Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP C-036
Presenter
Kim Fong Ng
Authors
Kim Fong Ng1, Chuey Yan Lee2, Mahadevan Gurudevan3, Heng Shee Kim1, Kumutha Gobal1, Adelyn Nisha Henry1, Vicknesan Kulasingham4, Tee Choon Keong1, Azrina Abdul Kadir5, Hou Tee Lu1
Affiliation
Sultanah Aminah Hospital, Malaysia1, Hospital Sultanah Aminah, Malaysia2, Sultanah Amina Hospital, Malaysia3, Ministry of Health Malaysia, Malaysia4, KPJ Bandar Dato Onn Specialist Hospital, Malaysia5,
View Study Report
TCTAP C-036
CORONARY - Bifurcation/Left Main Diseases and Intervention
Urgent PCI in a Complex Left Main Bifurcation for an ESRD Patient with Recurrent ACS
Kim Fong Ng1, Chuey Yan Lee2, Mahadevan Gurudevan3, Heng Shee Kim1, Kumutha Gobal1, Adelyn Nisha Henry1, Vicknesan Kulasingham4, Tee Choon Keong1, Azrina Abdul Kadir5, Hou Tee Lu1
Sultanah Aminah Hospital, Malaysia1, Hospital Sultanah Aminah, Malaysia2, Sultanah Amina Hospital, Malaysia3, Ministry of Health Malaysia, Malaysia4, KPJ Bandar Dato Onn Specialist Hospital, Malaysia5,
Clinical Information
Patient initials or Identifier Number
Mr SS
Relevant Clinical History and Physical Exam
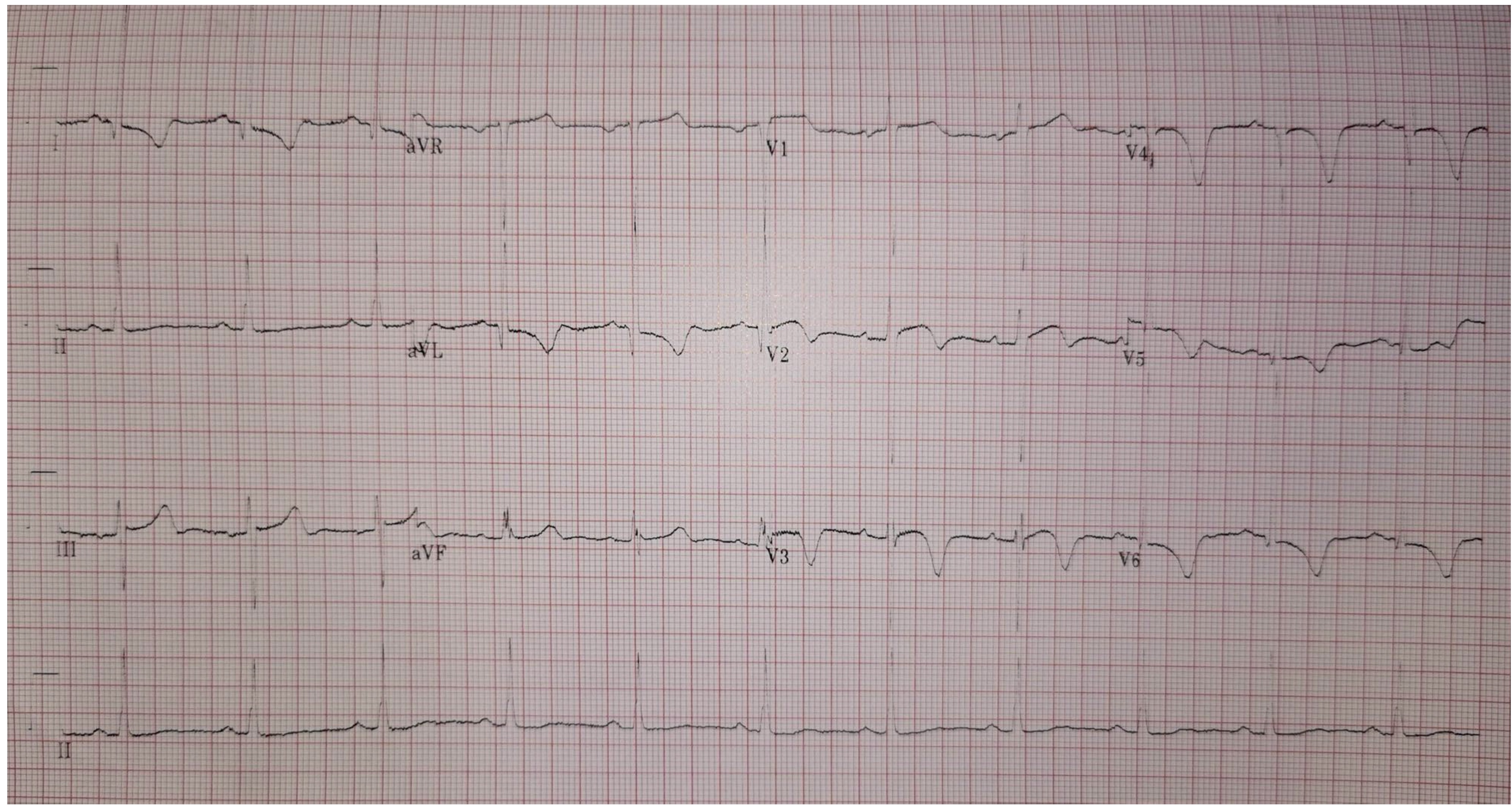
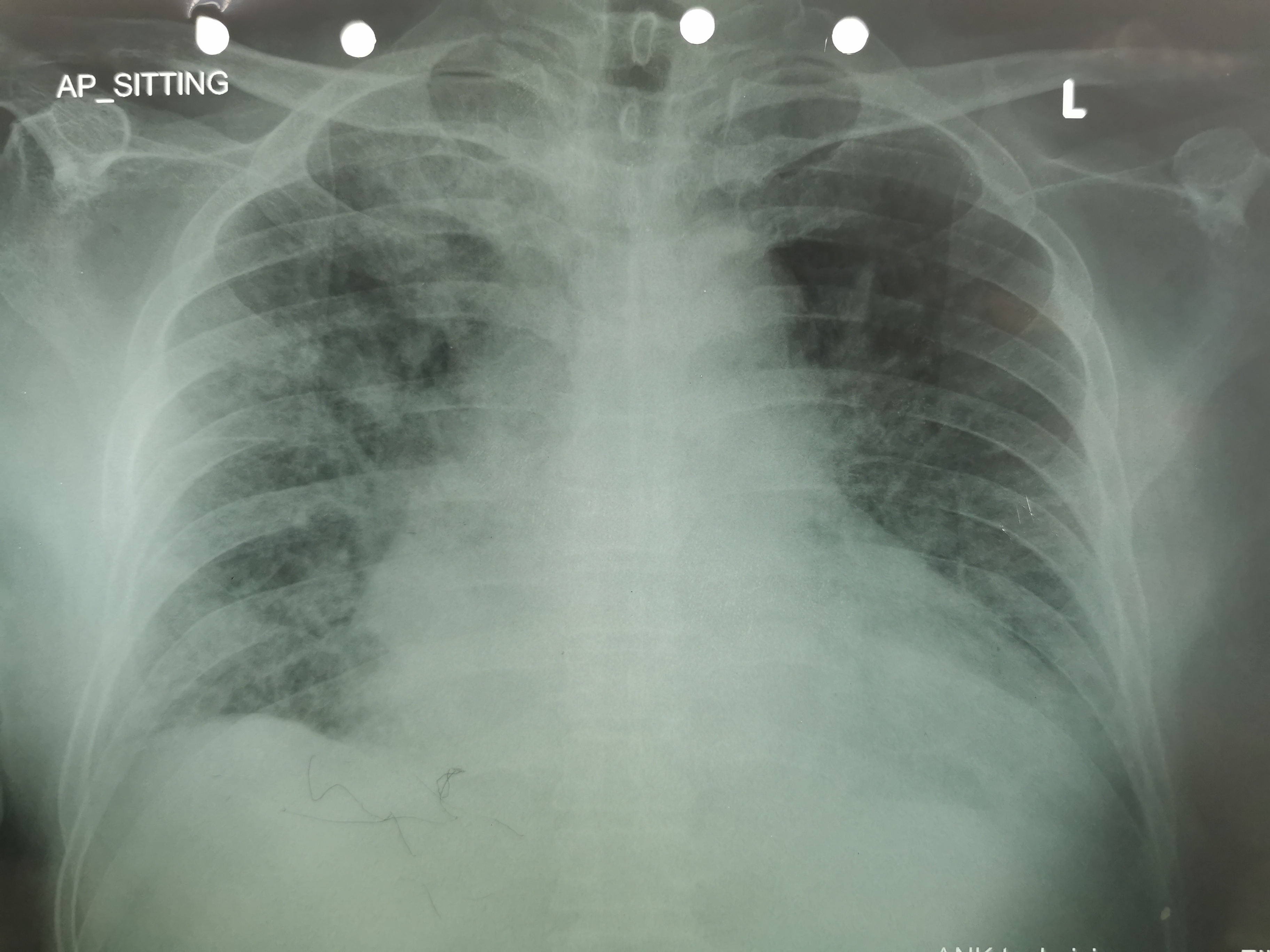
A 70-year-old male, non-smoker with background history of diabetes mellitus, hypertension, benign prostate hypertrophy, and end stage renal disease on regular haemodialysis presented with multiple admissions of unstable angina and NSTEMI.Patient developed hypotension due to poor tolerability with haemodialysis. Therefore, he was switched to peritoneal dialysis.His Blood pressure was 106/60 mmHg and pulse rate was 62/min.Respiratory examination revealed bibasal crepitation.
Relevant Test Results Prior to Catheterization
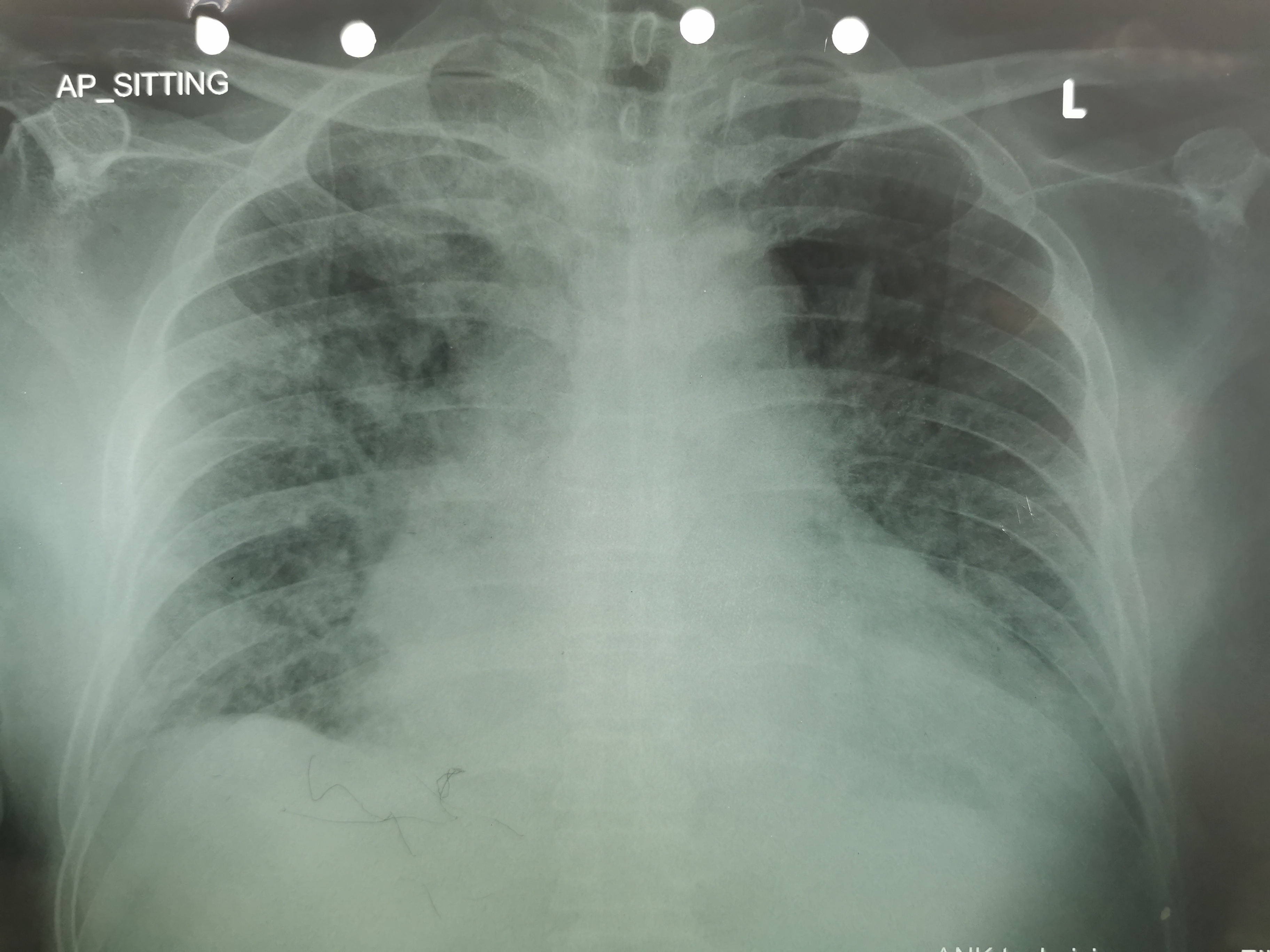
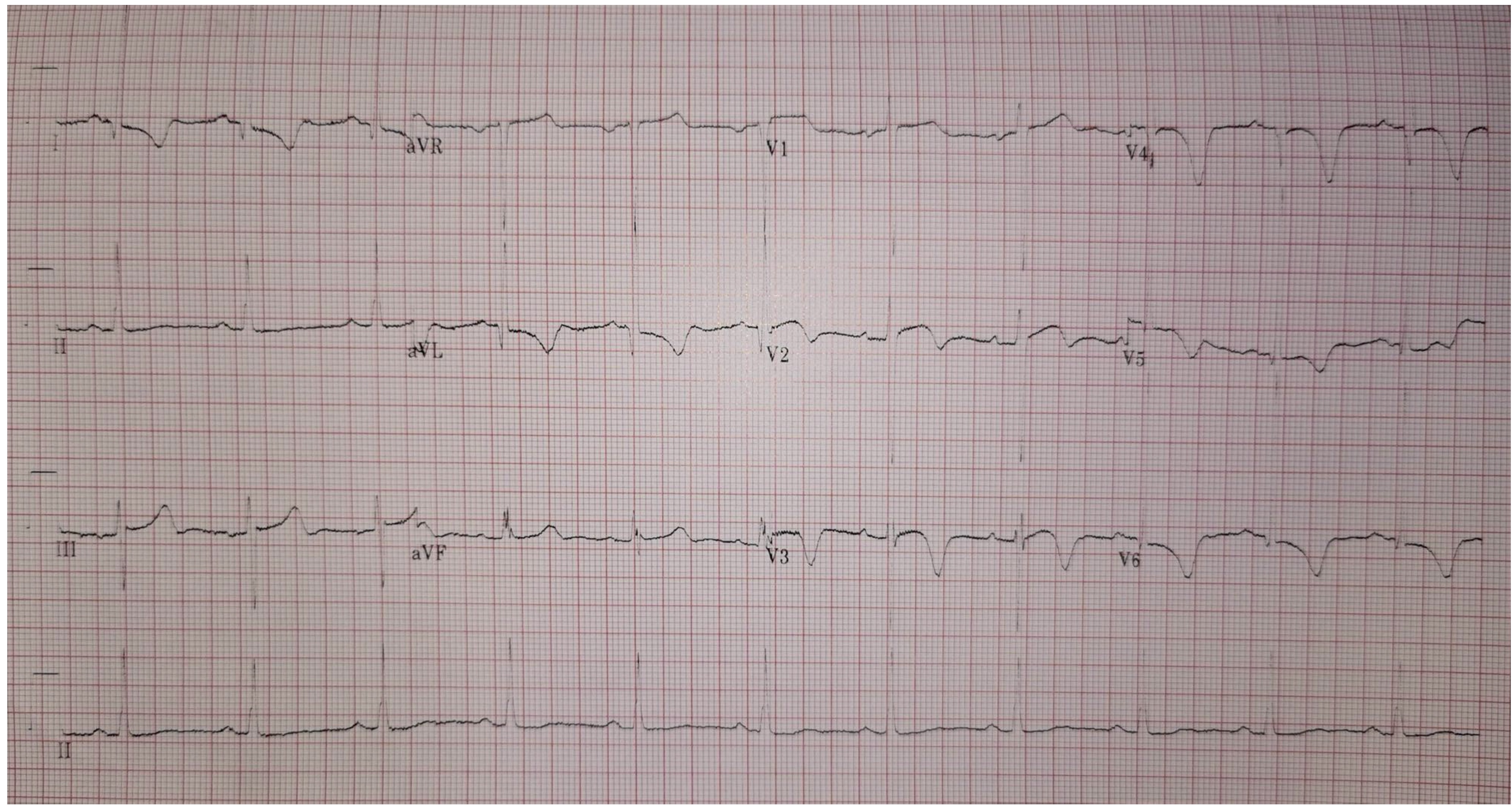
Blood investigations showed Hb of 12.1g/dl, creatinine 603 μmol/L, troponin T 2265.Echocardiography examination revealed reduced left ventricular function with ejection fraction of 40%, dilated left atrial, global hypokinetic and there was no clot or thrombus observed.There was also no pericardial effusion observed.ECG showed LVH pattern and T wave inversion V2 to V6.
 3.mov
3.mov
 2.mov
2.mov
 4.mov
4.mov
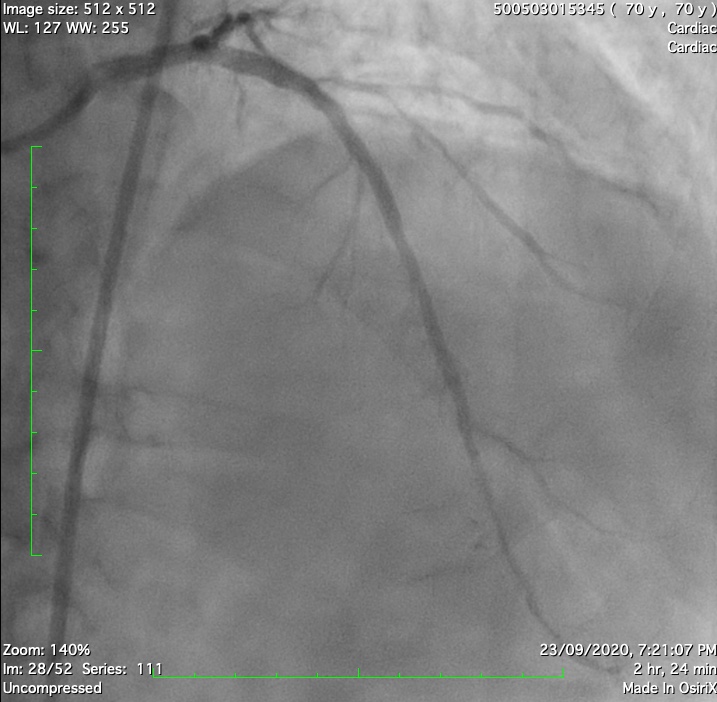
Relevant Catheterization Findings
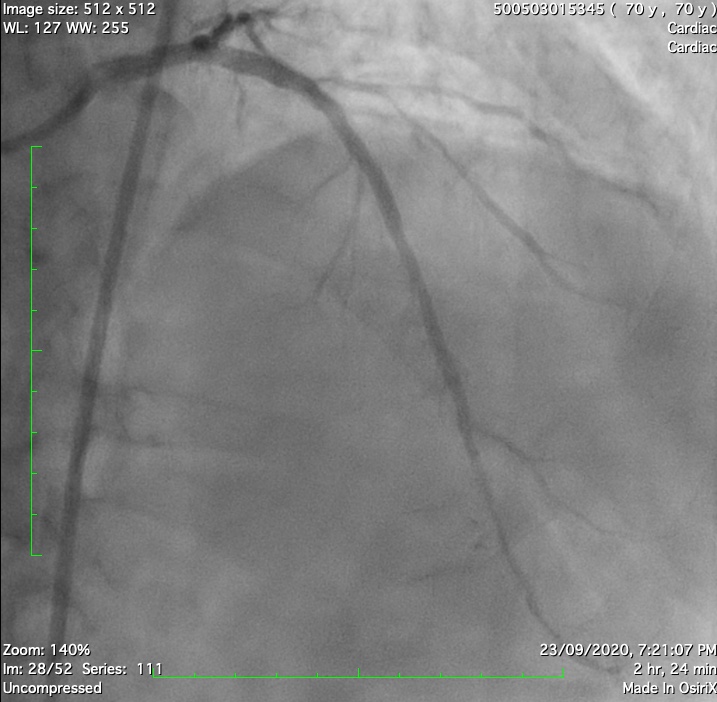
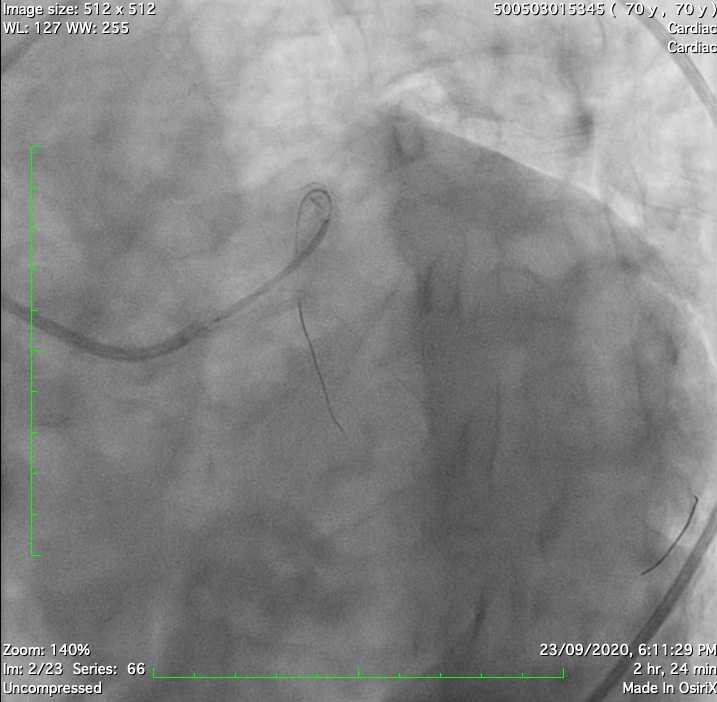
Coronary angiography showed LMT 50% stenosis, prox and mid LAD 90%, D1 artery 70% stenosis, and diffuse LCX disease where the ostial to distal is 70 % to 90% with medina classification 1,1,1 (LMT, LAD & LCX).He was referred for inpatient CABG and his calculated Society of Thoracic Surgeons (STS) risk score for mortality is 5% and Syntax Score is 32.However, after a discussion on his risk of CABG, the patient refused to undergo CABG procedure.Taking patient decision into consideration, we proceed to high risk PCI.
 8.mov
8.mov
 7.mov
7.mov
 6.mov
6.mov
Interventional Management
Procedural Step
The right femoral artery (RFA) was punctured. IABP was on standby mode.
A 7Fr JL 4 was used to engage LMT. A BMW II J tip wire was inserted into LCx and another wire runthrough floppy wired down to LAD. The LCx was predilated by NC 2.5x12mm balloon.
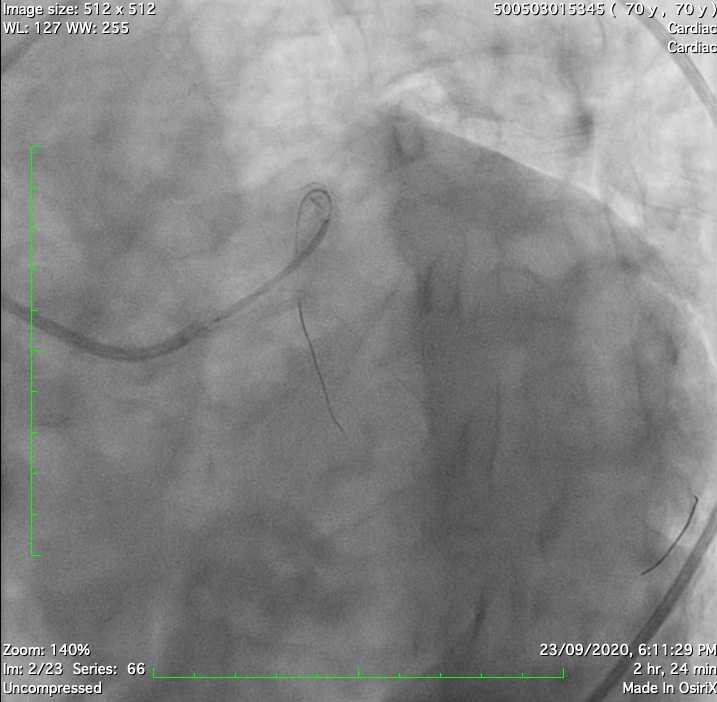

A 7Fr JL 4 was used to engage LMT. A BMW II J tip wire was inserted into LCx and another wire runthrough floppy wired down to LAD. The LCx was predilated by NC 2.5x12mm balloon.

Case Summary
PCI is an alternative treatment strategy for high surgical risk patients, especially with ESRD & recurrent NSTEMI