Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP C-110
Presenter
Hsinyu Tseng
Authors
Hsinyu Tseng1, Yen-Hung Lin1
Affiliation
National Taiwan University Hospital, Taiwan1,
View Study Report
TCTAP C-110
STRUCTURAL HEART DISEASE - Pulmonary Intervention: CTEPH, PHTN
Efficacy of Serial Balloon Pulmonary Angioplasty in Treating an Octogenarian with Severe Chronic Thromboembolic Pulmonary Hypertension and Right Heart Failure
Hsinyu Tseng1, Yen-Hung Lin1
National Taiwan University Hospital, Taiwan1,
Clinical Information
Patient initials or Identifier Number
Lee
Relevant Clinical History and Physical Exam
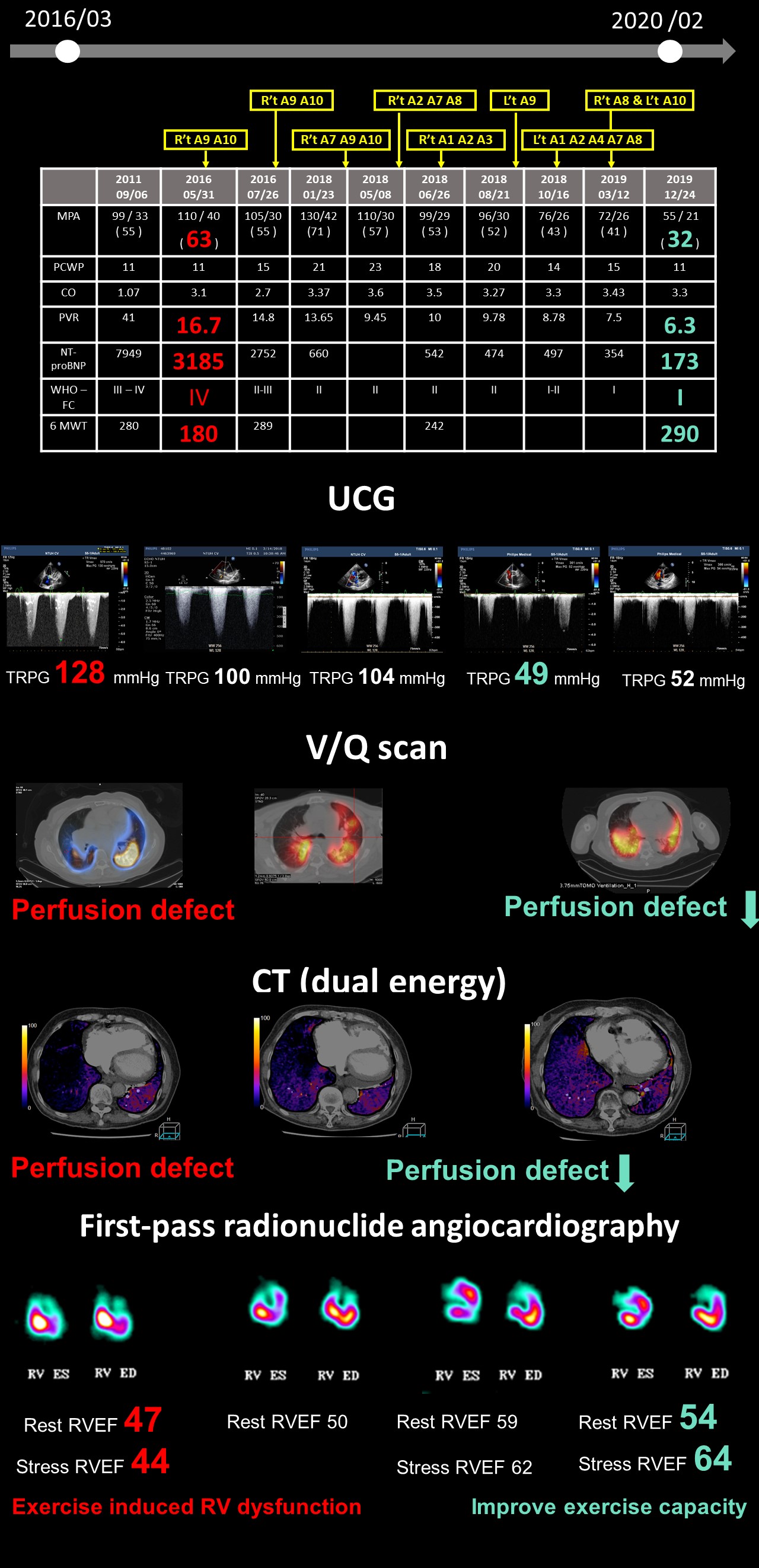
A 76-year-old female presented with progressive dyspnea for years. She had a history of pulmonary embolism at age of 67 and diagnosed of chronic thromboembolic pulmonary hypertension (CTEPH) at age of 71. She had been enrolled in the CHEST-1 clinical trial and riociguat (Adempas) had been administered for 5 years. However, progressive exertional dyspnea developed (WHO functional classification: IV). Physical examination showed RV heave, prominent P2 and bilateral leg edema.
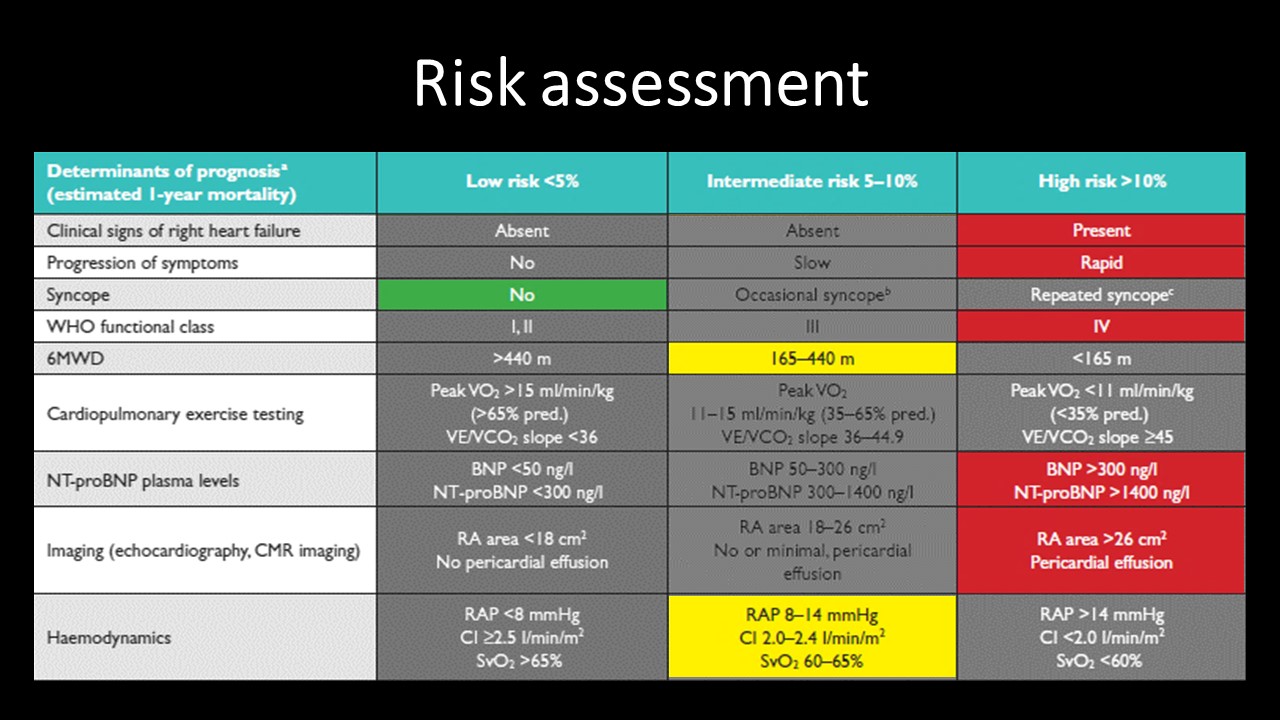
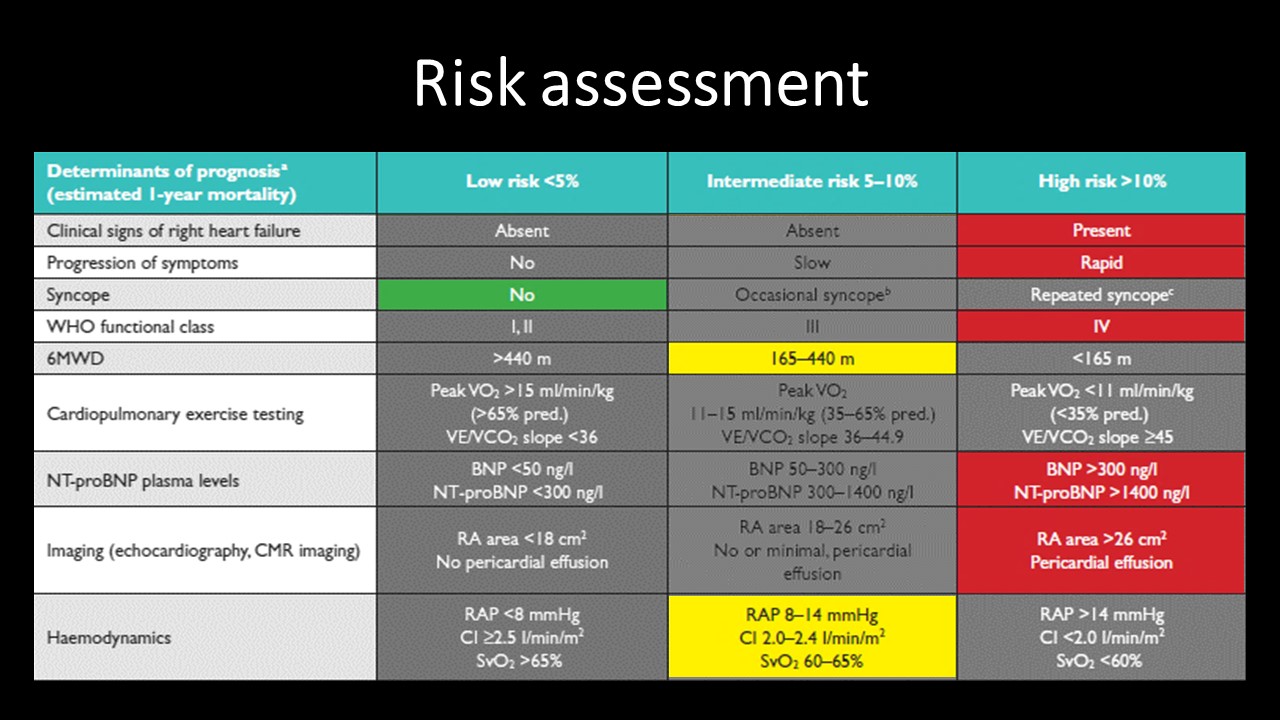
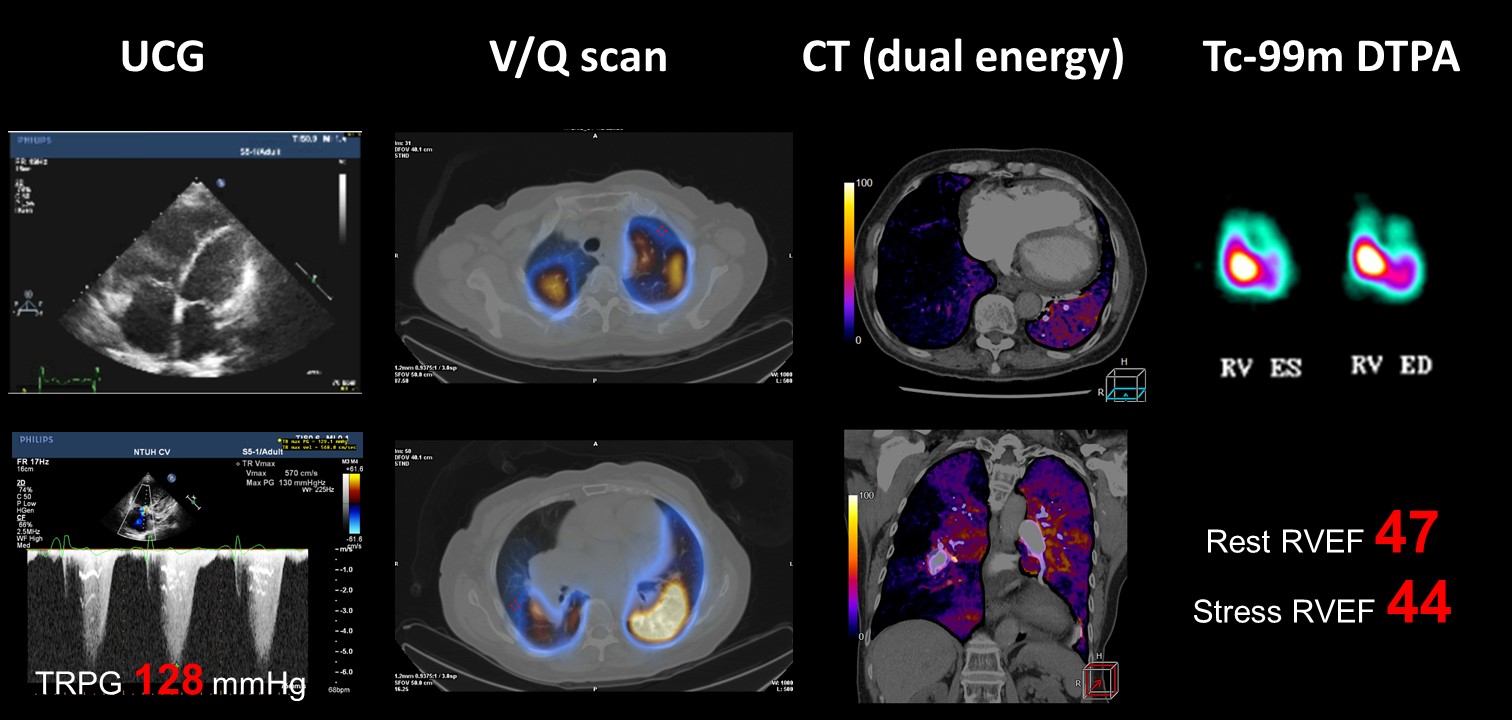
Relevant Test Results Prior to Catheterization
ECG showed right axis deviation and right ventricular hypertrophy. CXR disclosed cardiomegaly with prominent right pulmonary trunk. NT-proBNP was 3,185 pg/ml. Six Minute Walk Test (6WMT) was 180 meters. Echocardiogram confirmed enlarged right heart and elevated TRPG (128 mg). Ventilation/Perfusion scan revealed bilateral perfusion defects with most severe defect at right lower lung. Tc-99m DTPA first-pass radionuclide angiocardiography reported borderline decreased RV systolic function.
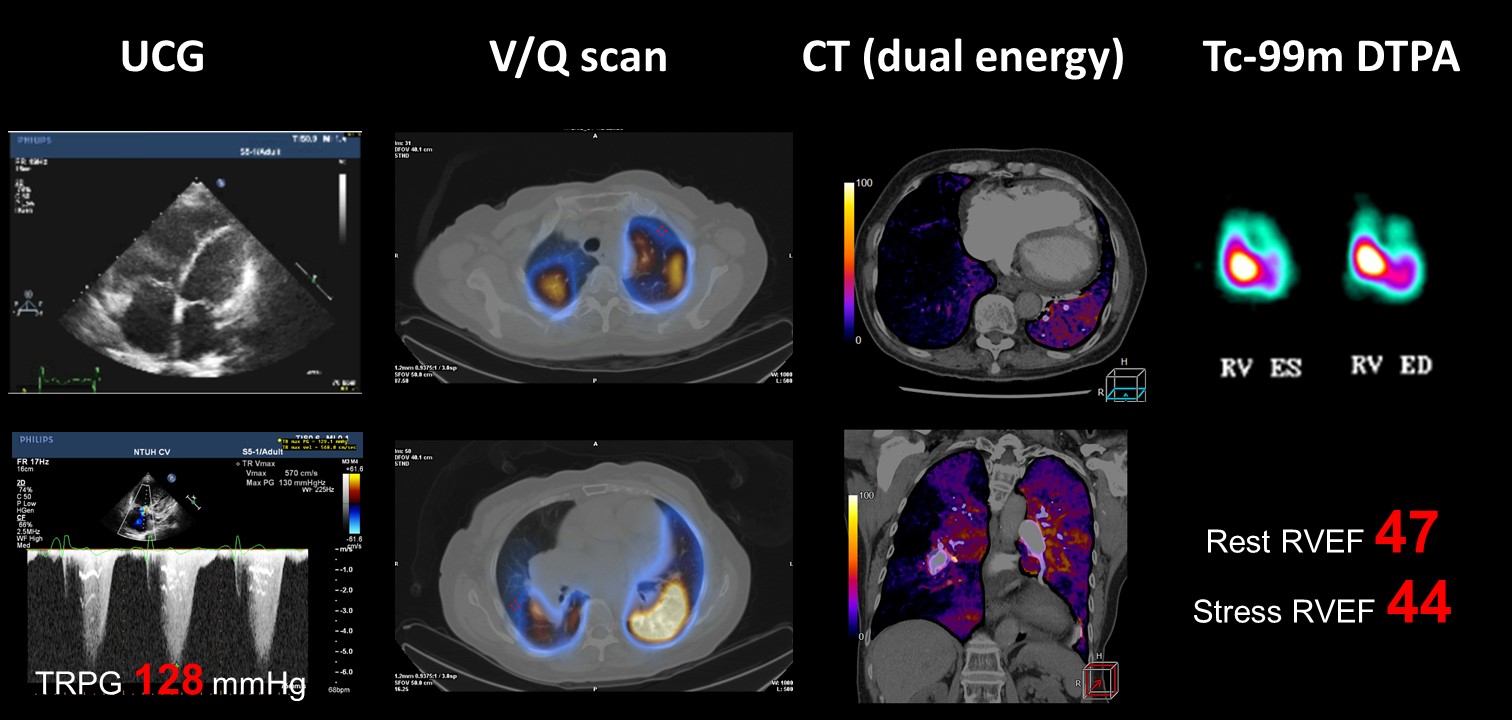
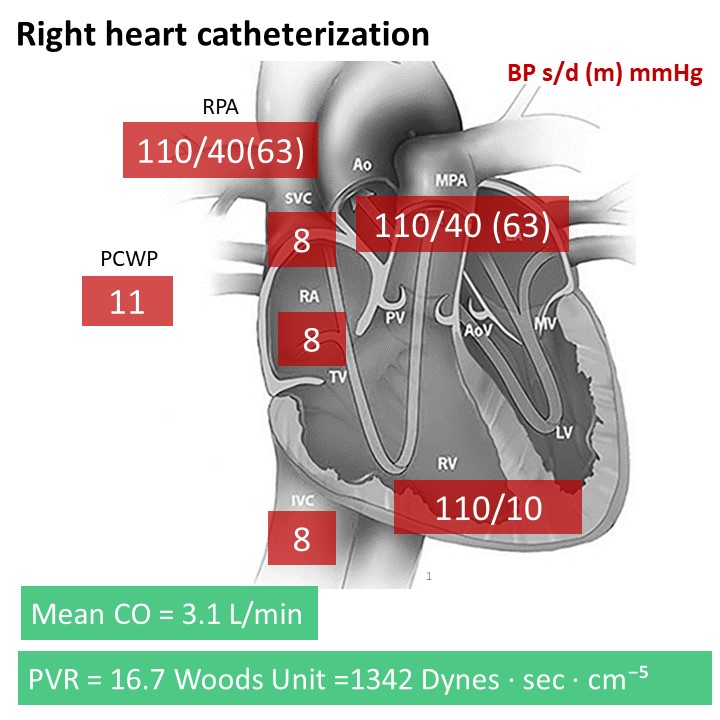
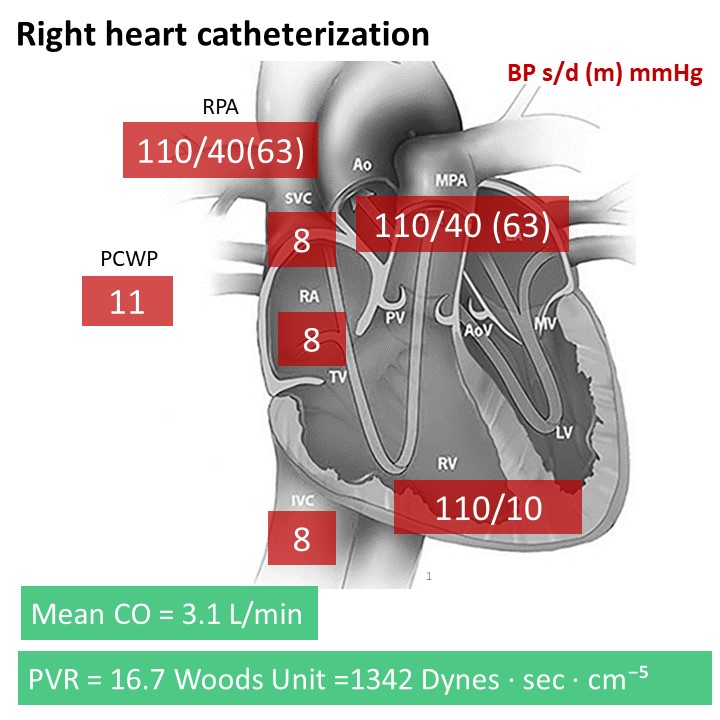
Relevant Catheterization Findings
Right heart catheterization showed severe pulmonary hypertension with pulmonary artery pressure 110/40 (63) mmHg and extremely elevated pulmonary vascular resistance (16.7 Woods Unit). Non selective pulmonary angiography discovered multiple bilateral lower lung filling defect, especially in right lower lung field. Selective pulmonary angiography revealed severe stenosis at right A7, A9 and A10 with abrupt narrowing and webs & bands appearance.
 2. Relevant cath finding.mp4
2. Relevant cath finding.mp4
Interventional Management
Procedural Step
< 1st Balloon pulmonary angioplasty (BPA) >
 Video 1 Procedure.mp4
Video 1 Procedure.mp4
 Video 2 Pre and Post and Lung Edema.mp4
Video 2 Pre and Post and Lung Edema.mp4
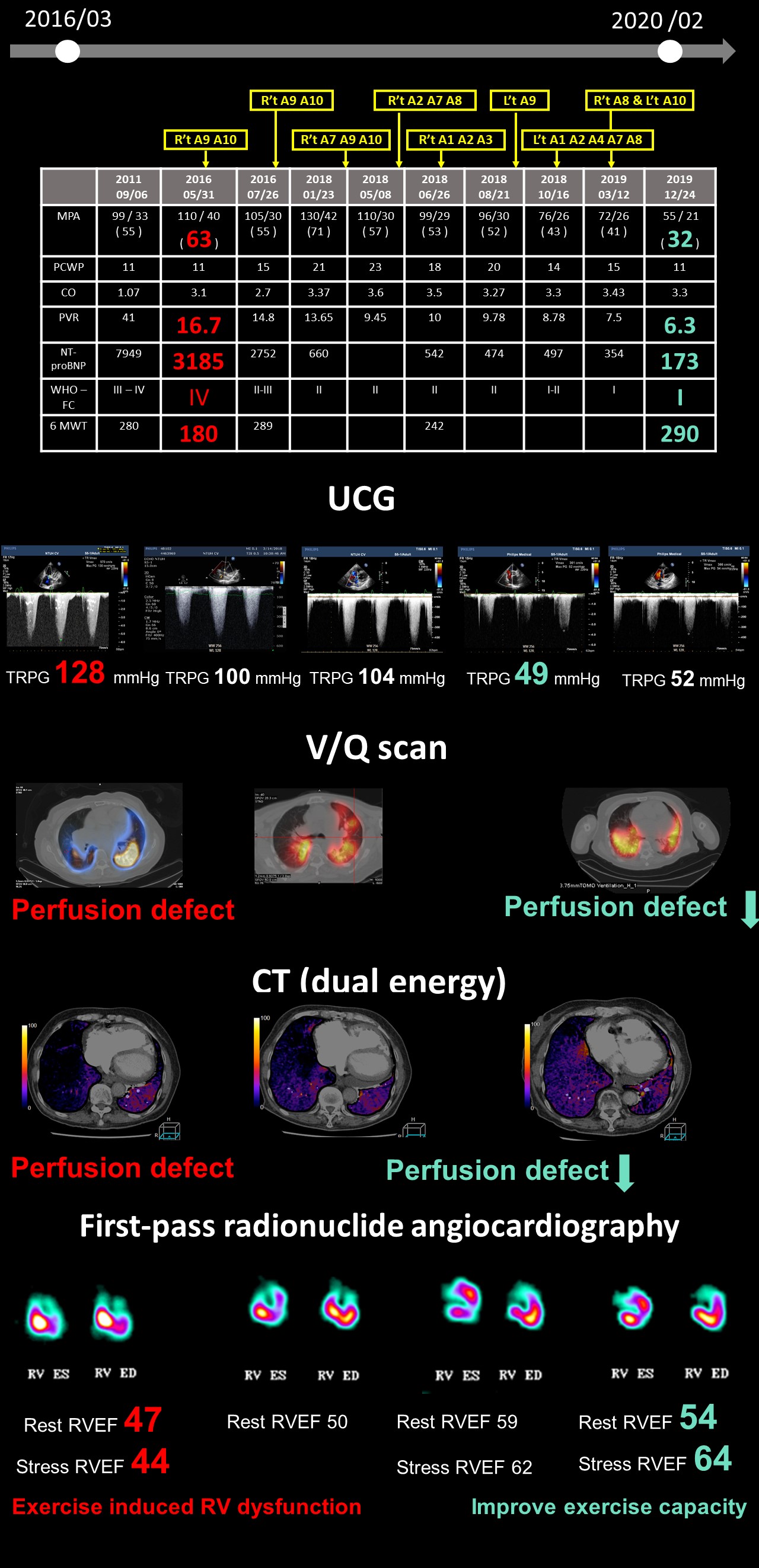
Case Summary
Balloon pulmonary angioplasty (BPA) is an effective treatment with acceptable procedure risk for inoperable CTEPH patients. Both clinical and hemodynamic parameters improved dramatically after BPA. However, difficult wiring and unique complications are frequently encountered. The challenge of difficult wiring can be conquered by long sheath, dual lumen catheter and careful manipulation of hydrophilic wires. Such techniques should be appropriately applied to facilitate procedure. In addition, PEPSI score is a useful tool to predict the development of reperfusion lung edema and should be implemented in daily practice.