Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP A-048
Presenter
Nao Yasuda
Authors
Nao Yasuda1
Affiliation
Nagoya Ekisaikai Hospital, Japan1
View Study Report
TCTAP A-048
Physiologic Lesion Assessment
Assessment of Diagnostic Accuracy by Each Resting Index - Comparison with FFR
Nao Yasuda1
Nagoya Ekisaikai Hospital, Japan1
Background
Strategy based of physiological assessment by iFR (instantaneous wave-free ratio
Methods
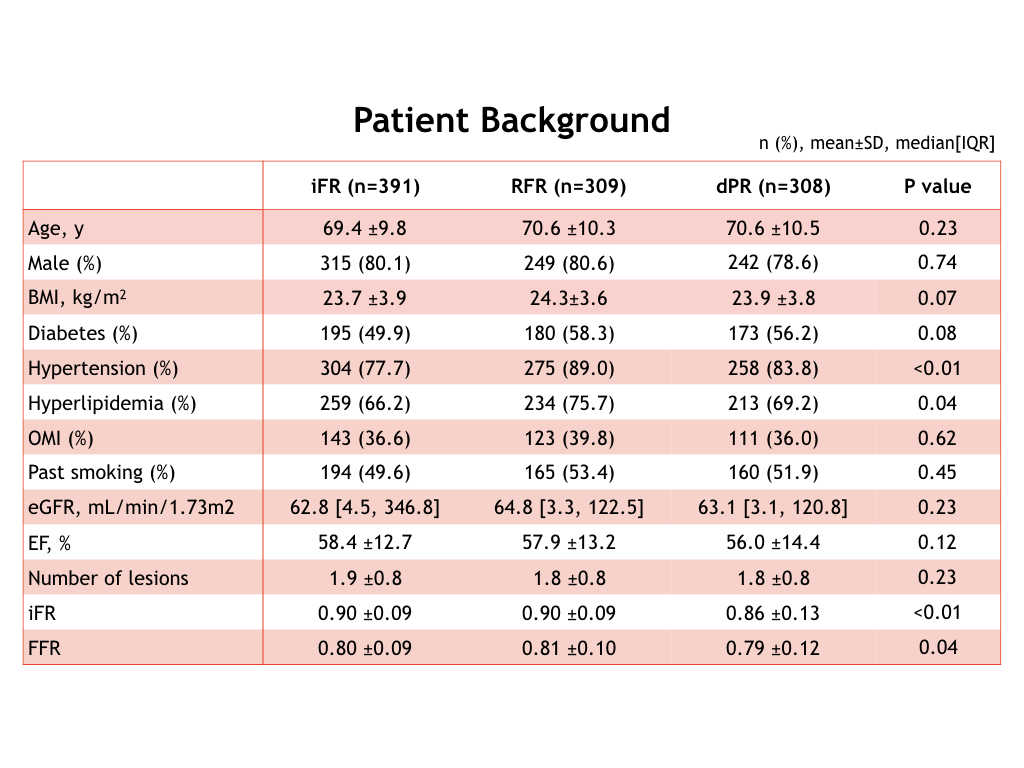
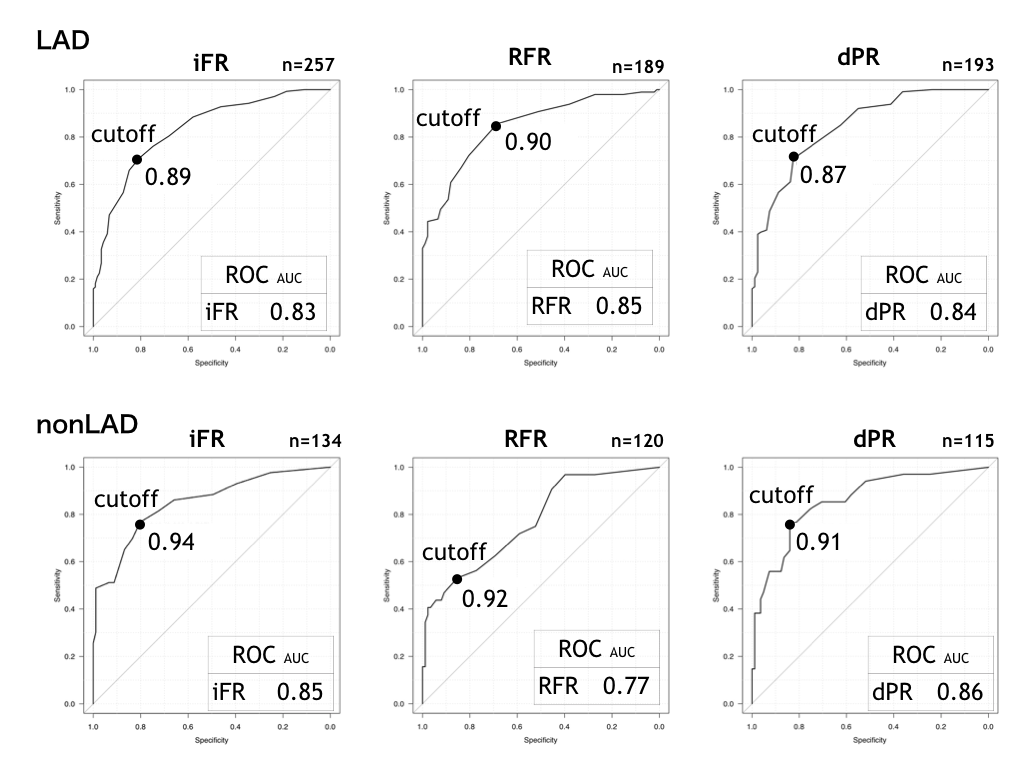
A total of consecutive 1008 lesions (iFR, n=391;RFR, n=309; dPR, n=308) was enrolled retrospectively, who underwent both FFR and resting index due to stable angina pectoris during September 2014 to October 2020. We assessed correlation coefficient and the area under the receiver operating characteristic curve by comparing each resting index (iFR, RFR and dPR) to FFR.
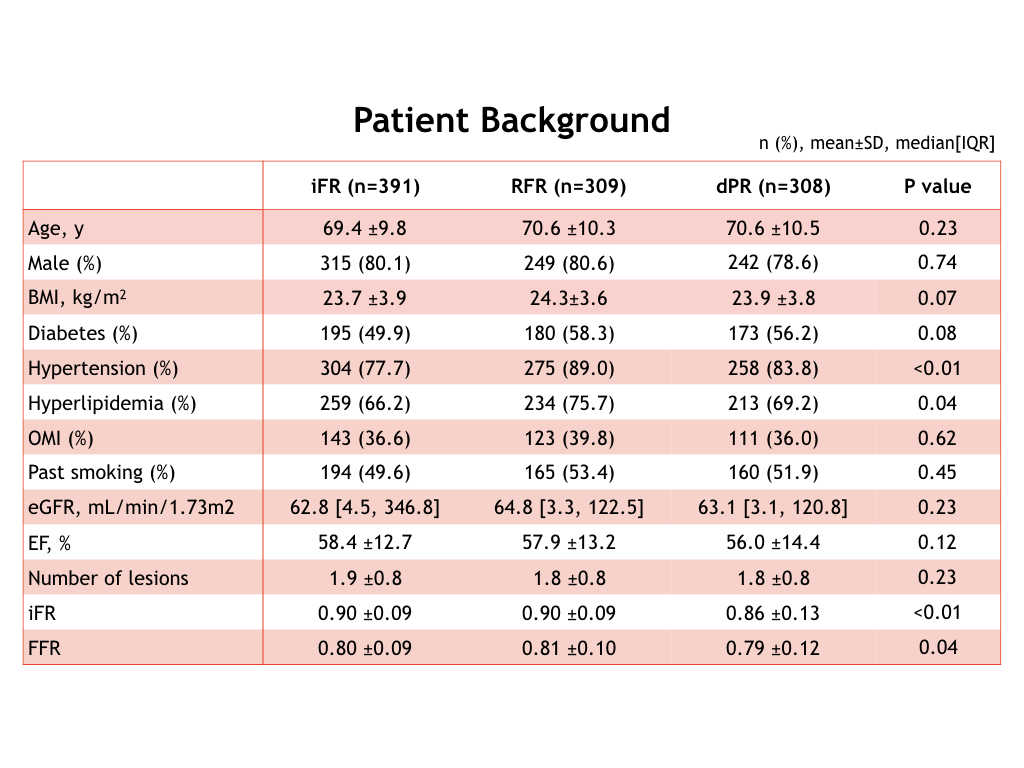
Results
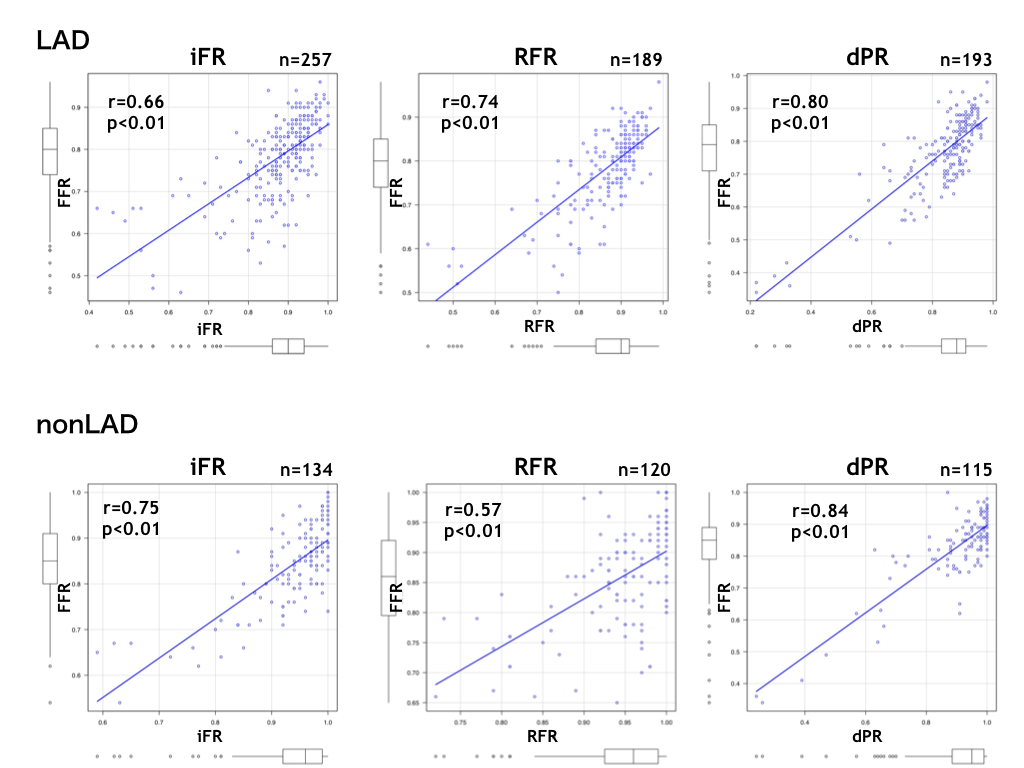
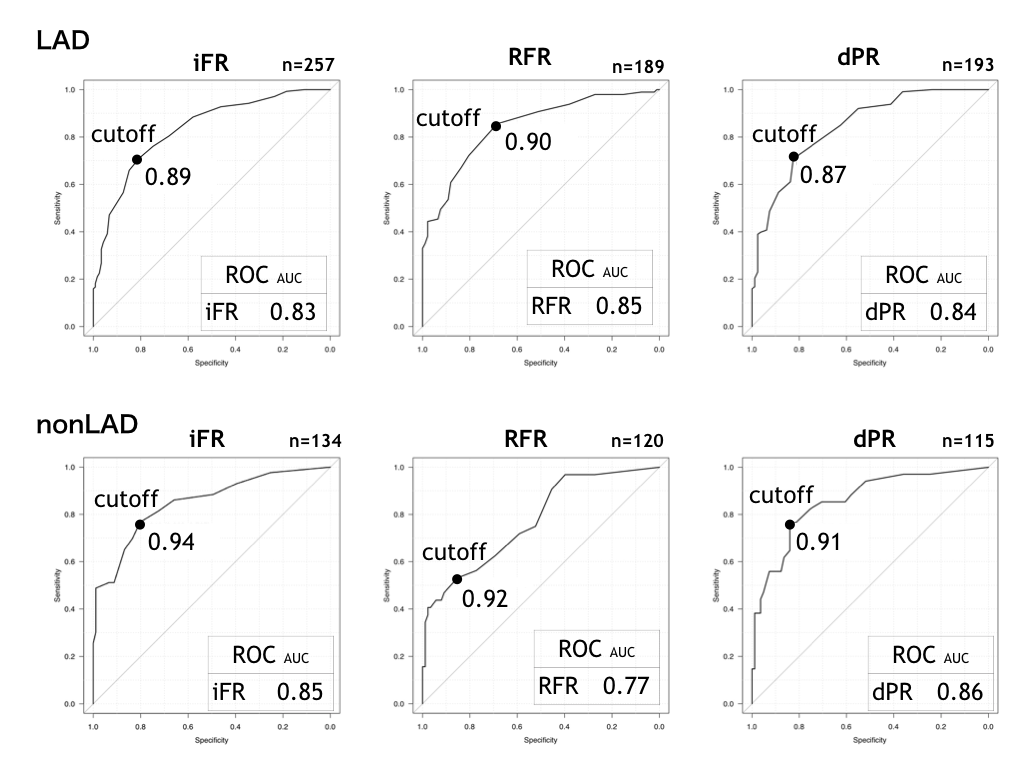
dPR showed a stronger correlation with FFR in LAD lesion (iFR-FFR, r=0.66 vs. RFR-FFR, r= 0.74 vs. dPR-FFR, r= 0.80). RFR showed a weaker correlation with FFR in nonLAD (iFR-FFR, r= 0.75 vs. RFR-FFR, r= 0.57 vs. dPR-FFR, r= 0.84).
Conclusion
dPR had better correlation with FFR in every lesion. Each resting index had a different cut-off value for FFR, moreover, RFR had low accuracy with FFR in nonLAD. This might be derived from the differences of calibration methods and calculation algorithms in themselves.