Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP A-032
Presenter
Dae Young Hyun
Authors
Dae Young Hyun1, Myung-Ho Jeong2, Min Chul Kim1, Kyung Hoon Cho1, Doo Sun Sim1, Young Joon Hong1, Youngkeun Ahn1
Affiliation
Chonnam National University Hospital, Korea (Republic of)1, Gwangju Veterans Hospital, Korea (Republic of)2
View Study Report
TCTAP A-032
Hemodynamic Support and Cardiogenic Shock
Proper Application Time and Effect of Extracorporeal Membrane Oxygenation in the Patients Who Underwent Percutaneous Coronary Intervention for Acute Myocardial Infarction with Cardiogenic Shock
Dae Young Hyun1, Myung-Ho Jeong2, Min Chul Kim1, Kyung Hoon Cho1, Doo Sun Sim1, Young Joon Hong1, Youngkeun Ahn1
Chonnam National University Hospital, Korea (Republic of)1, Gwangju Veterans Hospital, Korea (Republic of)2
Background
There are limited data regarding proper time of application and long-term clinical outcomes of extracorporeal membrane oxygenation (ECMO) in patient with cardiogenic shock (CS). This study appraised the clinical outcomes according to ECMO application or not and ECMO application time in the patients with acute myocardial infarction (AMI) combined CS.
Methods
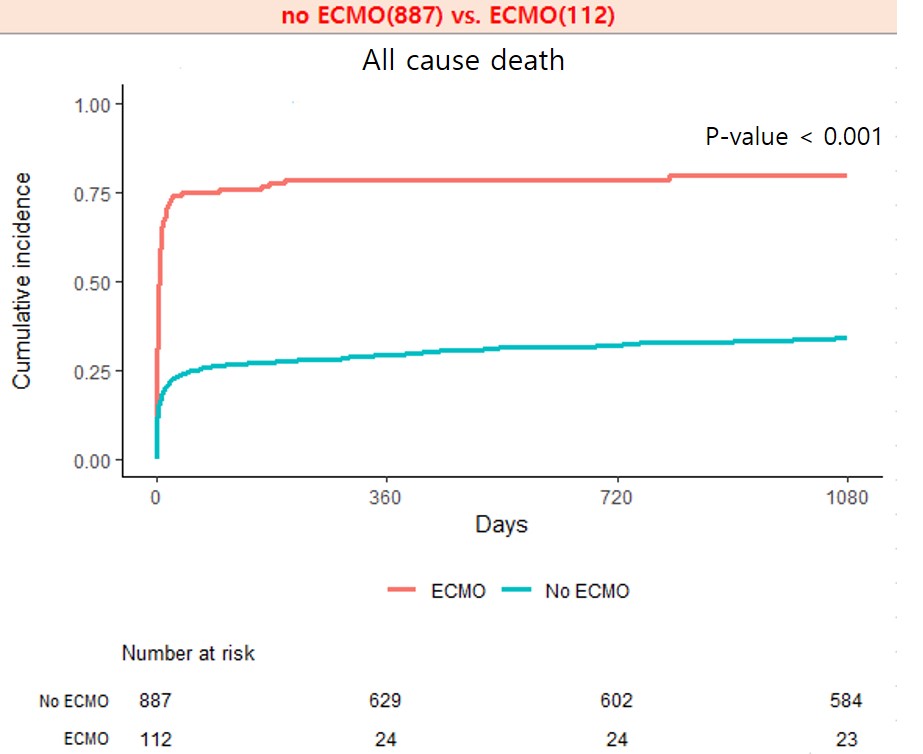
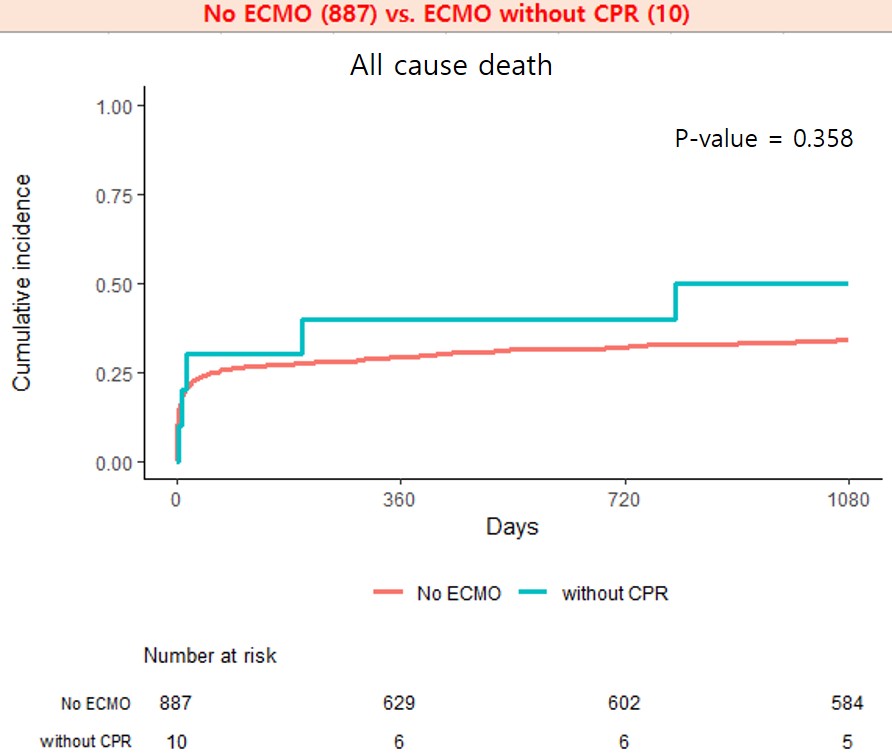
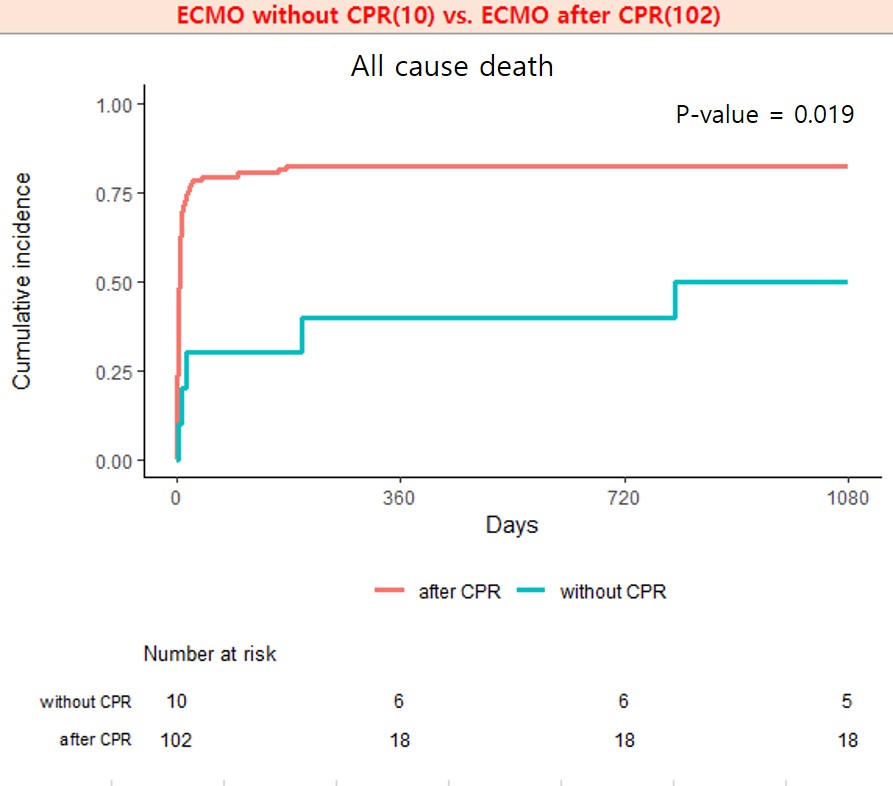
From 2011 to 2015, a total of 13,081 patients with AMI were enrolled in a nation-wide AMI registry. Eligible patients with CS who underwent percutaneous coronary intervention (PCI) and had 3-year clinical follow-up, were analyzed. The study patients were divided into two groups: no ECMO application group (n = 887, 627 men, 67.8 ± 12.4 years) and ECMO application group (n = 112, 88 men, 62.8 ± 11.6 years). The ECMO application group was divided into two groups again: ECMO without cardiopulmonary resuscitation (CPR) group (n = 10, 7 men, 61.3 ± 13.4 years) and ECMO after CPR group (n = 102, 81 men, 62.9 ± 11.5 years).
Results
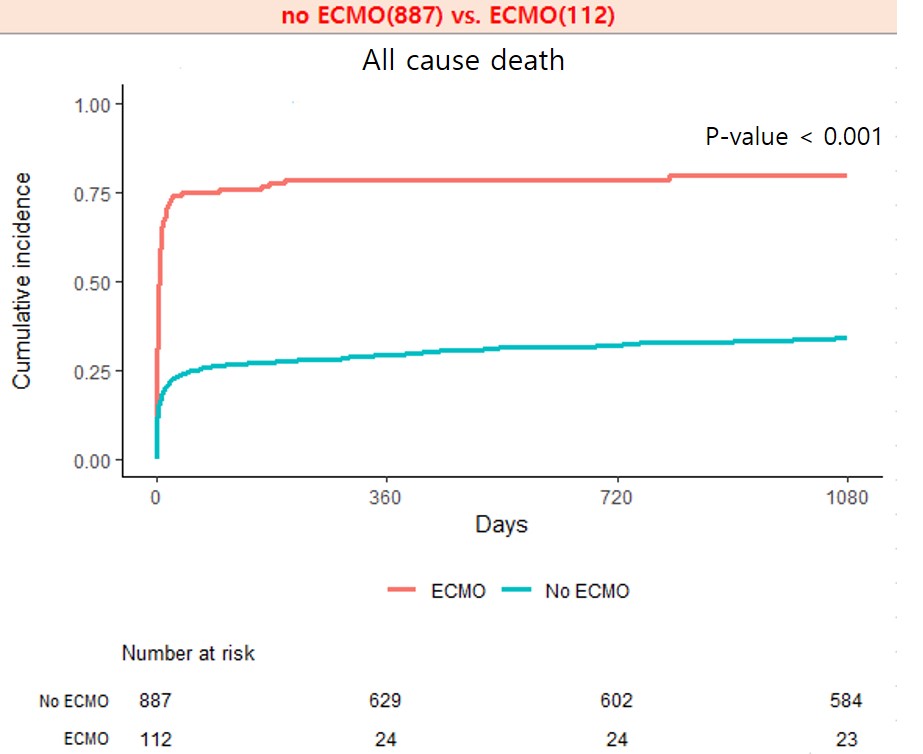
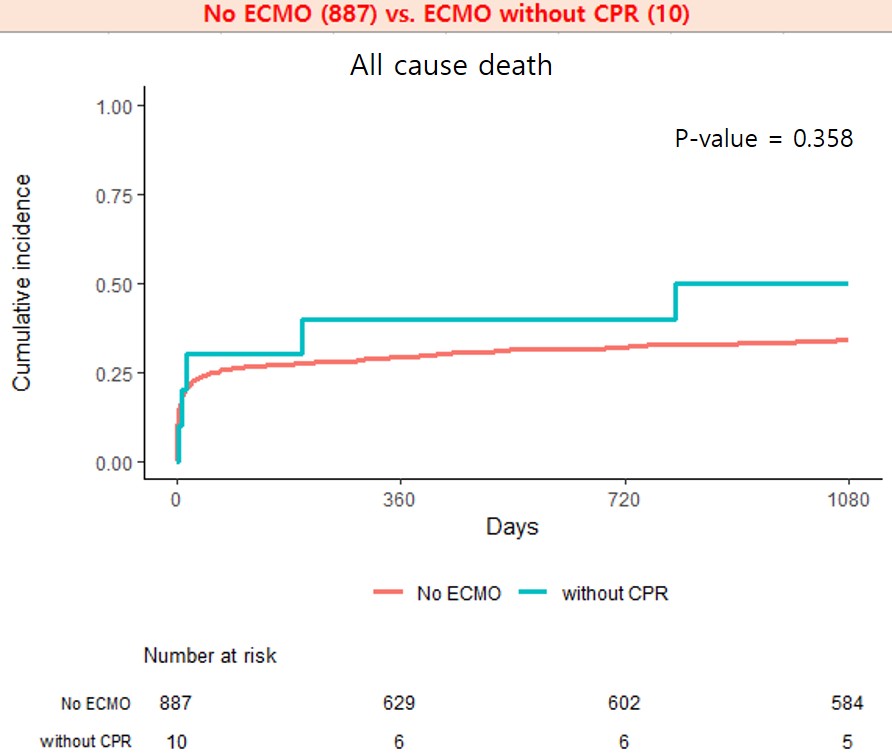
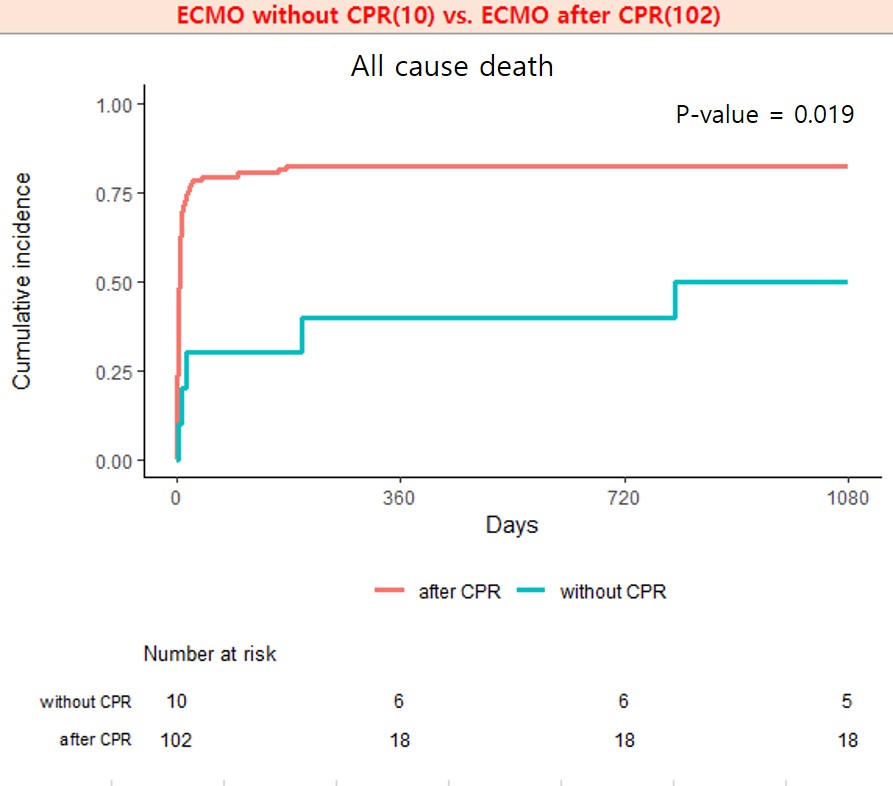
There was significant difference in all cause death between no ECMO application and ECMO application during three-year follow-up (n = 303, 34.2%vs. n = 89, 79.5%) (p < 0.001). However, ECMO application without CPR showed similar outcome compared with no ECMO application in three-year all cause death (n = 5, 50.0% vs. n = 303, 34.2%) (p = 0.358). And, all cause death during three-year follow-up was significantly lower in ECMO application without CPR than ECMO application after CPR (n = 5, 50.0% vs. n = 84, 82.4%) (p = 0.019).
Conclusion
So far, ECMO has been used as the last remedy for rescue and it has not been used frequently before patient’s condition got worse. In this study, ECMO before CPR showed good long-term clinical outcome. So early application of ECMO can be considered as a good procedure strategy in patients with CS with AMI.