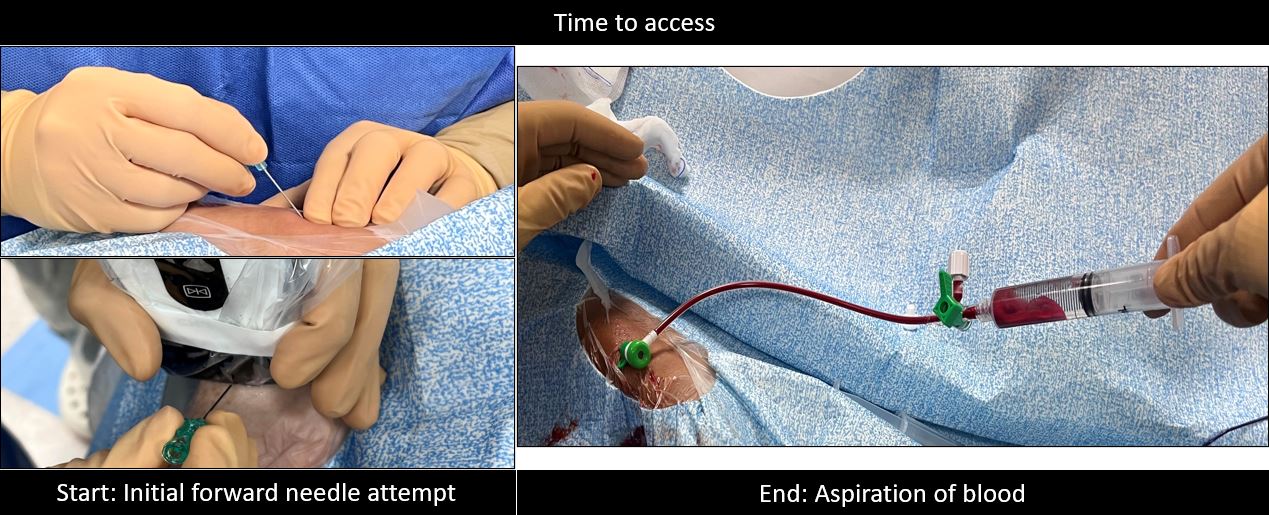
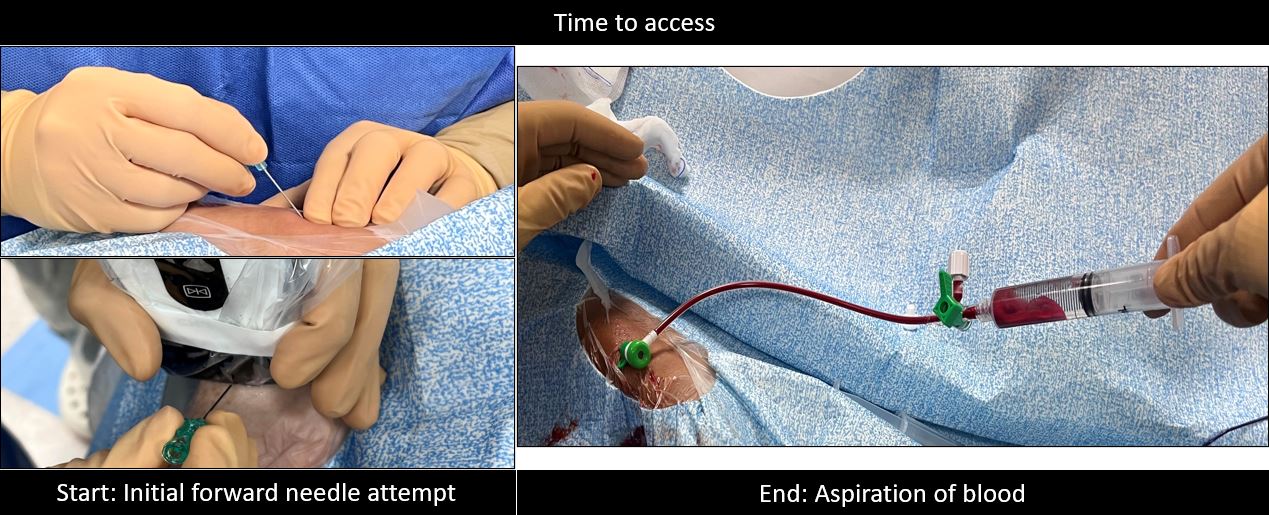
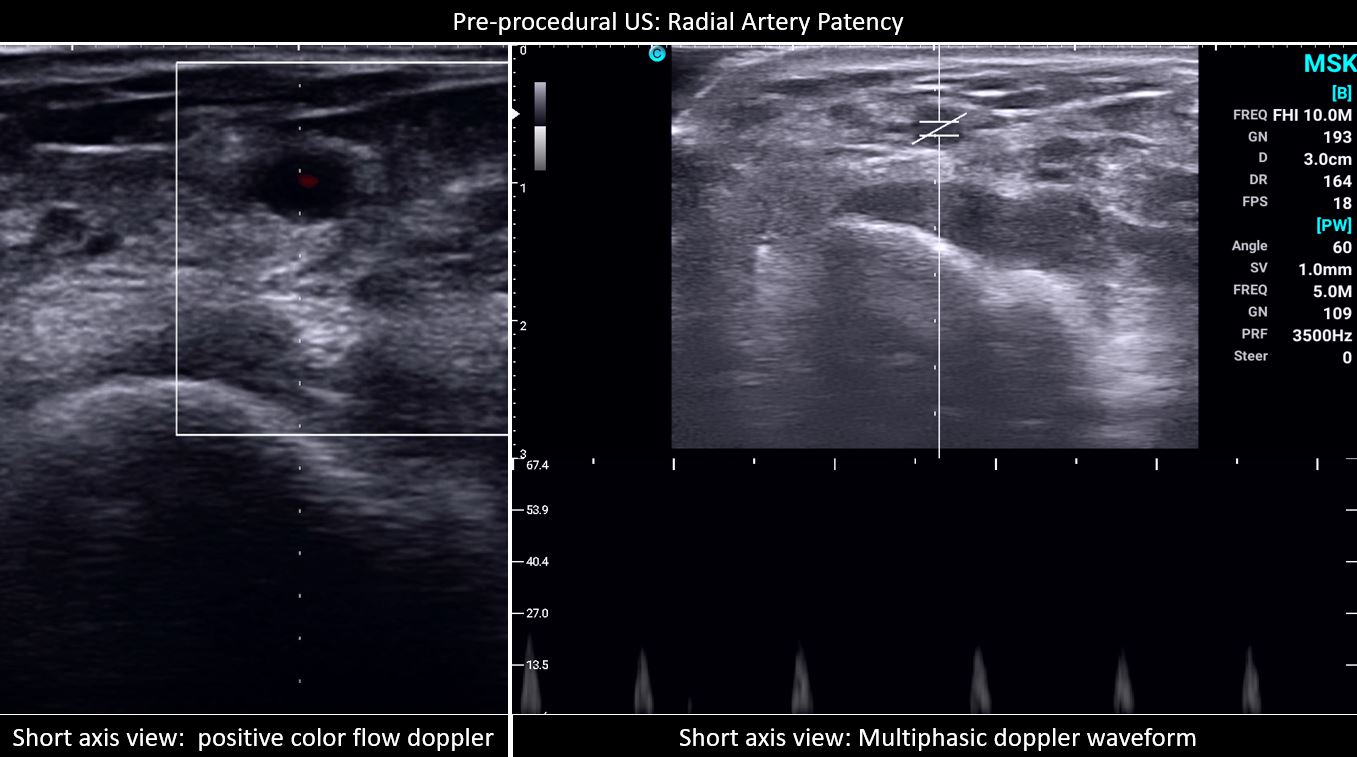
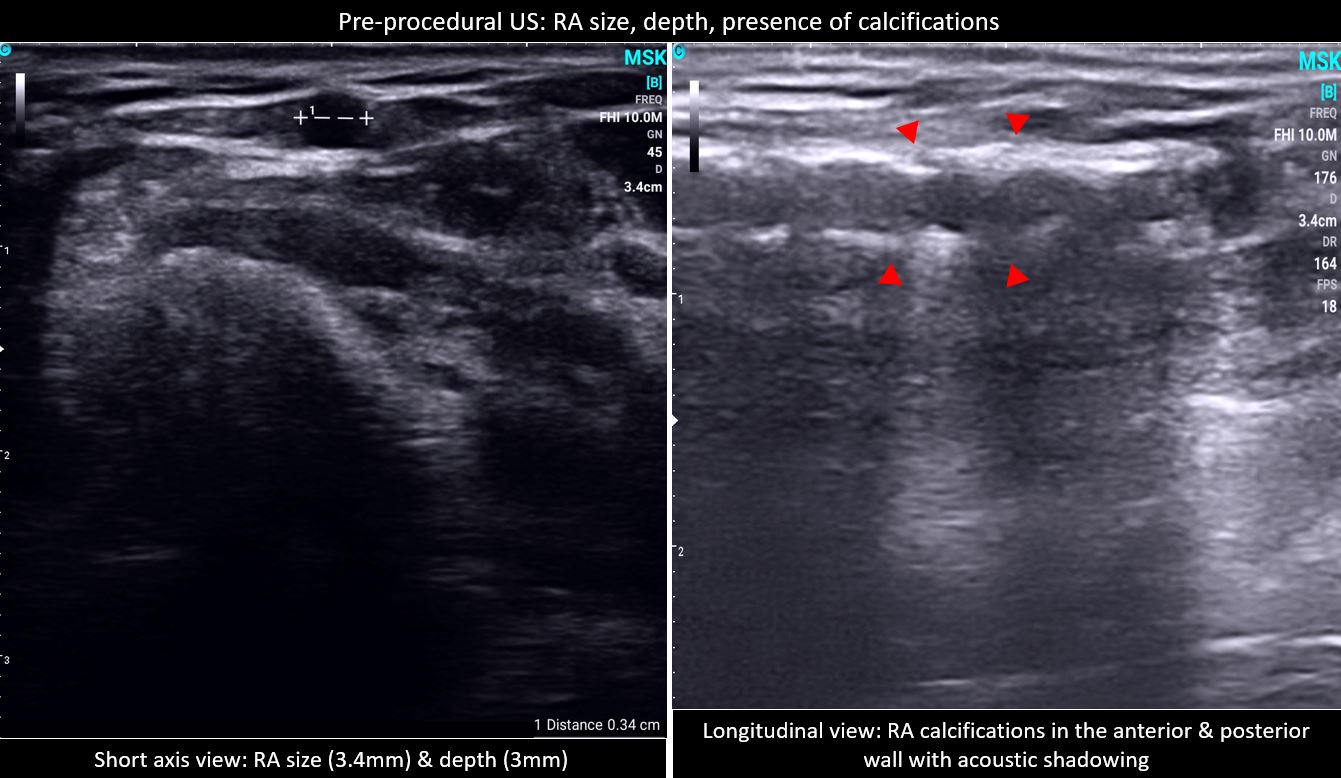
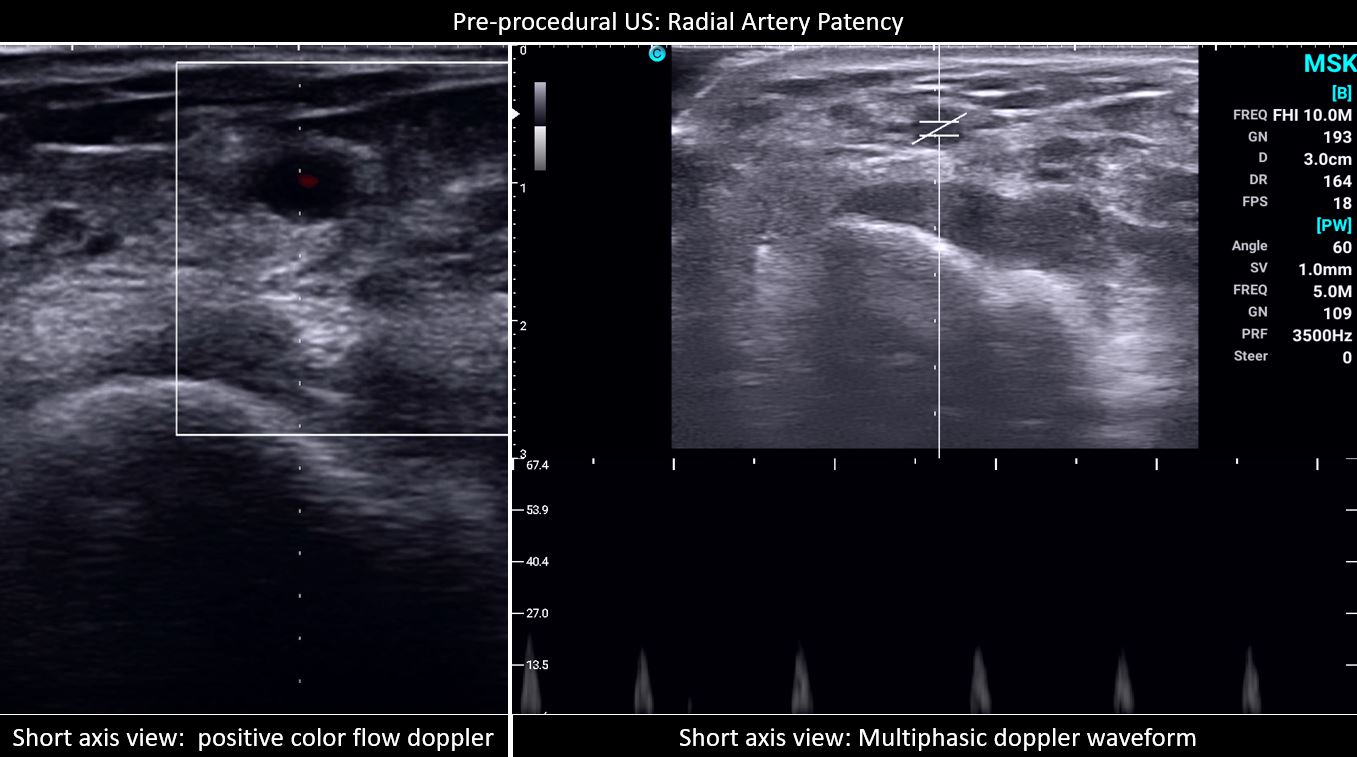
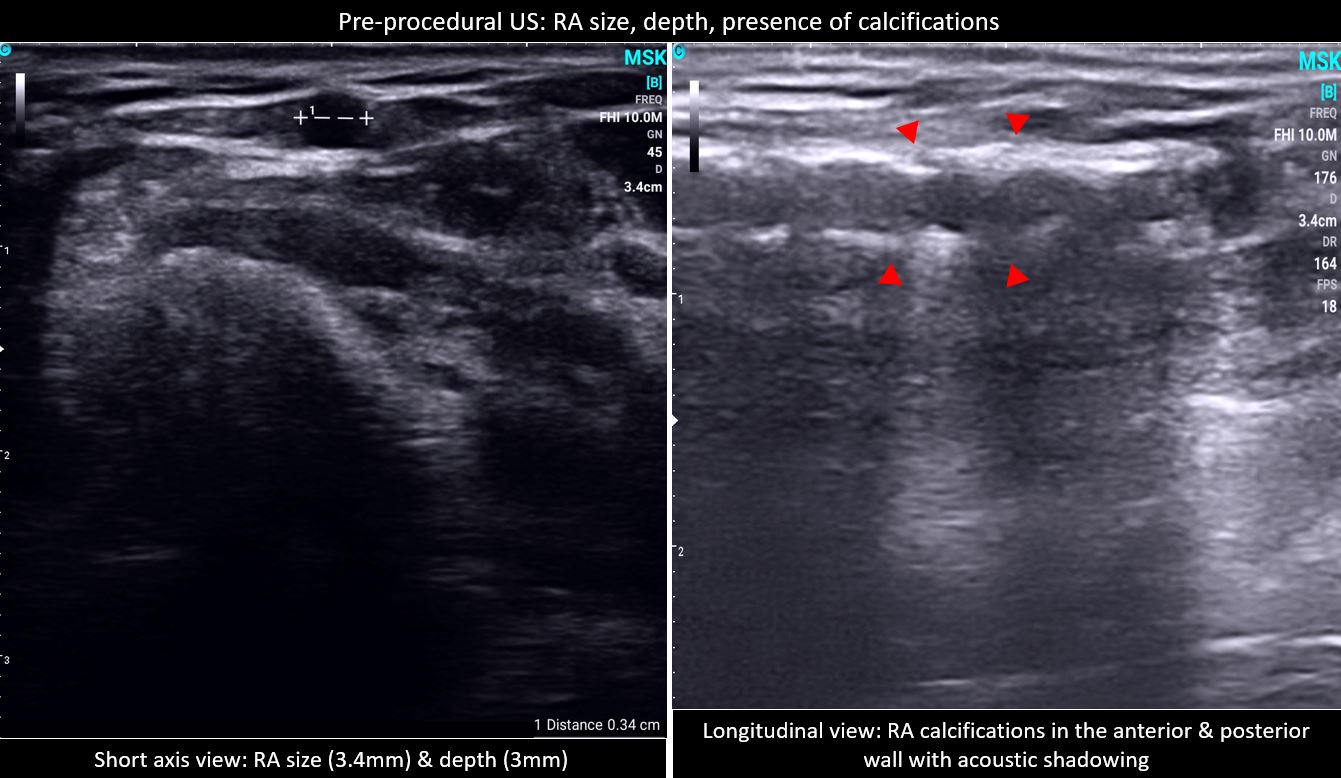
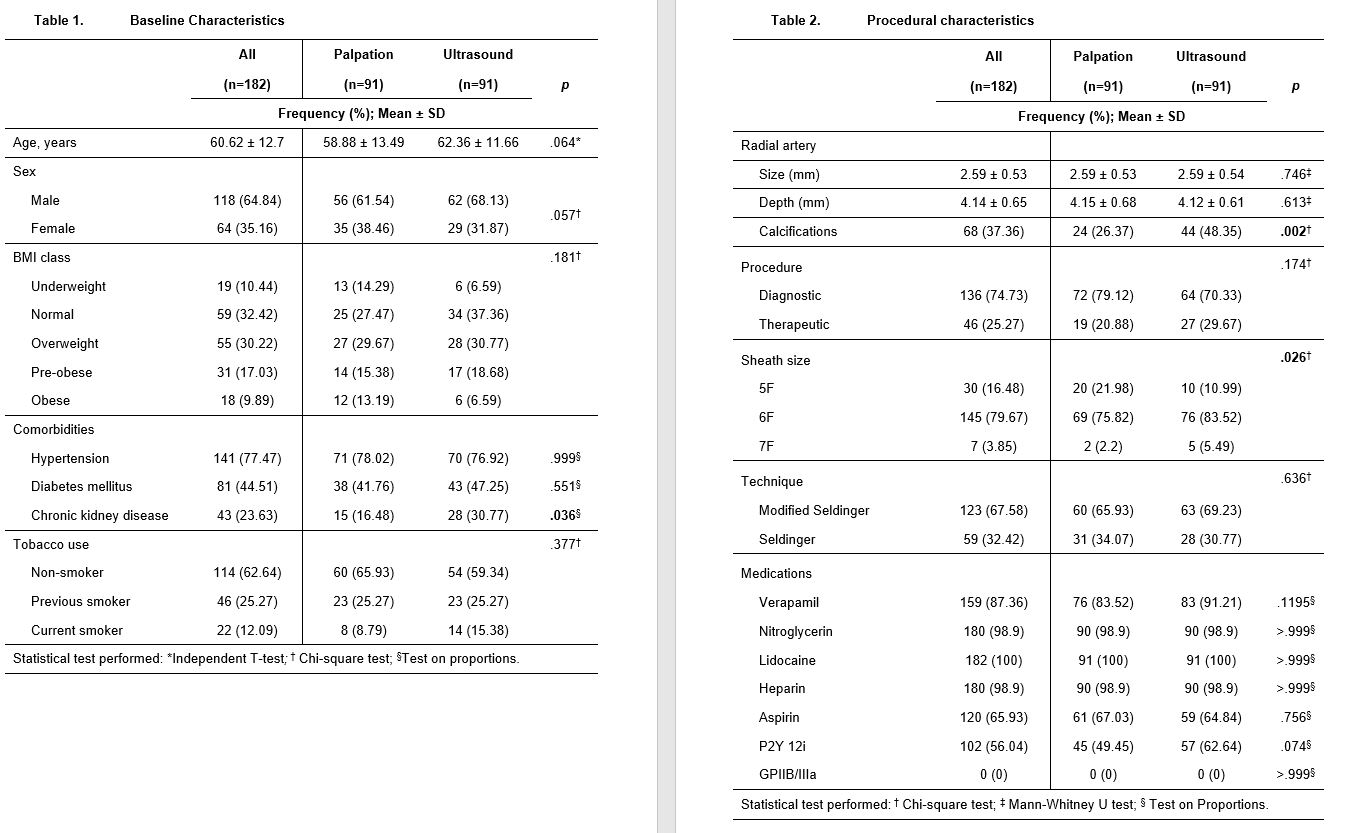
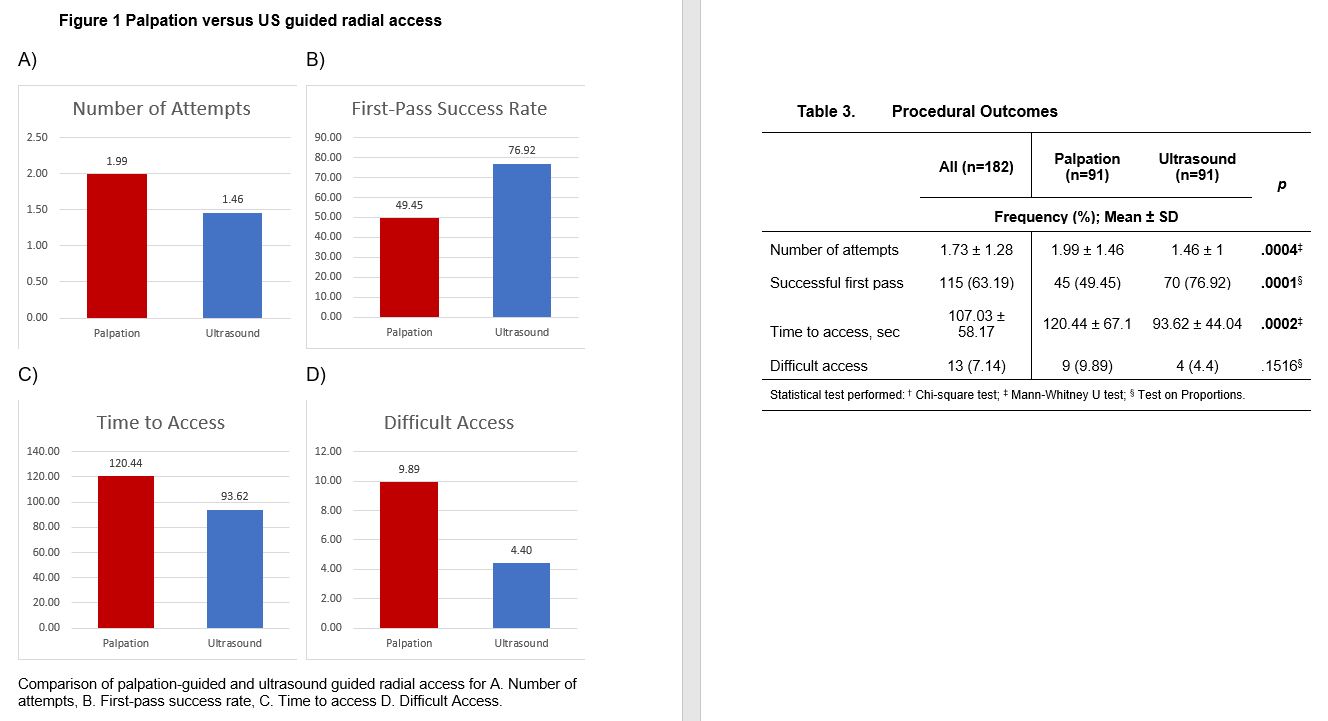
This is an investigator-initiated, prospective, single-center study. Consecutive consenting adult patients scheduled for elective radial cardiac catheterization procedures were included. A handheld probe with a 40mm linear array and 7-12 MHz transducer (CHISON Medical Technologies Co. Ltd) connected to a tablet was used. A sample size of at least 180 patients, 90 in each group was derived from 340 which is the laboratory’s quarterly average number of cardiac catheterization procedures, at a 5% level of significance and 95% power. The grouping was based on the attending interventional cardiologist/operator preference and experience. In both groups, the operators had performed a minimum of 100 palpation-guided and additional 15 US-guided successful RA catheterization procedures for the US group. Eight interventional cardiology consultants and two advanced interventional fellows participated in the study. In the pre-procedural US of the proximal RA, the patency, size, depth, and presence of calcifications were identified. All procedures were performed according to local standards and operator preference except for the mode of radial access. Baseline patient demographics and comorbidities were recorded via interview. Procedural details including the number of attempts, time to access, medications, sheath size, type of procedure, access technique, and any access site crossovers or rescue to ultrasound were tracked by the operator, first assistant, and circulating nurse. Screening for vascular complications such as spasms, pain, or bleeding, was done during and after the removal of the tourniquet band. The characteristics of the patients were summarized and tabulated using mean and standard deviation for quantitative and frequency and proportion for qualitative variables. Comparison between groups was done using Independent T-test for normal, Mann-Whitney U test for non-normal, Chi-Square for categorical, and a test on proportions for binary data. All p-values less than 0.05 were considered statistically significant and computed using Microsoft Office Excel 2016 and MedCalc v12.5 for forest plots.
Results
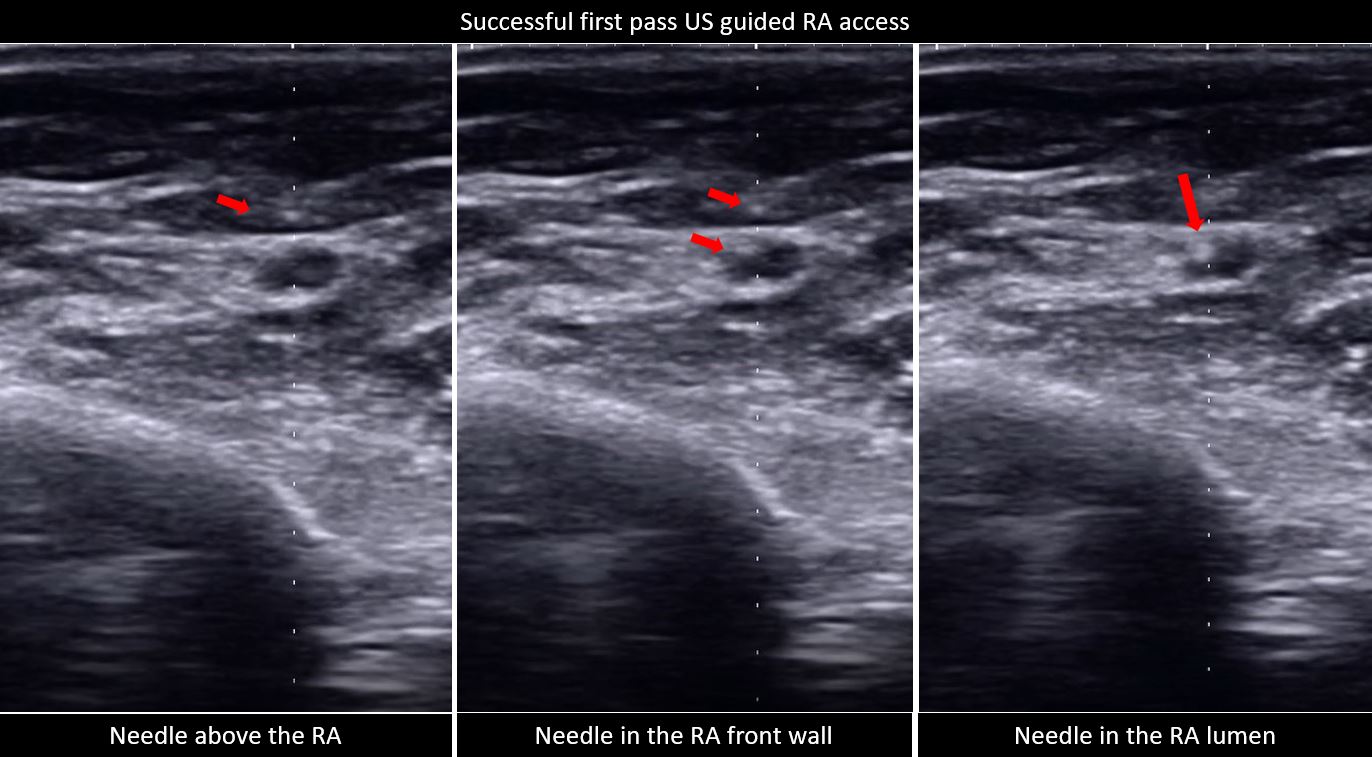
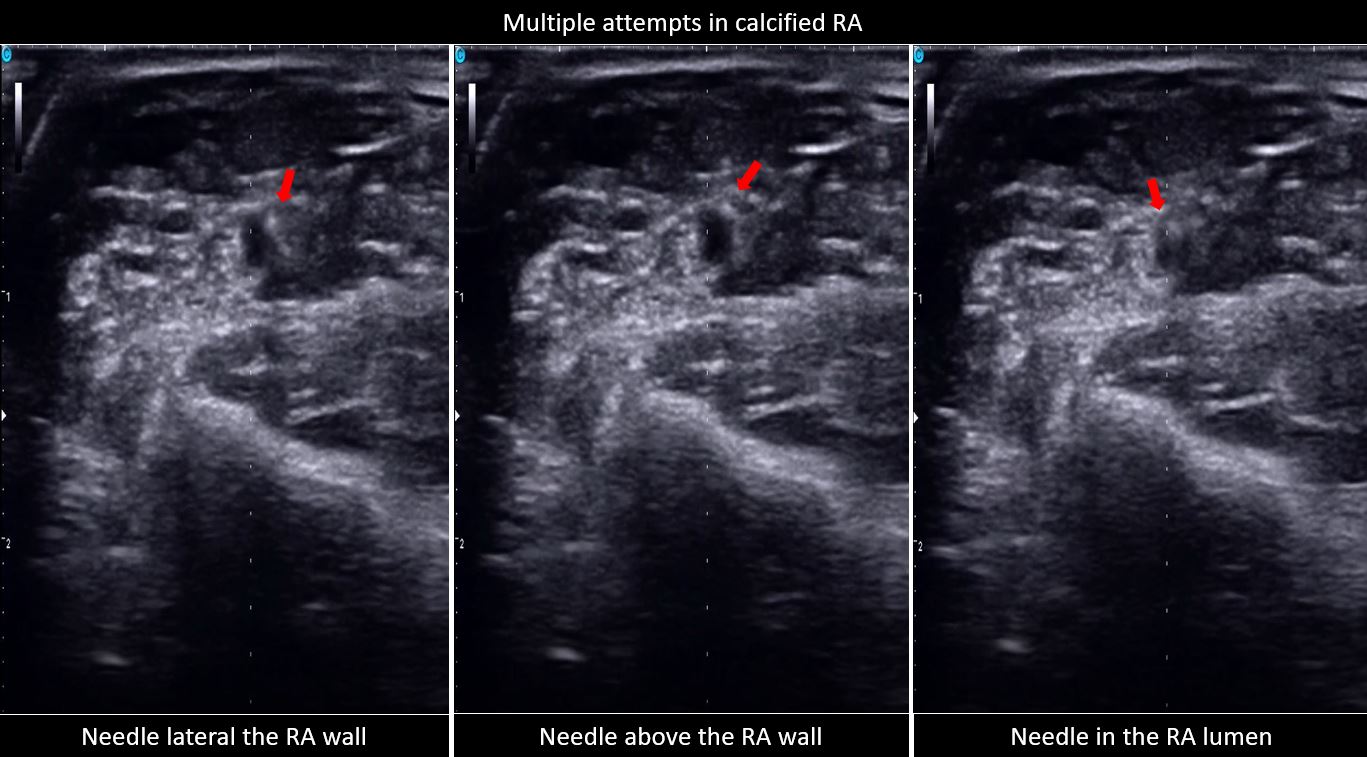
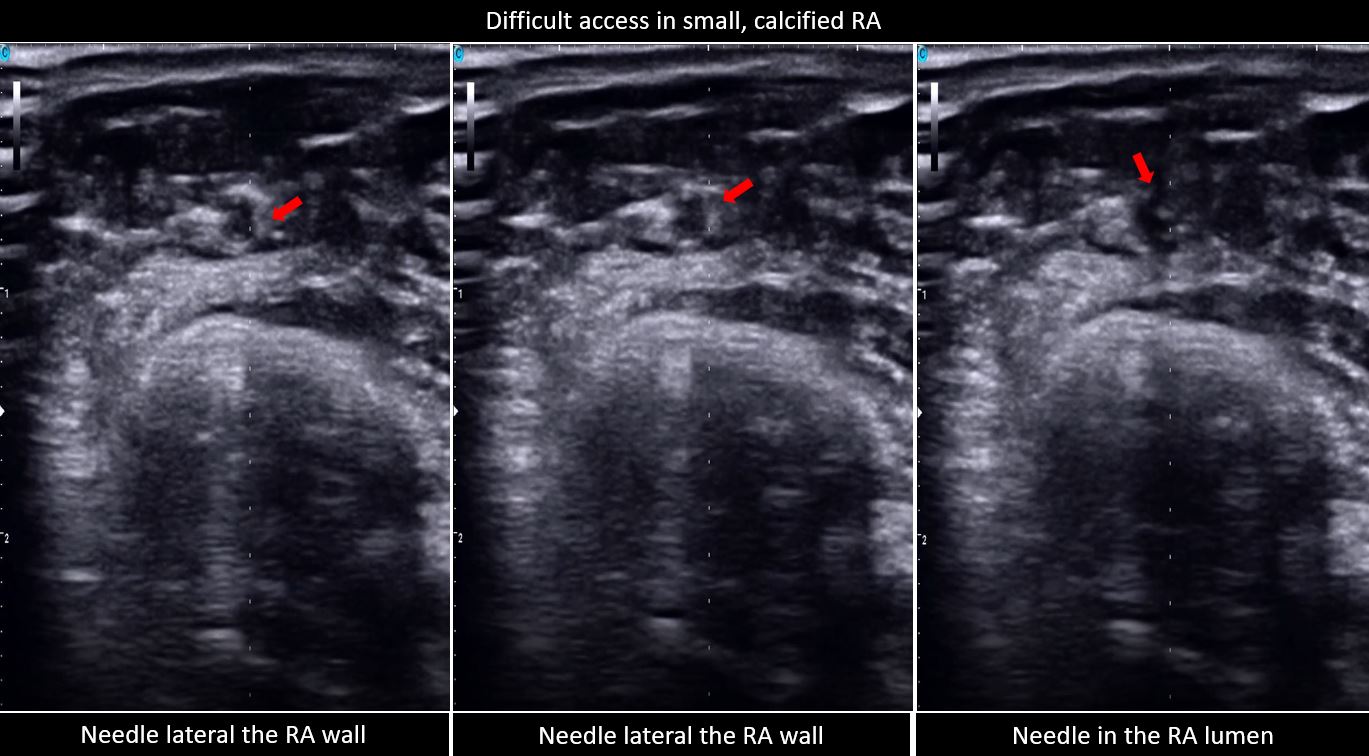
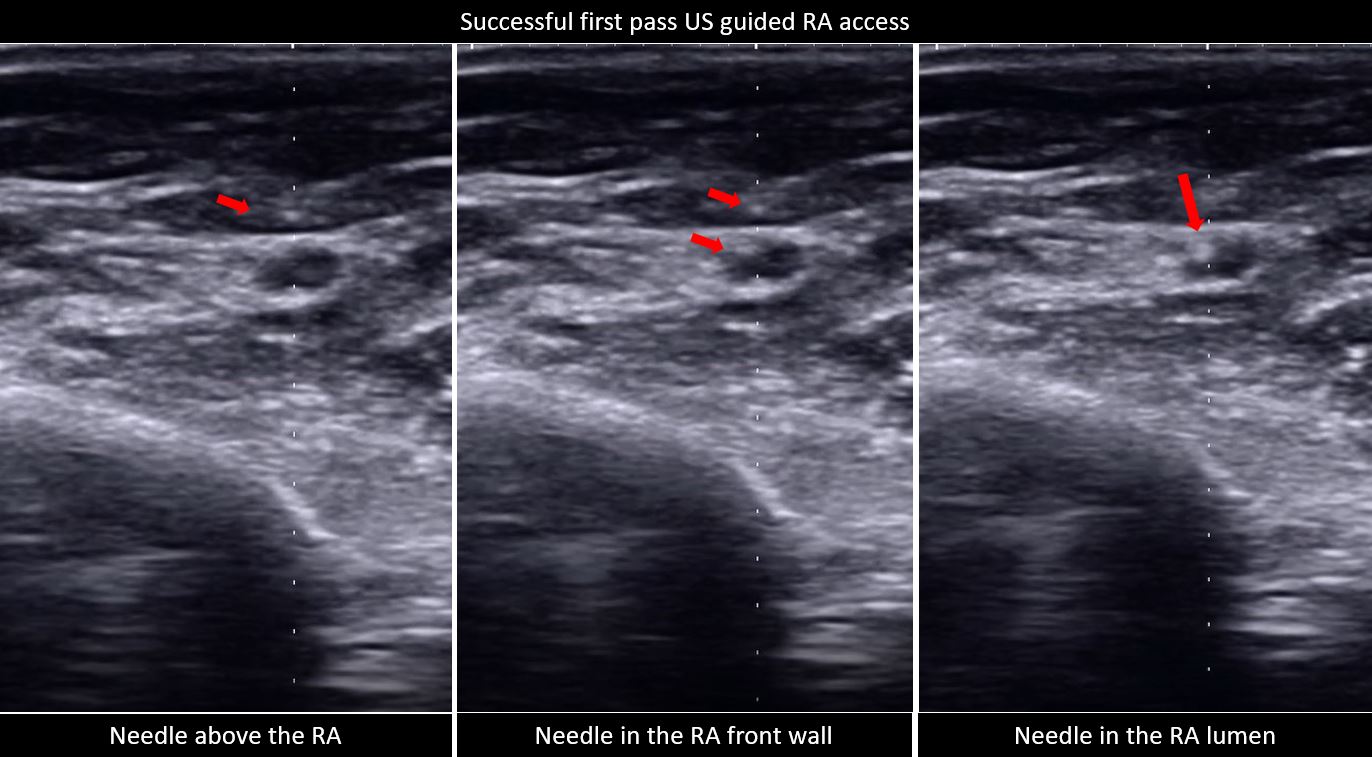
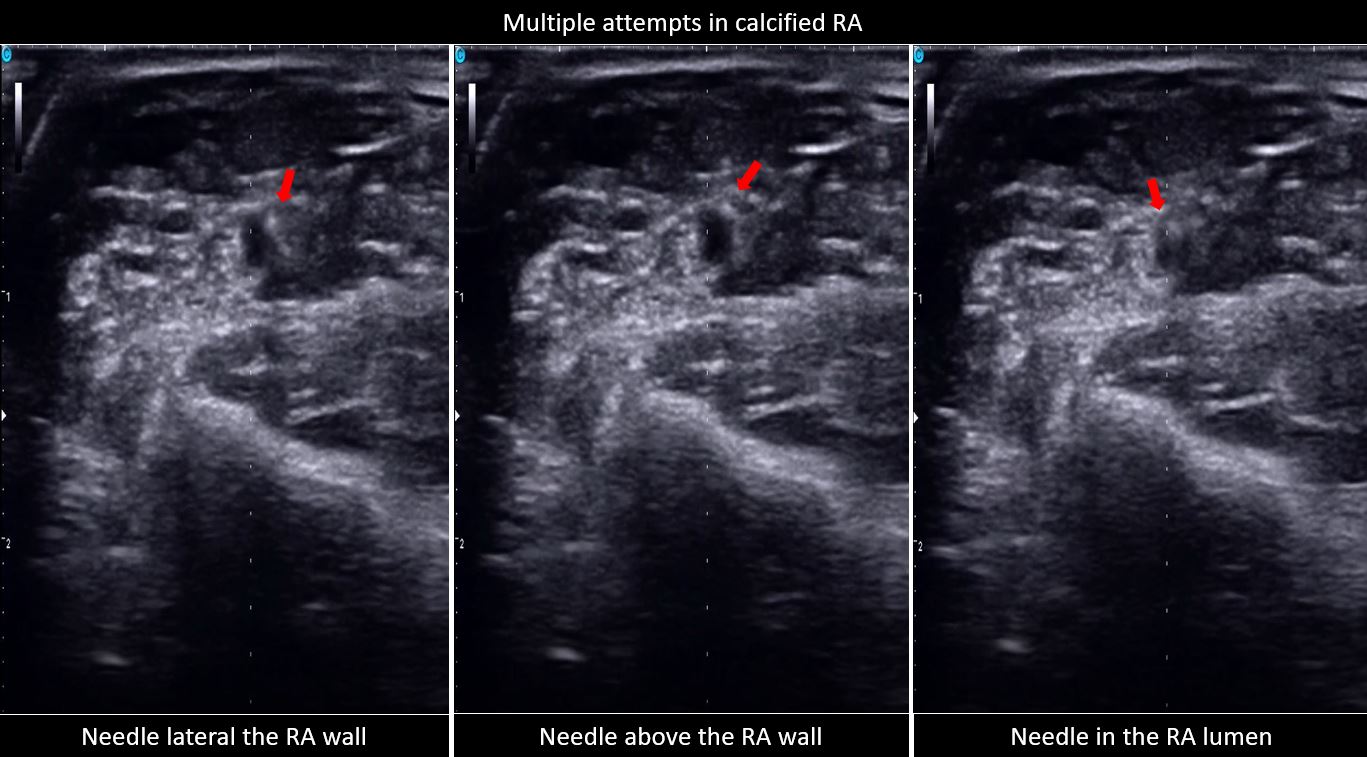
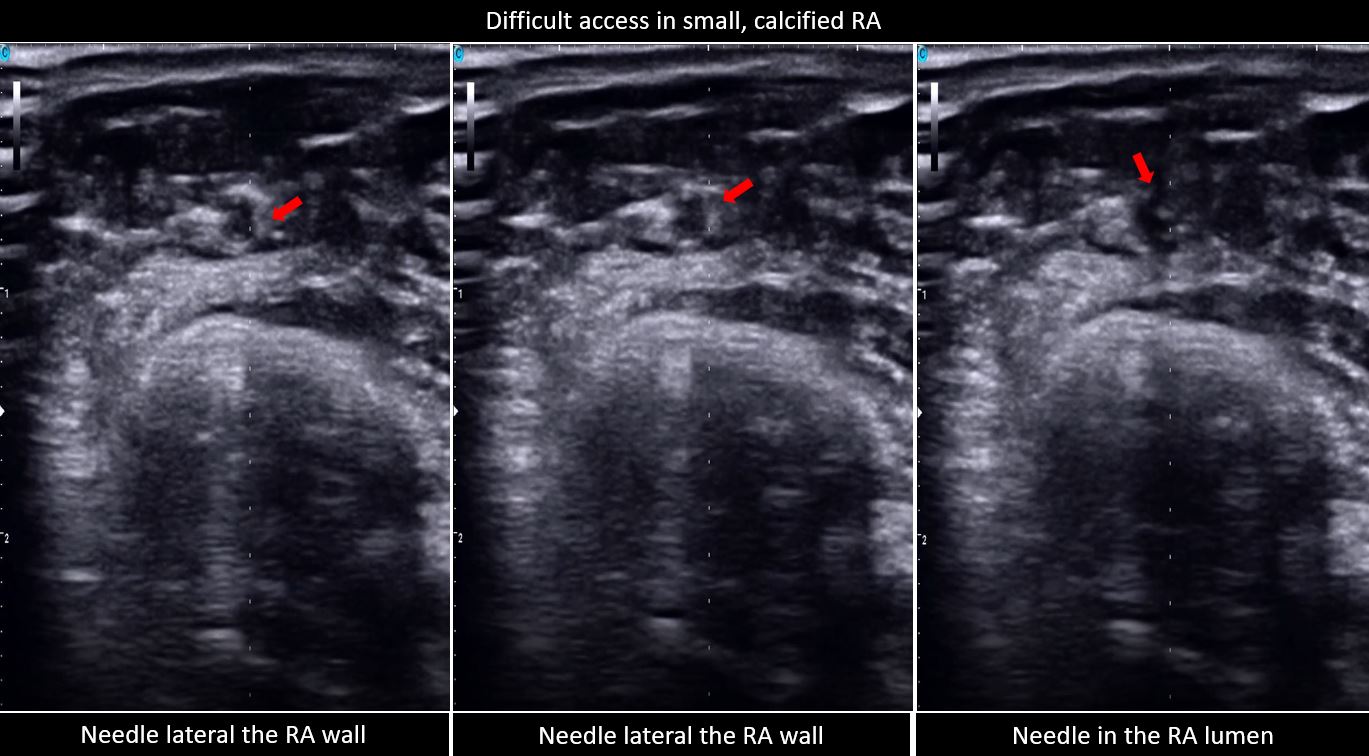
Between June 1 to September 1, 2022, two were excluded due to non-palpable pulse and were determined to have a hypoplastic RA size of 1.3 mm, and the other with radial artery occlusion, a monophasic signal on US. A total of 182 patients were grouped to palpation (n= 91) and US (n= 91) guidance. The baseline characteristics for both groups were comparable except for the significantly higher prevalence of patients with chronic kidney disease, in the US group (Table 1). The US group also has a significantly higher prevalence of RA calcifications and used larger sheath sizes for access. The rest of the procedural characteristics have no significant differences, including radial size, depth, type of procedure, technique for access, and medications administered (Table 2). The procedural outcomes showed a significantly higher first pass success rate from the initial attempt to successful sheath aspiration with US versus palpation (76.92% vs. 49.45%, p 0.0001), with fewer number of attempts (1.46 ± 1 vs. 1.99 ± 1.46, p 0.004) and shorter amount of time (93.62 ± 44.04 vs. 120.44 ± 67.1, p 0.002). In both groups, there was no significant difference in the number of difficult access defined as more than 5 or more attempts and/or mins (Table 3, Figure 1). The clinical outcomes showed a significantly higher incidence of spasms in the palpation versus US group (15.38% vs 3.3%, p 0.0052) and a trend of an increased bleeding complication (20.88% vs 14.29%, p 0.2442), both groups showed low scores of patient-reported pains. A total of 9 patients were required to cross over to another site, 3 in each group occurred after sheath insertion due to severe spasm and arteria lusoria. None of the cross overs from the US group occurred before sheath insertion while 3 from the palpation group were due to loss of pulse from repeated attempts and 1 was rescued by US (Table 4). Subgroup analysis demonstrated a consistent benefit of US use, especially in calcified RA, but not on small radial size per se (Figure 2). Post hoc analysis revealed a trend of inverse correlation between RA size and the number of attempts (r -0.098, p 0.187).
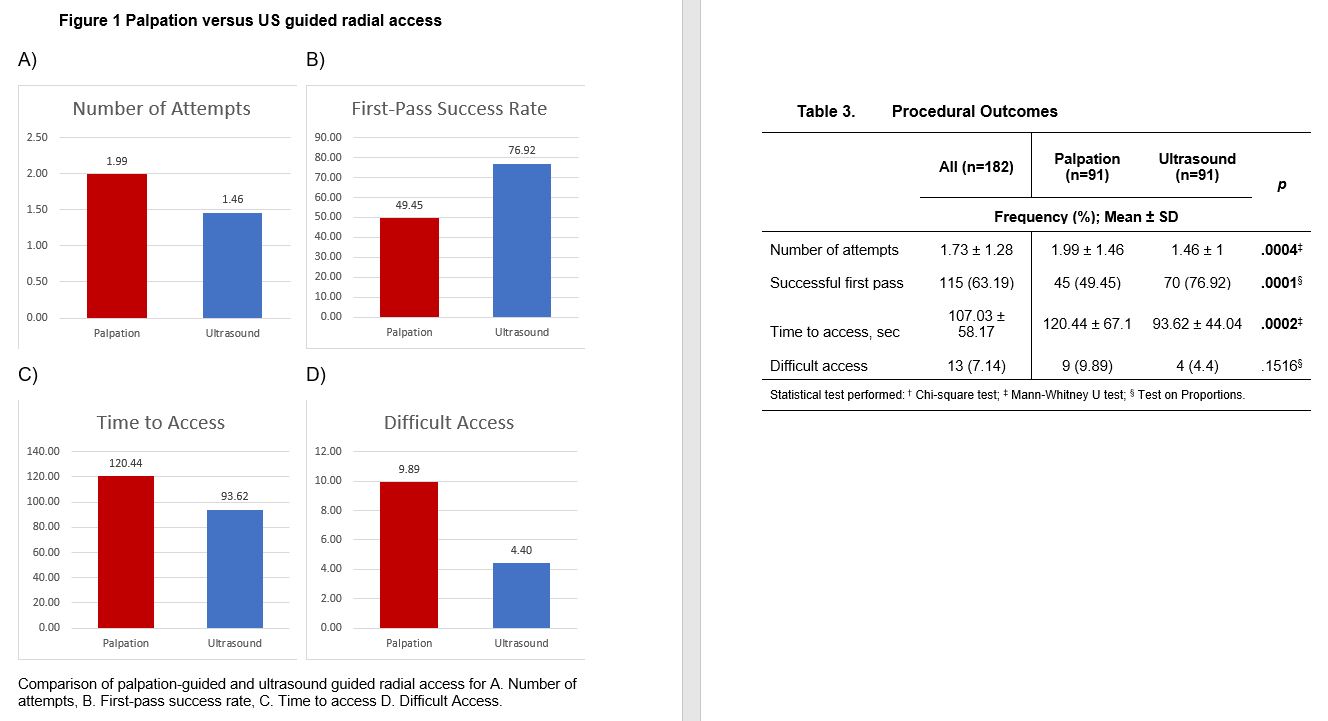
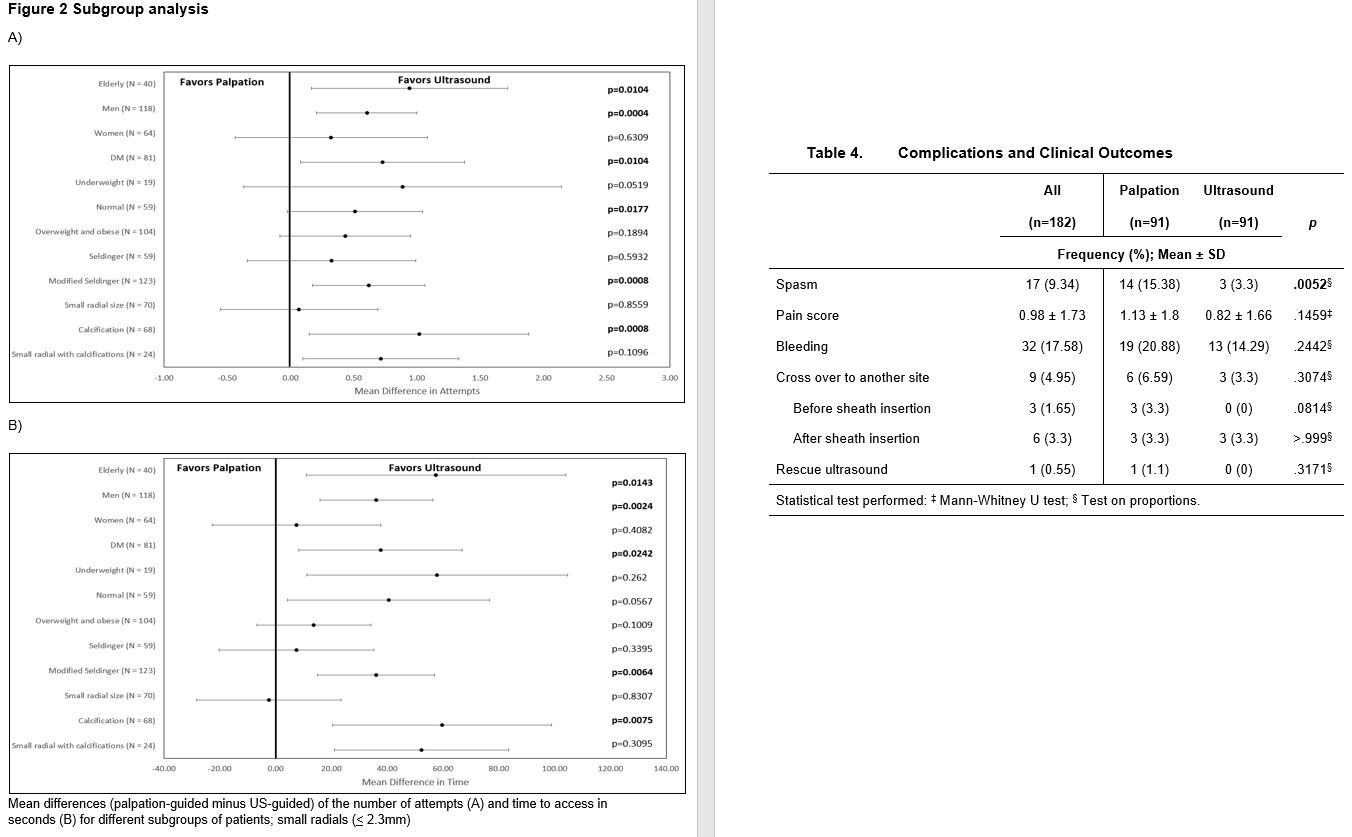
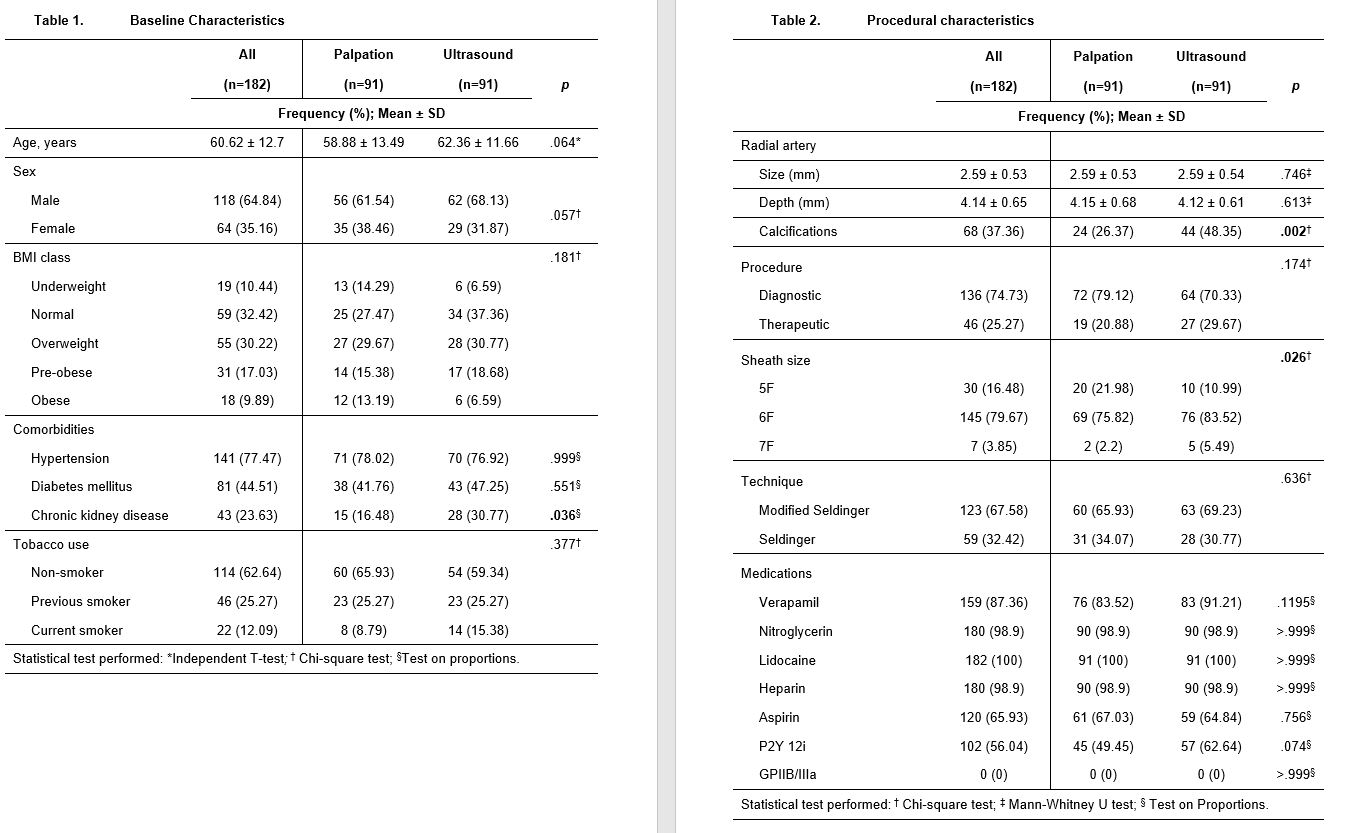
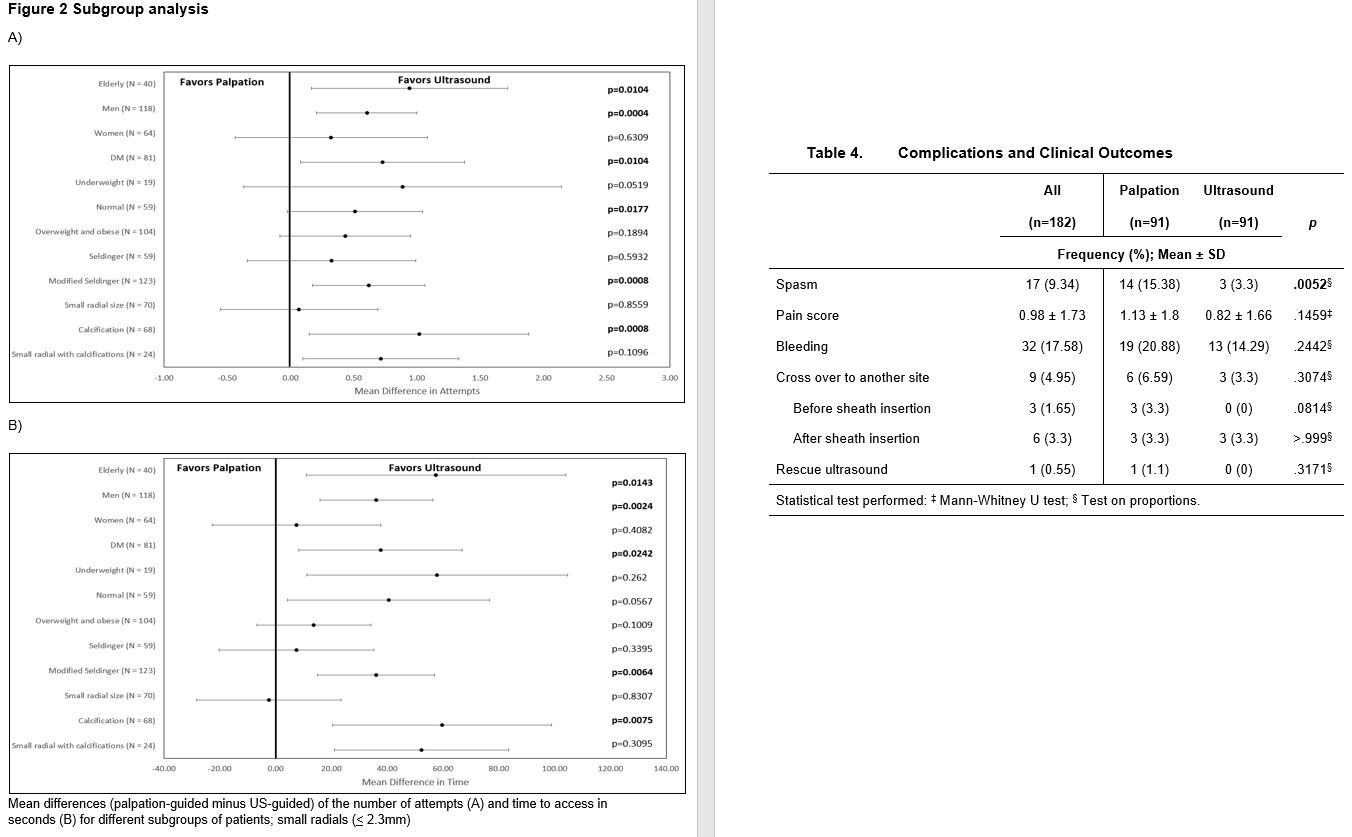
Conclusion
This single-center study compared the mode of radial access for cardiac catheterization procedures and demonstrated that the operator’s time and effort and the patient’s comfort were improved with procedural US over palpation guidance. In addition, the presence of calcifications, as seen in pre-procedural US favors the use of US over palpation and recommendations to do US screening before deciding which mode of radial access will likely increase procedural success. However there is a need to develop proficiency in ultrasound guided radial access for small radial arteries.