Lots of interesting abstracts and cases were submitted for TCTAP 2021 Virtual. Below are accepted ones after thoroughly reviewed by our official reviewers. Don’t miss the opportunity to explore your knowledge and interact with authors as well as virtual participants by sharing your opinion!
TCTAP A-017
Presenter
Jianfeng Zheng
Authors
Jianfeng Zheng1, JiLin Zheng1, Xiaoying Lou2
Affiliation
Fuwai Hospital, China1, Cancer Hospital, China2
View Study Report
TCTAP A-017
Bifurcation/Left Main Diseases and Intervention
Long-term Outcomes of Percutaneous Coronary Intervention Versus Coronary Artery Bypass Surgery in Elderly Patients with Multivessel and/or Left Main Coronary Artery Disease and Diabetes Mellitus: A Systematic Review and Meta-analysis
Jianfeng Zheng1, JiLin Zheng1, Xiaoying Lou2
Fuwai Hospital, China1, Cancer Hospital, China2
Background
This meta-analysis was performed to compare two methods of superior revascularization strategies coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) in patients with multivessel and/or left main coronary artery disease for elderly patients diabetes mellitus.
Methods
An electronic search of recent studies (2009–2019) was carried out using “diabetes mellitus”, “coronary artery bypass surgery”, and “percutaneous coronary intervention” as the main search terms. Stata software (version 15.0) was used to calculate relative risk (RR) and 95% confidence intervals (CIs).
Results
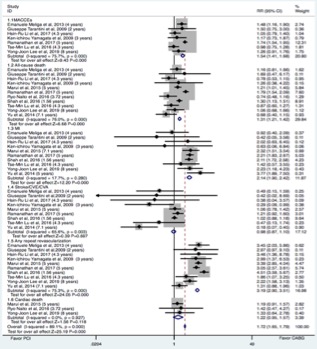
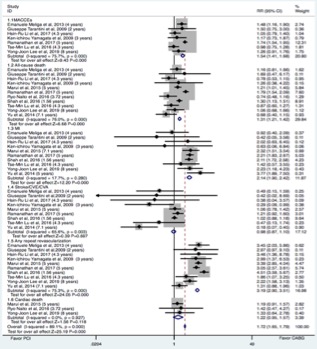
Among those observational studies, PCI and CABG patients did not differ significantly in their rates of stroke/cerebrovascular events(CVE)/cerebrovascular accident(CVA) (RR 0.98 95% CI 0.87-1.10;P=0.697 ) and cardiac death (RR 1.22 95% CI 0.95-1.57;P=0.118 ). However, rates of major adverse of cardiac and cerebral events(MACCEs), all-cause death, myocardial infraction(MI) and any repeat revascularization were significantly higher in the PCI group. Although there was no significant difference of MI (RR 1.26 95% CI 0.90-1.77;P=0.173) and stroke/CVE/CVA (RR 0.52 95% CI 0.26-1.03;P=0.061) among those RCT studies, the CABG significantly had lower all-cause death, cardiac death and any repeat revascularization.


Conclusion
Despite the high potential risk of stroke/CVE/CVA, CABG was better than PCI for diabetic elderly patients with multivessel and/or left main coronary artery disease in clinical practice.