Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP A-005
Presenter
Tianyu Li
Authors
Tianyu Li1, Jinqing Yuan1
Affiliation
Fuwai Hospital, China1
View Study Report
TCTAP A-005
Acute Coronary Syndromes (STEMI, NSTE-ACS)
Effects of Age and Sex on Outcomes After Percutaneous Coronary Intervention or Coronary Artery Bypass Grafting in Non-ST-Segment Elevation Acute Coronary Syndrome Patients with Triple-vessel Disease
Tianyu Li1, Jinqing Yuan1
Fuwai Hospital, China1
Background
Age-and sex-specific considerations are required for the choice of revascularization strategies in patients presenting with non-ST-segment elevation acute coronary syndrome (NSTE-ACS) and triple-vessel disease (TVD). We aimed to explore the effects of age and sex on outcomes after percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) in NSTE-ACS patients with TVD.
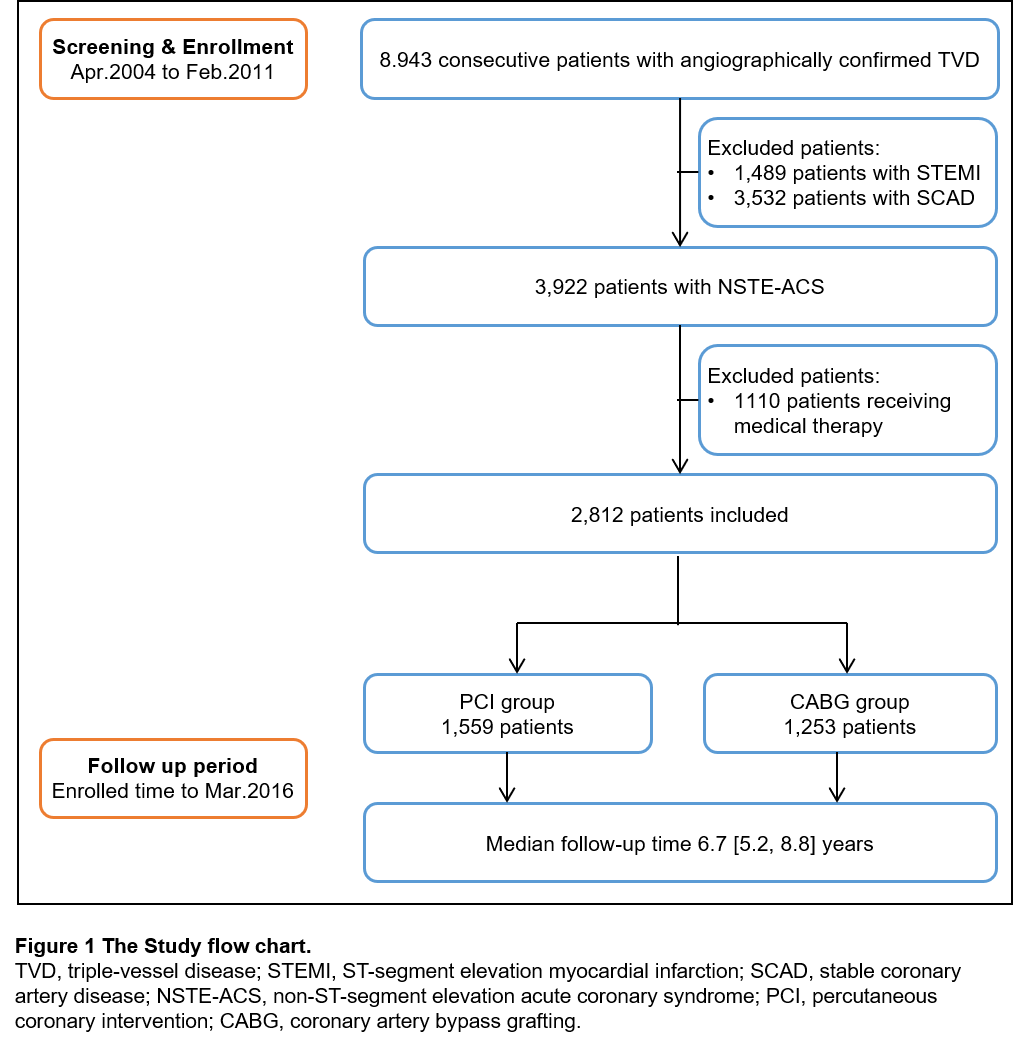
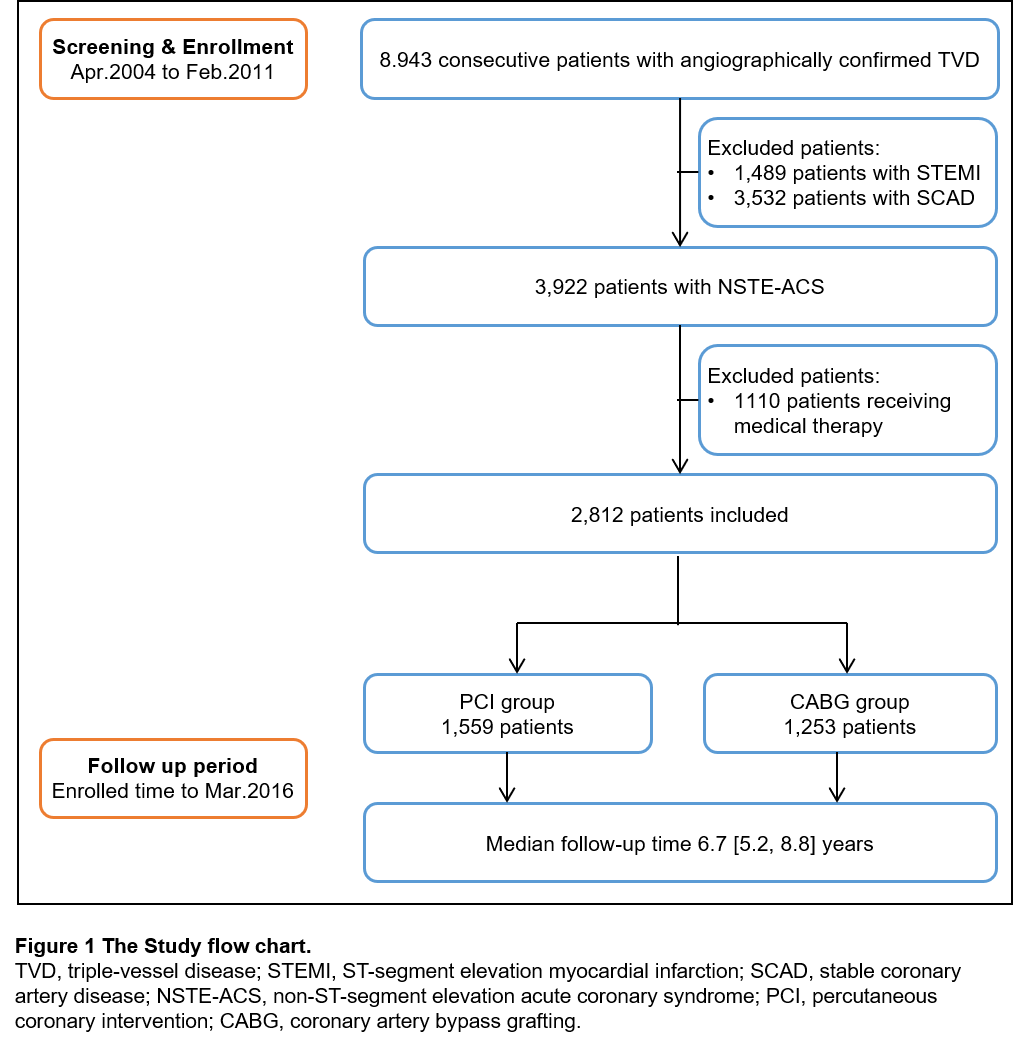
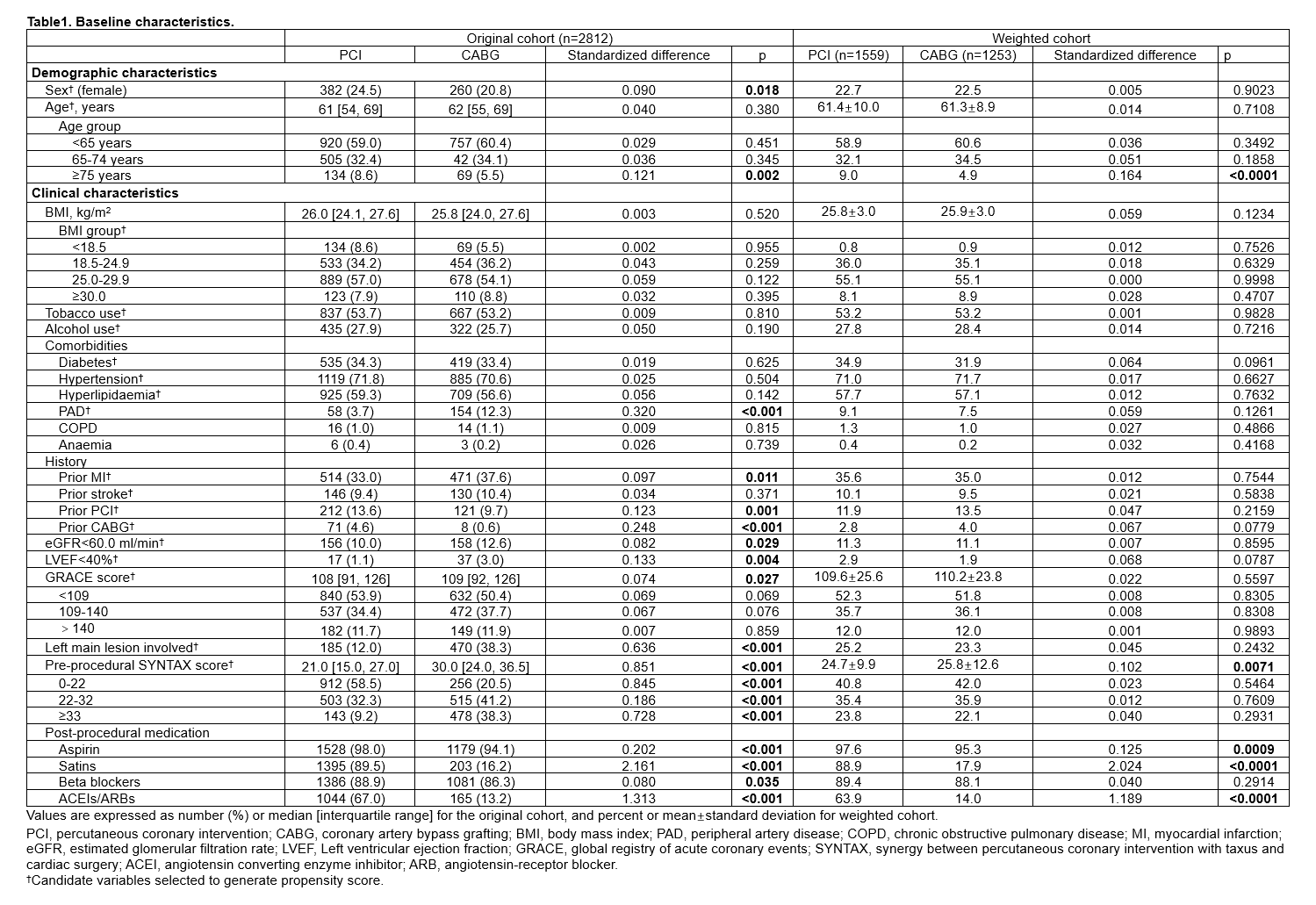
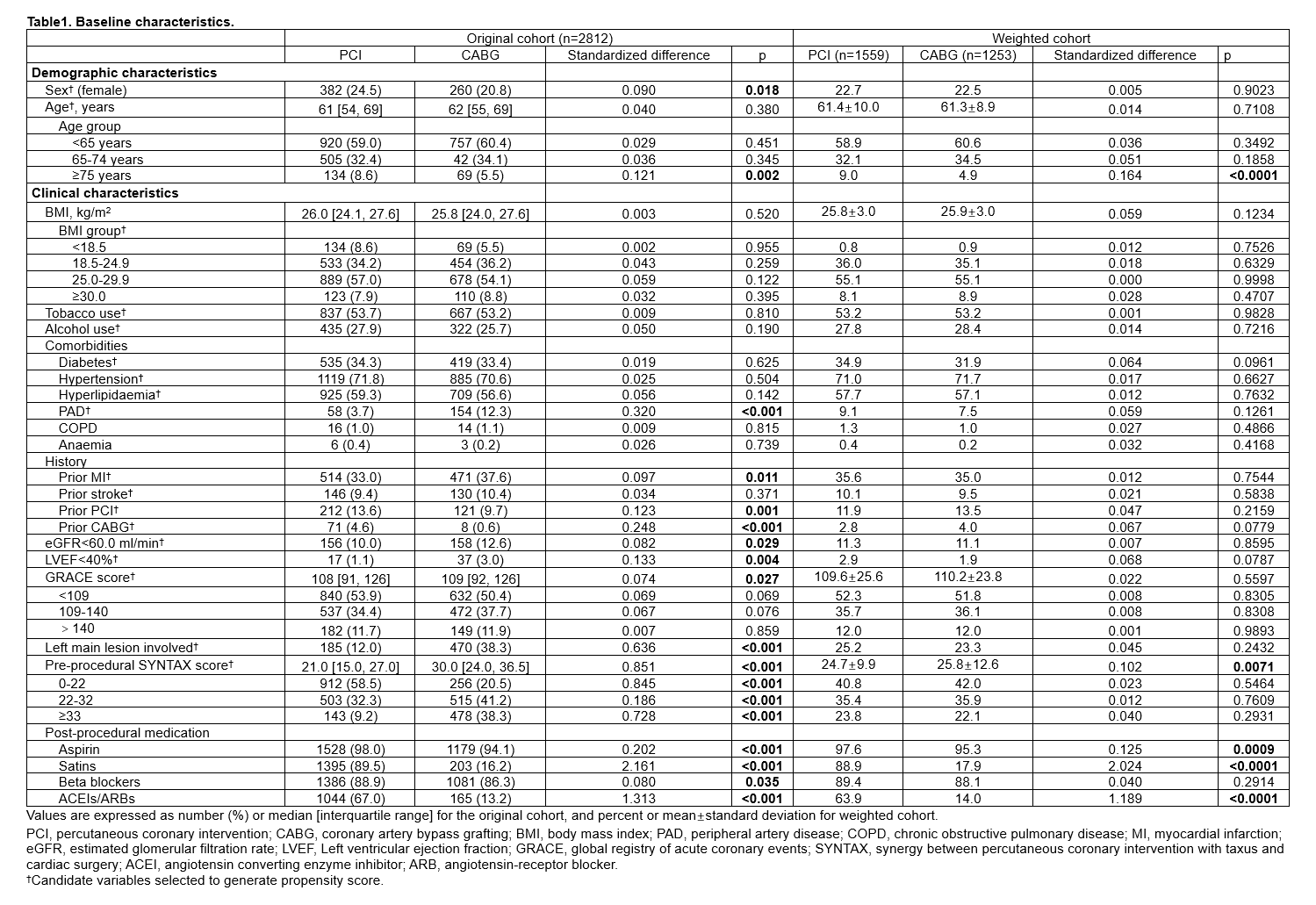
Methods
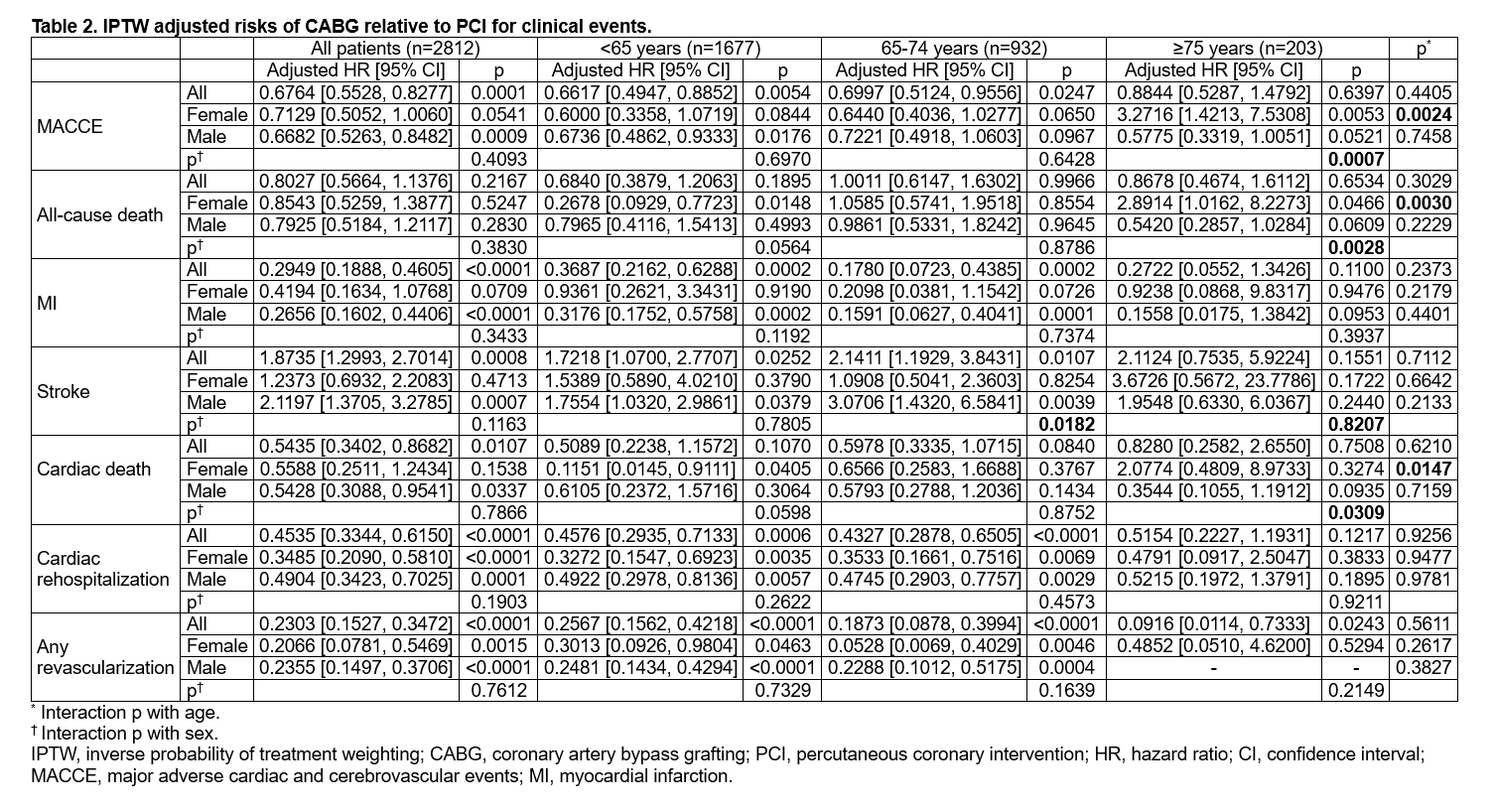
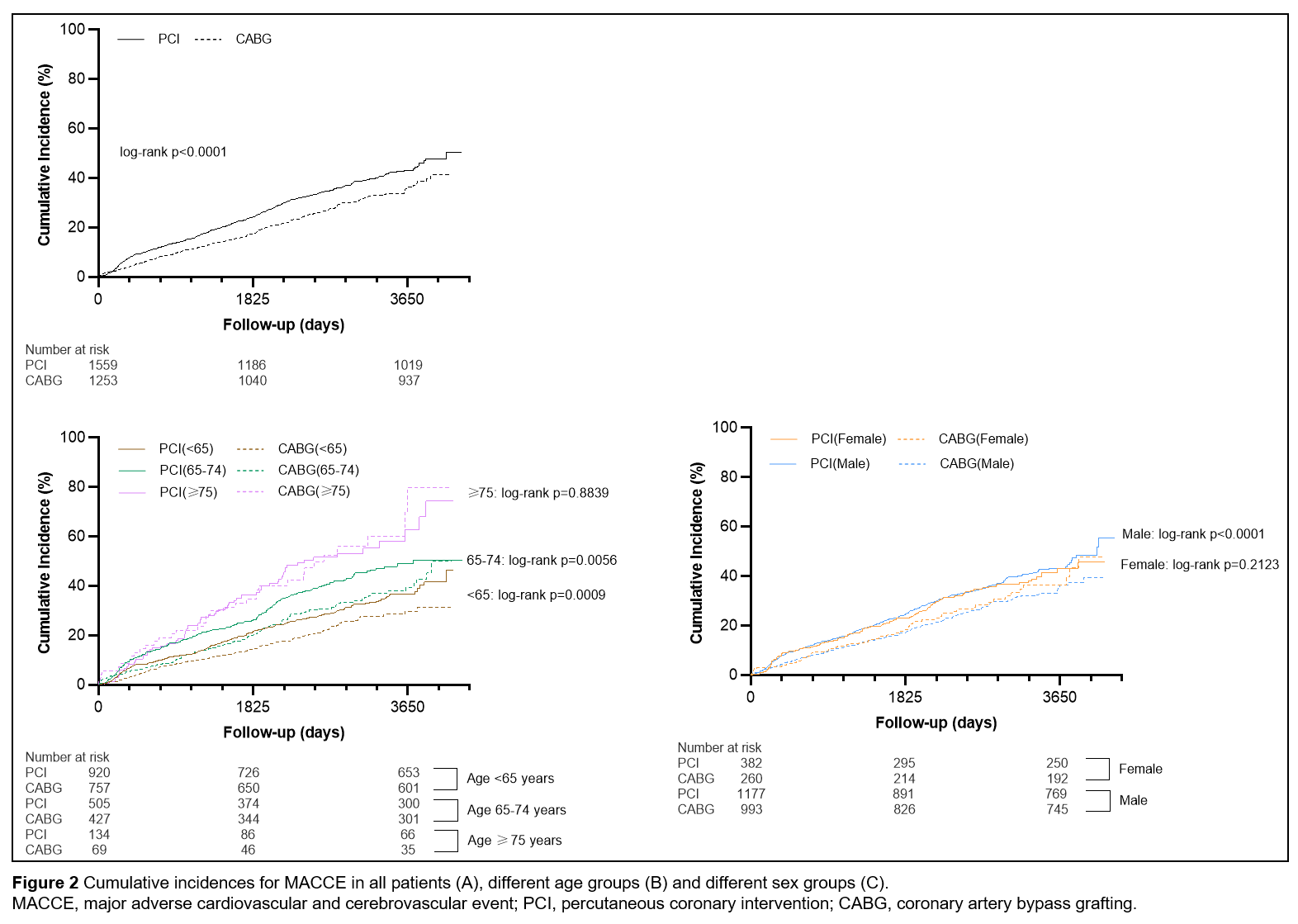
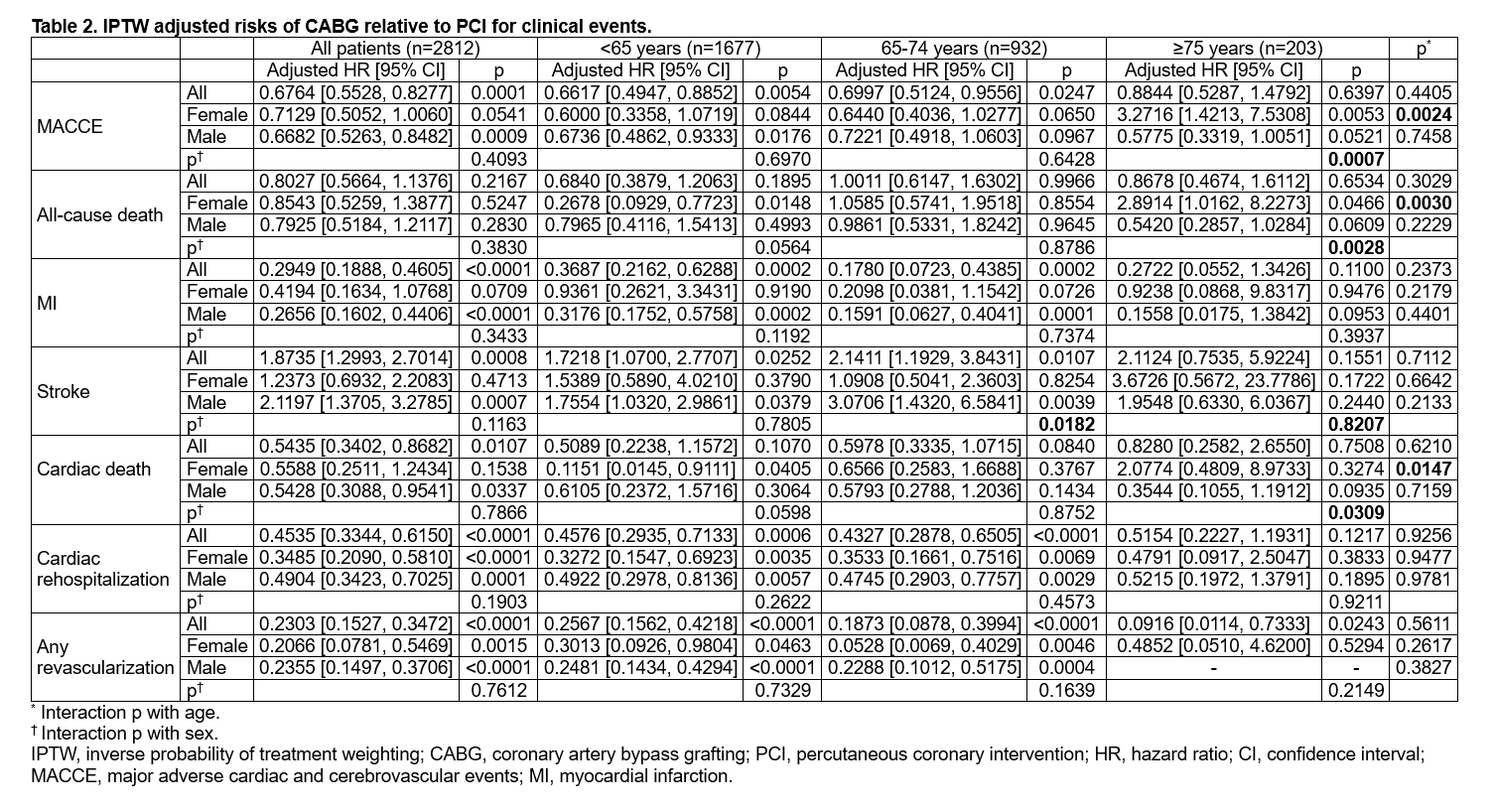
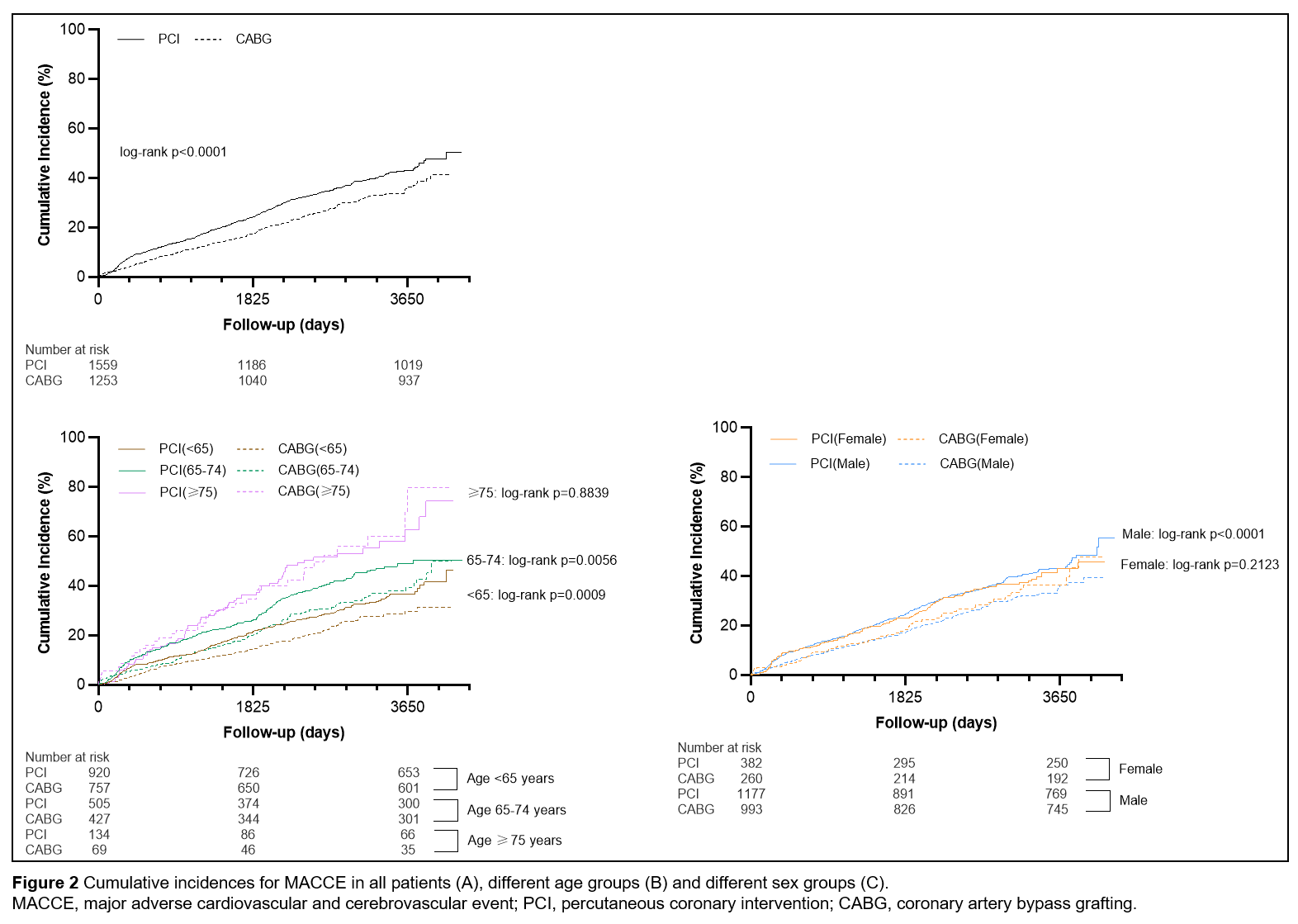
A total of 2,812 patients (22.8% women and 77.2% men) with NSTE-ACS and TVD who received coronary revascularization (PCI, n = 1,559; CABG, n = 1,253) were included in the present study. Patients were divided into three age groups: < 65, 65 to 74, and ≥ 75 years. The primary endpoint was major adverse cardiac and cerebrovascular events (MACCE), consisting of death, myocardial infarction and stroke. Other endpoints included cardiac death, cardiac rehospitalization and any revascularization. The adjusted hazard ratios (HRs) with 95% confidence intervals (CIs) were estimated using inverse probability of treatment weighting based on propensity scores.
Results
During a median follow-up of 6.7 years, the risk of MACCE after CABG was significantly higher than after PCI in women ≥ 75 years of age (HR = 3.2716, 95% CI: 1.4213 - 7.5308), whereas the risks were trended to be significantly lower after CABG than after PCI in men ≥ 75 years of age (HR = 0.5775, 95% CI: 0.3319 - 1.0051; interaction p for sex = 0.0007), women < 65 years of age (HR = 0.6000, 95% CI: 0.3358 - 1.0719) and women 66 to 74 years of age (HR = 0.6440, 95% CI: 0.4036 - 1.0277; interaction p for age = 0.00024). Compared with PCI, CABG was associated with significantly lower risks of MACCE in men of other two age groups. No significant interaction between age and revascularization strategies in men was observed, neither was it between sex and revascularization strategies in other two age groups.
Conclusion
Although CABG might be superior to PCI in terms of MACCE in most NSTE-ACS patients with TVD, women ≥75 years of age undergoing CABG experienced a significantly higher risk of MACCE than those undergoing PCI.